
Technology’s influence has reshaped nearly every aspect of modern life, and its application in public health is now moving beyond the clinic and into the heart of our neighborhoods. As communities grapple with increasing behavioral health challenges from the persistent crisis of loneliness to the need for accessible, preventative care, the traditional models of support are showing their strain. Community-based organizations (CBOs), the essential front lines of wellness, are often hampered by fragmented systems, manual processes, and an inability to clearly measure their profound impact. This is where innovation steps in. This blog explores how leveraging modern technology is not just an option, but a critical necessity for scaling effective, holistic community wellness initiatives. It’s time to move past siloed support and embrace a unified, tech-enabled strategy to build truly connected, resilient, and healthy communities.
The community wellness imperative: bridging the gap in behavioral health
Community wellness has become a central pillar of public health strategy, especially as behavioral health challenges become more visible and more urgent. Across the country, community-based organizations are struggling to meet the rising demand for support while navigating limited budgets, outdated systems, and complex compliance requirements. The end goal is no longer just to treat illness but to build connected, resilient communities that promote mental and physical well-being. To do this, first we must address:
The crisis of disconnection
Behavioral health cannot thrive in isolation. Many people experiencing mental health or substance-use issues never set foot in a clinic, relying instead on schools, local nonprofits, and peer-led programs. Yet these community touchpoints often operate in silos. Fragmented data, disconnected workflows, and inconsistent communication create barriers that leave individuals slipping through the cracks. In an era where loneliness and social disconnection have been declared public health crises, the need for integrated community-level mental health support is non-negotiable.
The behavioral health lens
True wellness requires a holistic approach. Treating behavioral and physical health separately fails to address the interconnected nature of people’s lives. Community-centric wellness programs look beyond diagnoses, focusing instead on social determinants such as housing, employment, and family dynamics. This model shifts care from being episodic to continuous, where prevention and engagement matter as much as treatment.
Challenges to scale
Even when programs succeed locally, scaling them is difficult. Community organizations often face three core barriers. The first is fragmented data (behavioral health, school counseling, and social service records rarely integrate). The second is manual or paper-based workflows, which slow response times and make tracking progress nearly impossible. The third is measurement; because many CBOs struggle to demonstrate outcomes or return on investment to funders. Without that proof, sustaining grants and contracts becomes an uphill battle.
5 essential technology capabilities for community wellness programs
Technology has the power to remove many of these barriers if it is designed for community settings rather than hospital systems. Five capabilities are especially critical.

- Mobile-friendly engagement tools allow field workers, case managers, and peer counselors to stay connected in real time. Whether recording a visit, updating care notes, or checking in with a client, mobile access keeps data flowing and reduces lag between fieldwork and follow-up.
- Unified care coordination and referral tracking ensure no individual gets lost between services. A shared platform lets counselors, social workers, and partner agencies see the same care plan and track whether referrals to housing, food assistance, or behavioral therapy have been completed.
- Built-in behavioral screening and assessment tools make it possible to identify needs early. Standardized tools such as PHQ-9 or GAD-7 can be embedded into intake forms, school health screenings, and community events, generating data that supports early intervention.
- Data dashboards for outcomes and compliance transform how CBOs communicate value. With visualized metrics on engagement, attendance, and improvement, organizations can meet funder reporting requirements and make stronger cases for continued support.
- Finally, AI and automation can ease administrative burdens. From auto-filled documentation to follow-up reminders, automation reduces time spent on clerical work and lets staff focus on personal connection, a.k.a the heart of community wellness. Remote patient monitoring and digital engagement tools extend that connection further, allowing ongoing check-ins and wellness tracking outside clinic walls.
Optimizing community initiatives with advanced behavioral health EHR tools
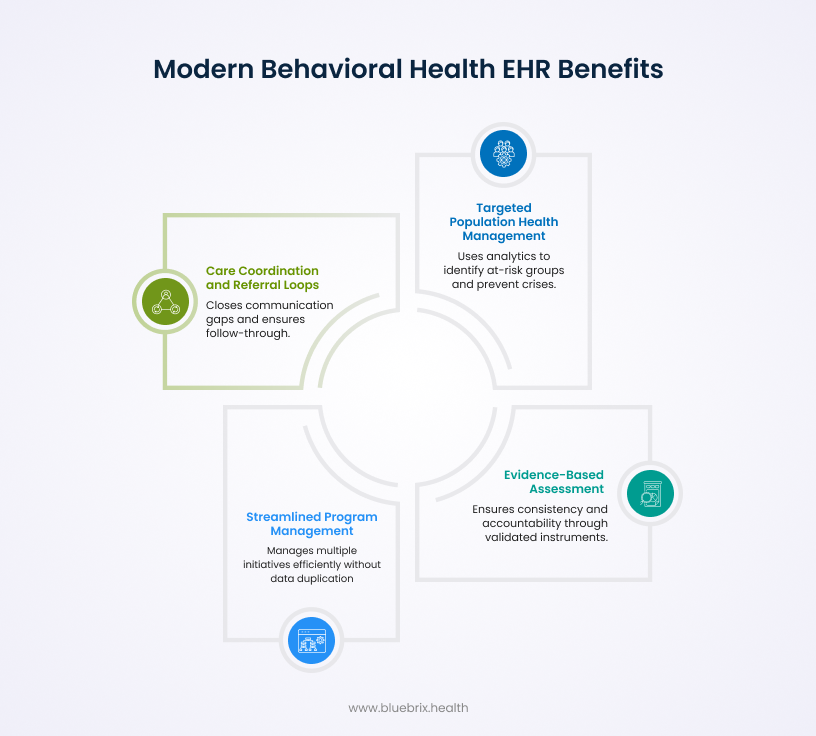
A modern behavioral health EHR, built with community programs in mind, transforms wellness initiatives from reactive to preventive. Targeted population health management uses analytics to identify at-risk groups; for instance, youth showing early signs of anxiety or seniors isolated after hospital discharge. Predictive analytics, such as those used in our blueBriX platforms, can flag risk trends before crises occur, helping organizations intervene early.
Evidence-based assessment and tracking tools bring structure and accountability to community work. Embedding validated instruments like PHQ-9, GAD-7, and CRAFFT into digital workflows ensures consistency across programs and supports longitudinal outcome measurement.
Streamlined group and program management is another key advantage. Many CBOs run multiple initiatives (group therapy, youth mentorship, peer-support networks), all with overlapping participants. Advanced systems can manage attendance, progress, and outcomes across these programs without duplicating data entry.
Lastly, care coordination and referral loops close the communication gap between organizations. Automated messaging and referral tracking ensure that when a patient is connected to a partner service, follow-through is documented and outcomes are visible. This is where technology turns collaboration into measurable impact.
Why a purpose-built behavioral health EHR is the missing link
Not all electronic health record systems are created equal. Generic medical EHRs, built for hospital workflows, often fail in community settings. They lack fields for group therapy notes, peer tracking, and social determinant data. A purpose-built behavioral health EHR is tailored to these realities, offering flexibility for multi-program enrollment, outreach documentation, and grant reporting.
For example, tracking a single individual who attends both a family counseling group and a substance-use recovery program can be complex. A community-driven platform simplifies this by linking all records to one profile, ensuring continuity while maintaining privacy under rules like 42 CFR Part 2.
Purpose-built systems also include built-in tools for compliance, such as CCBHC reporting templates and audit trails. This minimizes the administrative overhead that often overwhelms smaller organizations and allows them to stay focused on outcomes rather than paperwork.
The future is automated: reducing burden, maximizing impact
Automation is reshaping community behavioral health. Intelligent workflows now handle documentation, scheduling, and even elements of clinical decision support. AI-assisted note generation and smart templates can cut documentation time dramatically, freeing clinicians and peer counselors to focus on human connection.
blueBriX’s AI-powered assistants, for instance, are designed to suggest next steps or highlight gaps in follow-up care based on prior encounters. By guiding documentation and providing contextual prompts, these tools help maintain quality while reducing burnout.
Automation also supports financial sustainability. Robust revenue-cycle management modules ensure accurate billing for community-based services and grant-funded programs. For organizations dependent on mixed funding streams, this accuracy can be the difference between expansion and contraction.
Finally, simplified compliance and reporting tools make regulatory complexity manageable. Automated data aggregation allows CBOs to generate required reports for CCBHC certification, Medicaid billing, or federal grants without spending hours compiling spreadsheets. The result is a system that supports both mission and sustainability.
Conclusion: empowering your community’s wellness strategy
Community wellness depends on connection, coordination, and data. Technology alone cannot build compassion, but it can remove the friction that prevents compassionate care from scaling. Purpose-built behavioral health systems give community programs the structure they need to grow while staying true to their mission.
The return on investment is tangible. Programs using integrated digital tools report improved outcomes, reduced staff burnout, and stronger engagement with funders and stakeholders. As automation and analytics mature, the next evolution of community wellness will be proactive, data-driven, and deeply human. For organizations ready to lead that evolution, the next step is clear: adopt technology built for your world, not borrowed from someone else’s.
Every day spent navigating paper files and siloed systems is a day your dedicated staff could have spent making meaningful connections. The cost of delay is measured not just in lost productivity, but in preventable human suffering and unfulfilled grants. Stop subsidizing inefficiency.