When healthcare organizations ask about offline capabilities, they’ve moved past “Should we go mobile?” to the critical question: “Which architecture actually serves our field workers, supports care coordination, and helps us succeed in value-based care?”
This guide helps healthcare leaders navigate that decision by comparing what matters most—not just technical features, but real business outcomes that affect your bottom line and your ability to coordinate care effectively.
Why this decision matters now
Healthcare is increasingly distributed. Accountable care organizations, home health agencies, community health programs, and mobile clinics operate in environments where connectivity cannot be assumed. Rural areas, patient homes, and underserved neighborhoods often lack reliable cellular or WiFi coverage.
The stakes are high: complete documentation during patient encounters improves data quality, supports better HEDIS performance, and directly impacts value-based care financial success. But cloud-dependent systems fail in low-connectivity environments, forcing providers to document from memory hours later—introducing errors, compromising accuracy, and extending work into evening and weekend hours.
The global mobile health market surging from $62.7 billion to a projected $158.3 billion by 2030 signals the importance of this decision. The architectural choice you make will shape your care coordination capabilities and competitive positioning for years.
Understanding the core difference
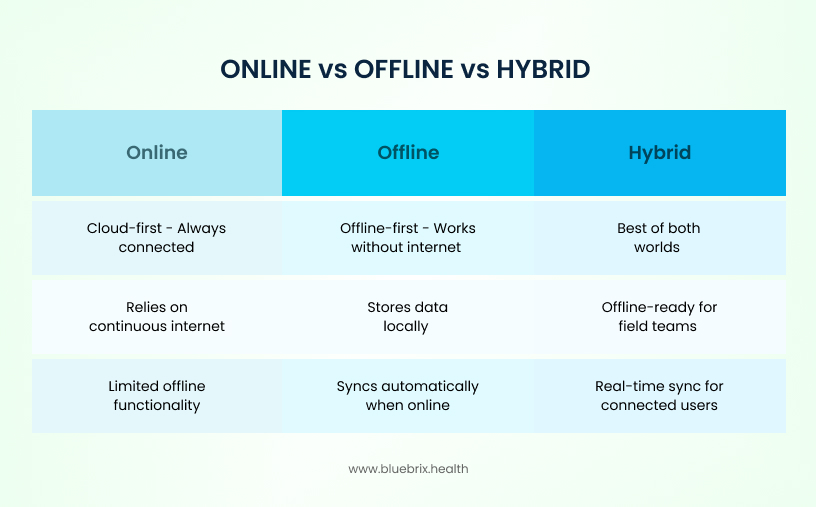
Offline-first architecture stores complete working datasets locally on mobile devices. Applications function fully without internet, treating server connection as a secondary enhancement. When connectivity resumes, the system synchronizes changes bidirectionally between device and servers.
Cloud-first architecture with limited offline assumes constant connectivity as the design foundation. The application may cache some data locally for read-only access during brief outages, but creates and updates typically require server communication. Full functionality degrades when connectivity fails.
Hybrid architecture combines offline-first capabilities for field workers with cloud-first real-time coordination for team members. This approach synchronizes data intelligently across multiple users, allowing both offline functionality and near-real-time updates when connectivity permits.
For healthcare, these distinctions shape how work actually happens: offline-first workers can document anywhere, cloud-first workers depend on networks, and hybrid approaches provide flexibility across both scenarios.
Where each approach excels
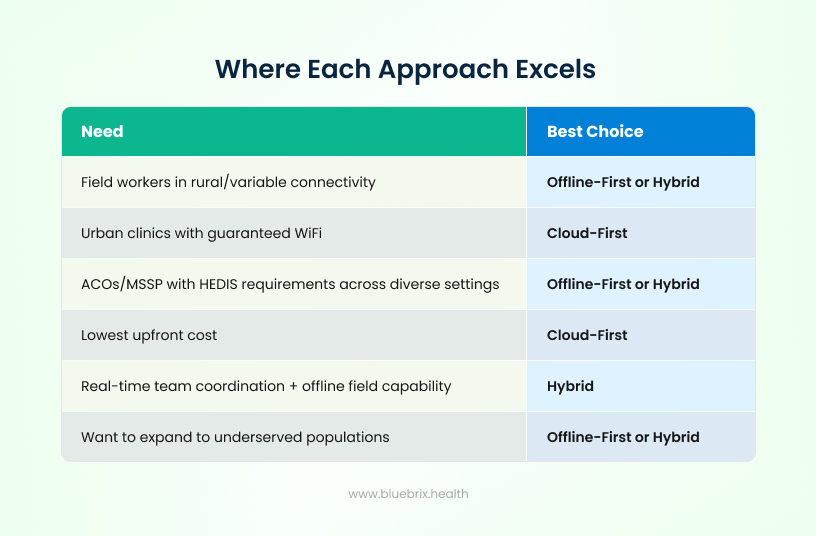
Offline-first works best when:
- Your field workers operate in variable connectivity environments—home health visits, rural clinics, mobile health programs, community screenings in underserved areas. The instant responsiveness of local processing improves user experience compared to cloud-dependent systems waiting for network roundtrips.
- You’re managing HEDIS quality measures and value-based care arrangements requiring comprehensive documentation. Real-time documentation during patient encounters captures details accurately, improving data quality and quality metric performance.
- You want to reduce provider burnout by eliminating evening documentation. Offline-first applications eliminate the documentation catch-up work that forces providers to complete charting as homework after clinical shifts.
- You need to expand services to underserved populations where infrastructure limitations make cloud-dependent systems impractical.
Cloud-first works best when:
- All care coordination occurs within facilities – hospitals, urban clinics, specialty practices – maintaining robust WiFi infrastructure.
- You require real-time data visibility where all team members work against synchronized server-side databases.
- Your development budget is tight. Cloud-first development typically costs 15-30% less than offline-first implementation because it avoids the complexity of synchronization logic and conflict resolution.
- Your application needs are primarily read-focused viewing cached information during brief connectivity interruptions.
Hybrid works best when:
- Your organization operates across mixed environments—some centralized clinic operations needing real-time coordination alongside field workers in variable connectivity settings. You want both offline functionality and real-time data visibility without compromising either.
- You need to balance development complexity and cost against operational requirements. Hybrid approaches allow phased implementation—starting with cloud-first infrastructure and adding offline capabilities to specific workflows or user roles.
- You want flexible escalation—enabling offline-first capabilities when field workers are deployed, then shifting to cloud-first emphasis when operations become more centralized.
- Your team needs a technology that gracefully handles mixed connectivity scenarios within the same application—some users online and some offline simultaneously, all working against synchronized data.
The business impact: what changes
Productivity and time management
Healthcare faces critical workforce shortages. The biggest driver? After-hours administrative work. Offline/Hybrid apps eliminate evening documentation because providers complete charts during patient visits. Cloud-first apps force evening catch-up when connectivity fails in the field. Offline-first and hybrid become retention tools.
Hybrid approaches benefit field workers while maintaining real-time coordination visibility for care team members in connected environments. Central care coordinators see updates immediately when field workers resynchronize, supporting faster clinical decision-making than pure offline-first deployments.
Data quality and compliance
Real-time documentation captures details accurately while fresh in the provider’s mind. Home health agencies improved from 45% same-day billing with cloud systems to 98% with offline-first.
Hybrid architectures add another layer: background synchronization can push critical updates (like new orders or test results) to field workers automatically when they reconnect, ensuring they have current information even if they were offline when decisions were made. This combines offline productivity with online data freshness.
Financial performance under value-based arrangements
Accountable care organizations depend on quality metrics like HEDIS measures to qualify for shared savings and avoid penalties. Offline-first and hybrid documentation’s support for comprehensive capture across all settings improves metric performance directly.
Hybrid approaches provide additional advantages: real-time sync means updated care plans, lab results, and quality interventions reach field workers promptly when they reconnect, reducing delays in clinical response. This supports better quality outcomes and improved financial performance under value-based arrangements.
Service area expansion
Offline-first architecture removes connectivity as a barrier to serving underserved populations. Rural mobile clinics reported 20% capacity increases after implementing offline-first technology, enabling five additional patients per clinic day—120 annual visits and $18,000 additional revenue per provider.
Hybrid deployments scale this further by allowing organizations to expand field operations while maintaining central visibility and control through real-time data sync when connectivity permits.
Technical considerations: architecture comparison
Offline-first architecture:
- Local data storage: All working data on device
- Synchronization: Bidirectional when connected
- Conflict resolution: Timestamp or version-based
- Development cost: Higher upfront
- Maintenance: Ongoing sync engine monitoring
- Security complexity: Encryption on distributed devices
- User experience: Consistent fast response regardless of connectivity
- Real-time visibility: Delayed until resync
Cloud-first architecture:
- Local data storage: Cached read-only data
- Synchronization: Always on, real-time
- Conflict resolution: Single source of truth
- Development cost: Lower upfront
- Maintenance: Primarily server-focused
- Security complexity: Centralized server security
- User experience: Depends on connectivity
- Real-time visibility: Immediate for all team members
Hybrid architecture (offline-first base + cloud sync):
- Local data storage: Complete working datasets on devices
- Synchronization: Intelligent background sync with server
- Conflict resolution: Smart merge with manual review option
- Development cost: Medium (higher than cloud-first, lower than managing two systems)
- Maintenance: Sync engine + server monitoring
- Security complexity: Distributed device + centralized server
- User experience: Consistent offline, near-real-time when online
- Real-time visibility: Near-real-time updates with background sync
Hybrid implementations use technologies like progressive web app background synchronization APIs or native mobile sync engines that persist data locally while automatically syncing changes when connectivity becomes available. This eliminates the either/or choice—field workers enjoy offline functionality while care teams receive updates that sync automatically in the background.
Comparing total cost of ownership
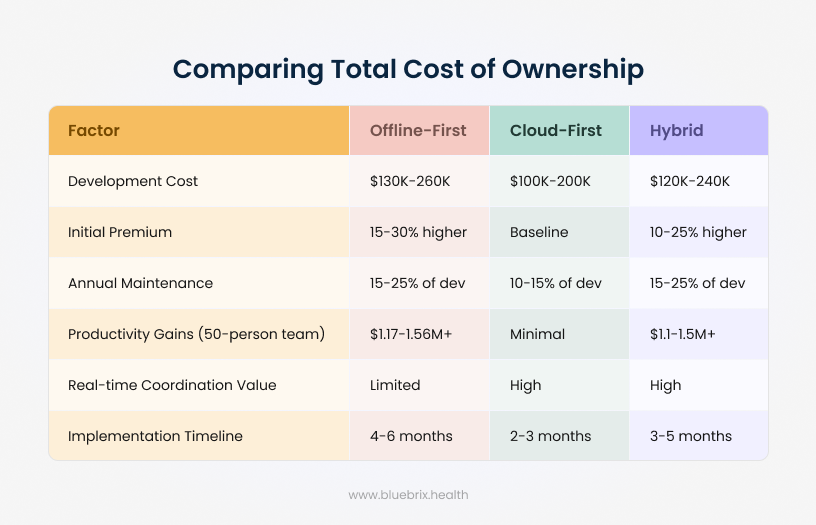
The Total Cost of Ownership comparison shows that Cloud-First architectures are the most cost-effective to develop and deploy, with lower initial and maintenance costs and faster implementation. However, Offline-First and Hybrid models, while 10–30% more expensive upfront, deliver significantly higher long-term productivity gains with over $1.1M annually for a 50-person team and maintain strong real-time coordination capabilities (in the case of Hybrid). Overall, organizations trade higher early investment in Offline-First or Hybrid systems for greater operational resilience and sustained efficiency.
For healthcare organizations with field workforces needing both offline capability and real-time coordination, hybrid approaches often represent the optimal cost-benefit balance. Development costs fall between pure offline-first and cloud-first approaches while capturing benefits of both.
The hybrid advantage (why most organizations should choose this)
Hybrid gives you:
- Field workers: Full offline functionality, no evening documentation homework
- Care coordinators: Automatic background sync—see field updates without workers needing constant connectivity
- Real-time coordination: Better than pure offline-first
- Cost efficiency: Development cost between pure offline-first and cloud-first
- Flexibility: Expand field operations while maintaining central coordination
When hybrid makes sense:
- You operate across mixed environments (some centralized clinics, some field-based care)
- You want offline reliability AND real-time team visibility
- You need to expand to underserved populations without sacrificing care coordination
- You want balanced cost vs. operational benefit
Practical decision framework
1. Map your care delivery footprint
Where does your organization deliver care? Urban clinic with robust WiFi? Rural home visits? Mobile clinics in underserved areas? Mixed environments?
If most care occurs in controlled environments with reliable connectivity, cloud-first suffices. If you deploy workers in variable connectivity, offline-first or hybrid becomes essential. If you operate across both scenarios, hybrid provides flexibility without forcing compromises.
2. Evaluate your value-based care model
Are you participating in ACO arrangements, MSSP programs, or other value-based contracts requiring comprehensive quality metric documentation?
Offline-first and hybrid architectures’ ability to capture complete data regardless of location directly improves HEDIS and other quality measures determining value-based care financial success.
3. Consider team coordination requirements
Do care coordinators need real-time visibility of field worker activities? Do field workers need immediate access to updated care plans and clinical orders?
Cloud-first provides immediate real-time visibility but fails when connectivity drops. Offshore-first ensures availability but delays team updates until resync. Hybrid provides both: field workers maintain offline functionality while background synchronization keeps care teams informed.
4. Assess workforce preferences
Engage field workers in the evaluation. Organizations universally report that workers prefer offline-first and hybrid solutions because they eliminate evening documentation work.
The retention and satisfaction implications carry financial weight given healthcare turnover costs.
5. Calculate return on investment
For organizations with 50+ field workers, productivity gains typically generate positive ROI within 12 months even with hybrid’s moderate development cost premium.
Hybrid approaches often optimize the ROI calculation by reducing development complexity compared to pure offline-first while delivering most core benefits.
Red flags & realities
Don’t choose cloud-first if:
- You have >20 field workers in variable connectivity environments
- You’re joining/operating ACO/MSSP requiring field-based quality metric capture
- Provider burnout is a retention concern
- You want to expand to rural/underserved populations
Don’t choose offline-first alone if:
- Real-time team coordination is operationally critical
- Most workers operate within connected facilities
- You have minimal field operations
Do choose hybrid if:
- You’re uncertain whether field or centralized operations will dominate
- You want flexibility to expand field programs without rearchitecting
- You need both offline reliability and real-time coordination

