Your CoCM registry says you’re screening 200 patients a month. Your billing data shows 80-100 active enrollments. Where are the other 100 going?
Your warm handoff completion rate is probably sitting somewhere around 40-50%, and it’s quietly killing your CoCM program. And if you’re using split EHR systems or relying on verbal handoffs between PCP visits, you’re probably closer to 30%.
You’ve got the BHCM. You’ve got the psychiatric consultant. You’re billing 99492 and 99493. On paper, you’re running Collaborative Care. But when you actually pull the registry numbers, only half the patients’ PCPs flag for behavioral health ever make it into active treatment. The rest? They’re lost in that gap between “Mrs. Rodriguez needs to see someone” and “Mrs. Rodriguez is enrolled in our CoCM caseload.”
You’re stuck between providers who say, “just make sure they connect” and finance asking, “why aren’t we billing more 99494s?” Neither gives you the workflow map to actually close the loop.
That gap used to be an internal problem. Now it’s about to become an external audit finding. The practices hitting 75-80% completion rates aren’t doing anything heroic. They’ve just stopped treating warm handoffs like a soft skill and started treating them like a designed workflow with failure points you can actually measure.
In this blog we will discuss what’s turning your warm handoffs cold, why 2026 makes fixing it non-negotiable, and the workflow redesign that gets completion rates above 75%.
The 2025 policy shift that changes everything
Three things happened in the first half of 2025 that fundamentally changed the game for behavioral health integration. If you haven’t connected these dots yet, you need to stop and pay attention:
First: On January 1st, CMS launched the Innovation in Behavioral Health Model across Michigan, New York, and South Carolina. By 2028, specialty behavioral health practices in these states get per-beneficiary-per-month payments specifically for care coordination and integration. Read that again: they’re paying for the coordination work, not just the visits. The catch? You need closed-loop referrals. You need documented transitions. You need proof that care was actually coordinated.
Second: The momentum around Medicaid CoCM coverage continues to accelerate. As of 2025, 36 states now cover Collaborative Care through Medicaid up from just a handful in 2020. The expansion is accelerating, which means more auditors are looking at whether you’re actually running true CoCM or just calling it that.
Third: The 2025 Behavioral Health Core Set measures are now mandatory. States must report on them. Which means payers are going to start asking you for that data. And “follow-up after ED visit for mental health” and “initiation and engagement of treatment” aren’t aspirational metrics anymore—they’re reportable requirements.
Which means, the paperwork warm handoff is dead! If your workflow is “PCP identifies depression, sends referral to BHCM via EMR task, BHCM calls patient later,” you’re not going to survive what’s coming. Because when the audit happens—not if, when—you won’t be able to show systematic transitions. You’ll show referrals that went nowhere.
Understanding three behavioral health integration models and their handoff requirements
Most practices implement “integrated behavioral health” without defining which model they’re actually operationalizing. This creates fundamental mismatches—CoCM billing codes applied to PCBH consultation workflows, or traditional co-location trying to support registry-based population management.
The handoff requirements differ fundamentally across three models:
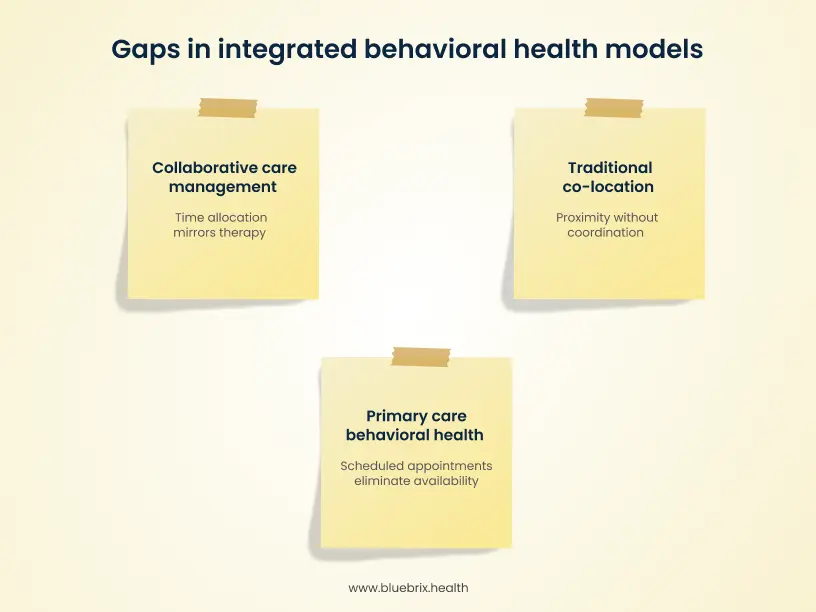
Traditional co-location model
Your BH provider operates independently with a traditional therapy schedule. Physical proximity doesn’t solve the problem: the provider is still booked 4-6 weeks out with 50-minute slots. When the PCP identifies acute need in Room 3, that 50-foot distance means nothing. The patient still gets “we’ll have someone call you to schedule.” The handoff is referral-based, similar to external specialty referral.
The common failure point: proximity without systematic coordination protocols.
Primary care behavioral health (PCBH) model
The BH consultant is embedded in primary care workflow for same-day consultations—brief 15-30 minute interventions focused on immediate problem-solving. The model requires protected capacity for unscheduled, PCP-initiated consults. The handoff looks like: “Let me grab our BHC to chat with you for 15 minutes right now about managing your anxiety.”
The failure point: when the BHC schedule fills with pre-scheduled appointments, eliminating drop-in availability. The model reverts to traditional referral patterns despite consultation-based design.
Collaborative care management (CoCM) model
The BHCM manages a patient caseload systematically via registry. The psychiatric consultant provides indirect oversight. The model depends on registry-driven population management with proactive outreach capacity. The handoff looks like: “I’m enrolling you in our depression treatment program. Our care manager will contact you within 24 hours to schedule your first session and explain how the program works.”
The failure point: BHCM time allocation mirrors traditional therapy (back-to-back patient sessions) rather than population management (20-30% time reserved for intake, consultation, registry review). This eliminates capacity for timely enrollment when PCPs identify treatment needs.
Root cause analysis: why systematic handoffs fail
Now that we’ve established which model you’re operating, let’s examine why handoffs fail regardless of model type. The root causes fall into five categories—each representing a failure point you can actually measure and fix:
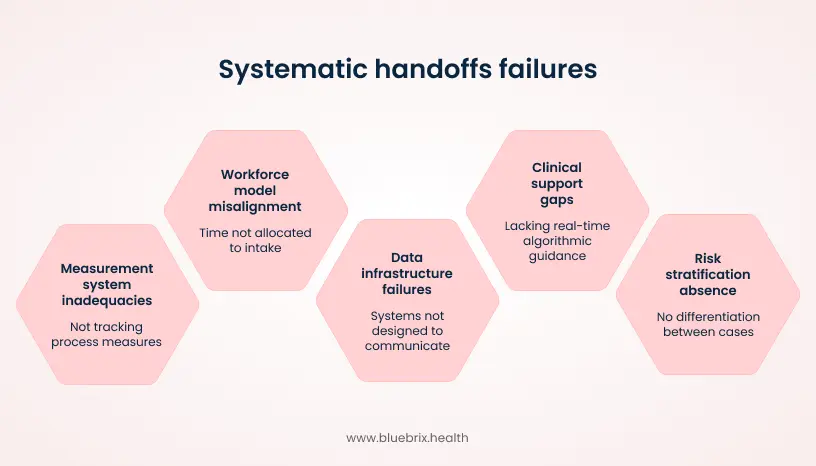
The absence of risk stratification at point of identification
Current workflows treat all positive behavioral health screens the same—no differentiation between mild and severe cases. A PHQ-9 of 11 gets the same handoff process as a PHQ-9 of 23 with suicidal ideation. EHR screening modules capture scores but don’t automatically stratify risk or trigger severity-based routing. The result: PCPs make ad-hoc judgments without decision support, and CoCM registries show no correlation between baseline severity and time-to-first-contact.
Clinical decision support gaps at identification point
PCPs lack real-time algorithmic guidance on which patients need immediate handoff versus routine scheduling versus external referral. EHR systems present screening scores as isolated data points, not integrated clinical decision pathways. There’s no automated guidance like “PHQ-9 = 18, item 9 endorsed: immediate safety assessment required” or “PHQ-9 = 12, prior failed SSRI: prioritize psychiatric consultation.” Hence, handoff decisions made without systematic consideration of clinical complexity, producing both over-referral and under-referral.
Data infrastructure and interoperability failures
Behavioral health transitions require data exchange across multiple systems not designed to communicate. This creates systematic information loss at every handoff point. The specific architectural failures:
Siloed screening data
PHQ-9 scores documented in primary care modules don’t automatically transfer to behavioral health intake documentation. BHCMs must manually locate prior scores or re-administer assessments, creating redundant data collection and patient frustration.
Medication reconciliation gaps
Primary care medication lists don’t sync in real-time with behavioral health documentation. BHCMs often cannot see recent medication changes made by PCPs, and PCPs cannot see medication recommendations from psychiatric consultants without manual chart review.
Registry population mechanisms
Most EHR-based registries require manual enrollment. When the PCP identifies need for CoCM, there’s no automated process to add the patient to the BHCM caseload, assign to psychiatric consultant review queue, or trigger baseline data compilation. Each step requires separate manual action.
Lack of standardized data exchange protocols
Even within single EHR platforms, primary care and behavioral health modules often operate as separate databases with minimal bidirectional data flow. HL7/FHIR integration for behavioral health data remains limited, and 42 CFR Part 2 consent requirements create additional data segmentation. Every handoff requires manual data assembly, with predictable information loss at each transition. The BHCM cannot access complete clinical context needed to start treatment, leading to delayed care initiation and repeated patient interviews covering information already documented.
Even when the data infrastructure is solid, handoffs still fail if the workforce model doesn’t support population health demands. Here’s the math problem most practices can’t see:
Workforce model misalignment with population health demands
Most practices structure BHCM time around traditional therapy scheduling—eight 50-minute sessions daily with 1.5 hours for everything else. When 15-20 PCP-identified patients need intake each week (requiring 11-15 hours of enrollment time), the math doesn’t work. The issue here is that practices can’t see this capacity mismatch in real-time. Without visibility into BHCM schedule utilization—percentage of time available for urgent intake versus blocked for scheduled sessions—leadership assumes the solution is hiring more staff rather than restructuring existing time.
CoCM requires 20-30% of BHCM time allocated to intake capacity and registry surveillance. Purpose-built platforms make this workforce allocation visible and measurable, flagging when schedule structure drifts away from population health requirements and making warm handoffs mathematically possible.
Measurement system inadequacies
Current measurement frameworks track volume (PHQ-9 screens administered, patients enrolled, billing codes) but not process measures that predict handoff success. What’s missing: completion rates (percentage of positive screens that result in successful handoff), transition lag (time from identification to first BHCM contact), failure point analysis (insurance issues versus patient disengagement versus scheduling barriers), and BHCM schedule utilization.
When completion rates sit at 40%, leadership can’t identify whether the problem is BHCM availability, patient engagement, administrative barriers, or referral quality. The result: practices invest in interventions—additional staffing, patient education, new EHR modules—without data showing those interventions target actual failure points.
Administrative barriers to warm handoffs: 5 process failures that block care
Beyond clinical workflow gaps, systematic handoff failures stem from administrative process deficiencies that create predictable barriers at every transition point. These aren’t clinical judgment failures—they’re structural process gaps that make successful handoffs mathematically unlikely:
Incomplete referral packets
CoCM enrollment requires specific documentation such as baseline PHQ-9 score, current medications, insurance eligibility, patient consent, ICD-10 diagnosis, and clinical indication. Most referrals are just an EHR task saying “Patient reports low mood, please evaluate for CoCM.” The BHCM can’t start treatment with incomplete information, so the referral bounces back to the PCP’s task queue—where it sits buried among dozens of other tasks. The patient waits without knowing why. High-performing systems use automated packet assembly that won’t let the handoff proceed until all required fields are completed—a hard stop, not a skippable checklist.
Insurance eligibility and prior authorization timing
Standard workflow verifies eligibility at appointment check-in, not at referral placement. Behavioral health coverage often has different rules than primary care—a patient eligible for a PCP visit may not be eligible for CoCM services. CoCM billing codes (99492, 99493, 99494) require prior authorization with many payers, taking 7-14 days for approval, but authorization denials often aren’t visible until claims are submitted 45-60 days post-service. The patients complete intake and begin treatment, then receive denial notices weeks later, undermining trust. High-performing systems trigger real-time eligibility checks at referral placement, flag payer-specific authorization requirements before patient contact, and initiate prior authorization immediately with status tracking visible to the care team.
Consent documentation and release of information
Behavioral health treatment requires multiple distinct consents such as BH treatment consent (separate from general medical), HIPAA authorization for BH information, 42 CFR Part 2 consent for substance use disorder information, release for PCP-BHCM communication, and psychiatric consultation consent.
Standard workflow provides paper forms at first appointment, but only 40% of patients arrive with completed consents. The consequence is that the first 15-20 minutes of a 30-minute intake appointment is consumed by paperwork instead of, or appointments get rescheduled because patients forgot reading glasses or need time to review. High-performing systems push digital consent forms to patient portal or mobile device immediately after referral placement, make appointment confirmation contingent on consent completion, and automate reminders for incomplete consents.
Structured handoff documentation
Current documentation: PCP progress note says “discussed behavioral health referral, patient agreeable” and sends a task with patient name and brief summary. What’s missing here are patient’s specific concerns about treatment, prior treatment attempts, treatment goals, barriers to engagement (transportation, work schedule, stigma), expected timeline, and context not in the chart (family dynamics, cultural considerations).
The result: BHCM starts first appointment without context, patient repeats information already shared with PCP, and opportunities to address barriers proactively are missed. High-performing systems use templated warm handoff documentation with required fields that auto-populate BHCM intake notes—data entered once by PCP flows directly to behavioral health record without manual transfer.
Failed handoff detection and escalation
When patients no-show for their first BHCM appointment, standard workflows leave them in “attempted contact, no response” status with no automated alert to the referring PCP. Failed transitions become invisible—PCPs assume patients are in treatment until they return months later with worsening symptoms.
High-performing systems trigger automated escalation protocols: same-day BHCM outreach, immediate PCP alert to re-engage, care coordinator follow-up within 48 hours, and after two failed attempts, psychiatric consultant review for alternative interventions. The system makes failed handoffs visible and actionable in real-time rather than allowing patients to disappear.
Infrastructure requirements for systematic transitions
We’ve identified what breaks. Now let’s examine what works. High-performing practices with handoff completion rates above 75% share common infrastructure characteristics that enforce systematic processes regardless of individual staff behavior. Here are the six critical components:
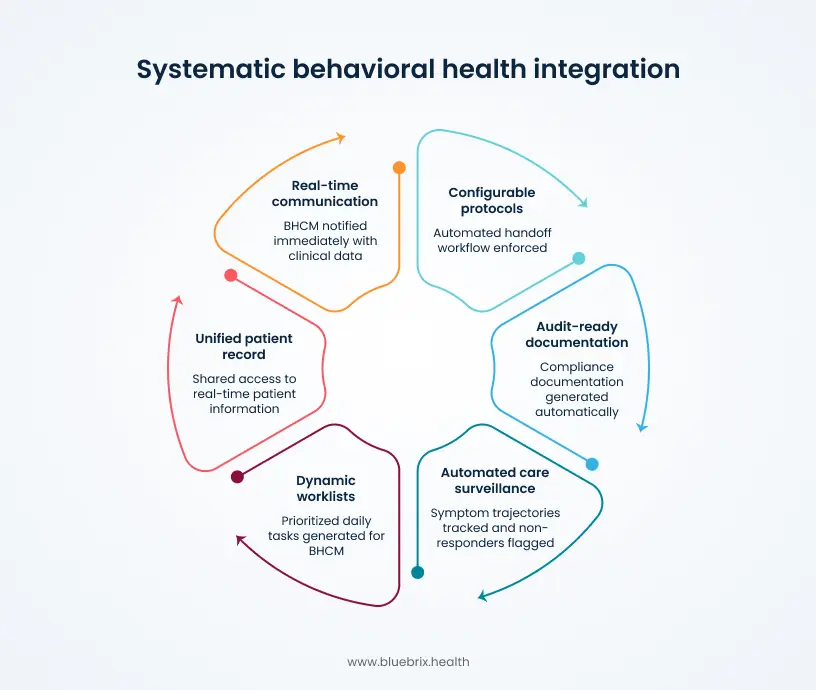
Real-time care team communication
When the PCP identifies a patient needing behavioral health intervention, the BHCM must be notified immediately—not when they next check their task queue. Context-aware clinical notification systems deliver alerts to BHCM devices with relevant clinical data (PHQ-9 score, presenting symptoms, current medications, urgency level) enabling immediate response. Response time drops from 45 minutes (asynchronous task) to under 5 minutes. If the BHCM cannot respond within defined timeframe, the system automatically escalates to backup protocol (care coordinator, psychiatric consultant, or scheduled intake within specified window).
Dynamic population health worklists
The registry must function as active management tool, not static report. Intelligent registries generate prioritized daily worklists—patients not contacted within defined timeframe (3-5 days), patients due for reassessment (6-8 weeks since last PHQ-9), patients showing treatment non-response (minimal score improvement after 6 weeks), yesterday’s no-shows requiring same-day outreach, patients flagged for psychiatric consultant review. BHCMs start each day with clear action lists rather than manually reviewing entire caseloads to determine who needs attention. Proactive outreach becomes systematic rather than dependent on clinical recall.
Configurable handoff protocols
The exact handoff workflow must be built into the platform, not dependent on individual staff adherence to training. Workflow automation enforces defined protocols—PCP flags patient for CoCM, system automatically checks insurance eligibility and prior authorization requirements, digital consent forms pushed to patient portal, BHCM notified with complete clinical packet, same-day or next-day appointment offered based on availability rules, patient receives automated confirmation with appointment details and program information, if patient no-shows automated outreach sequence initiates, if patient fails to engage after defined attempts escalation protocol triggers. Handoff steps occur systematically without requiring individual clinical judgment about “what comes next.” Staff time shifts from process management to clinical care.
Automated measurement-based care surveillance
The system must track symptom trajectories and flag non-responders without manual data compilation. Longitudinal symptom monitoring with algorithmic identification of treatment non-response—baseline and interval PHQ-9/GAD-7 scores graphed automatically, patients with less than 30% symptom improvement after 6-8 weeks auto-flagged for psychiatric consultant review, consultant reviews flagged patients with complete treatment history visible (medications tried, therapy modalities, adherence patterns, social determinants), consultant recommendations (medication adjustment, therapy intensification, different modality) automatically converted to PCP tasks. Psychiatric consultation time focuses on complex clinical decision-making rather than data gathering. Treatment adjustments occur systematically rather than dependent on BHCM recognizing stalled progress.
Unified patient record with role-based access
The PCP and BHCM must access same real-time patient information without manual data transfer or separate system logins. Single shared patient records with role-based access controls—PCP sees current BH treatment status, recent PHQ-9 scores, psychiatric consultant recommendations; BHCM sees current medications, recent lab results, upcoming PCP appointments, care plan for chronic conditions; updates are real-time with no batch processing or delayed synchronization; 42 CFR Part 2 compliance maintained through consent-based access controls. This eliminates scenarios where behavioral health treatment operates in parallel rather than integrating with whole-person care.
Audit-ready compliance documentation
Audit documentation must be generated as byproduct of normal workflow, not separate compliance activity. Time tracking automatically logs all CoCM activities (patient contact, care coordination, psychiatric consultation, registry review) against billing code requirements, consent documentation with timestamps showing when forms were sent, accessed, completed, prior authorization status tracking with audit trail, automated reports showing completion rates, time-to-engagement, measurement-based care adherence. When audit requests arrive, required documentation is generated with single report query rather than manual chart review of hundreds of patients.
You might be wondering: ‘Can’t our existing EHR do most of this?’ The short answer is no—and understanding why reveals the fundamental architectural mismatch between traditional health IT and behavioral health integration needs.
Why standard clinical workflows fall short for behavioral health integration
EHRs were architected for episodic visit-based care documentation, not population health management or real-time care coordination. The specific capability gaps:
Asynchronous task-based communication
EHR tasks are designed for “when you have time” workflow, not urgent clinical coordination. No capability for instant push notifications with clinical context. Cannot enforce response time requirements or escalation protocols.
Static registry reporting
Registry is database query result, not dynamic worklist. No automated patient prioritization based on risk algorithms. Cannot trigger proactive outreach based on time-since-contact or symptom trajectory.
Siloed clinical modules
Primary care and behavioral health documentation stored in separate databases. Bidirectional data flow requires custom integration work. Real-time visibility across modules not supported in standard configuration.
Manual workflow orchestration
Handoff protocols dependent on individual staff completing defined steps. No automated enforcement of workflow sequence. Process breakdowns invisible until patient fails to engage.
Limited measurement-based care tools
Symptom scores buried in encounter documentation. No longitudinal visualization or automated non-responder identification. Psychiatric consultation requires manual data compilation.
What purpose-built integration platforms provide
Platforms designed specifically for integrated behavioral health offer distinct architectural advantages:
Clinical notification engine
Delivers context-aware alerts in real-time to appropriate care team member based on defined protocols. Includes escalation logic for time-sensitive situations.
Intelligent registry
Sorts patients dynamically by AI-driven risk scores, days-since-contact, symptom trajectories. Auto-generates daily worklists for proactive care management.
Configurable workflow builder
Allows operational teams to define exact handoff protocols with automated enforcement. Hard stops prevent process steps from being skipped. Failed transitions trigger defined escalation sequences.
Unified patient view
Single real-time record accessible to entire care team with role-based permissions. Updates flow bidirectionally without manual data transfer.
Automated compliance tracking
Time logs, consent documentation, authorization status, and outcome measures captured as byproduct of clinical workflow. Audit reports generated on-demand.
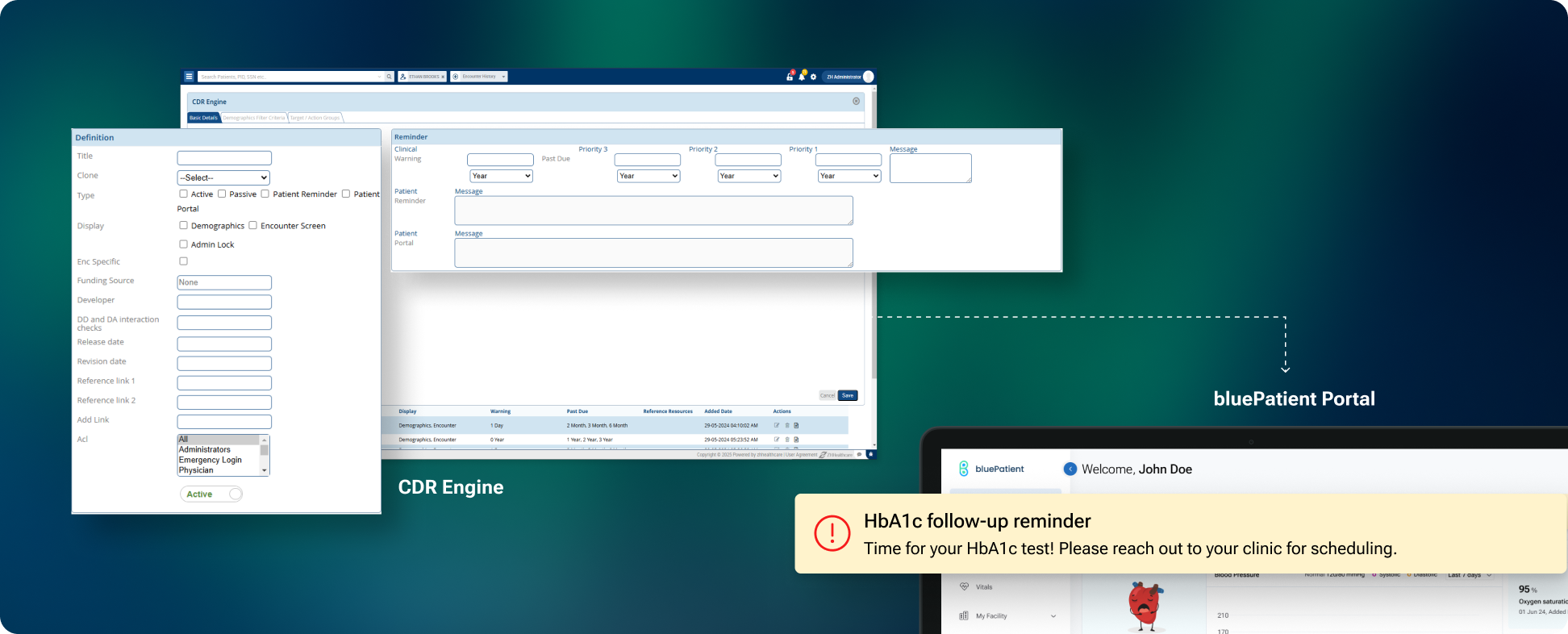
These aren’t theoretical capabilities. Purpose-built platforms like blueBriX operationalize these requirements into daily workflow. Here’s how the infrastructure translates into practice.
The blueBriX approach to handoff infrastructure
These infrastructure requirements aren’t theoretical. They translate into specific platform capabilities that make systematic handoffs operationally feasible. Here’s how the components work in practice:
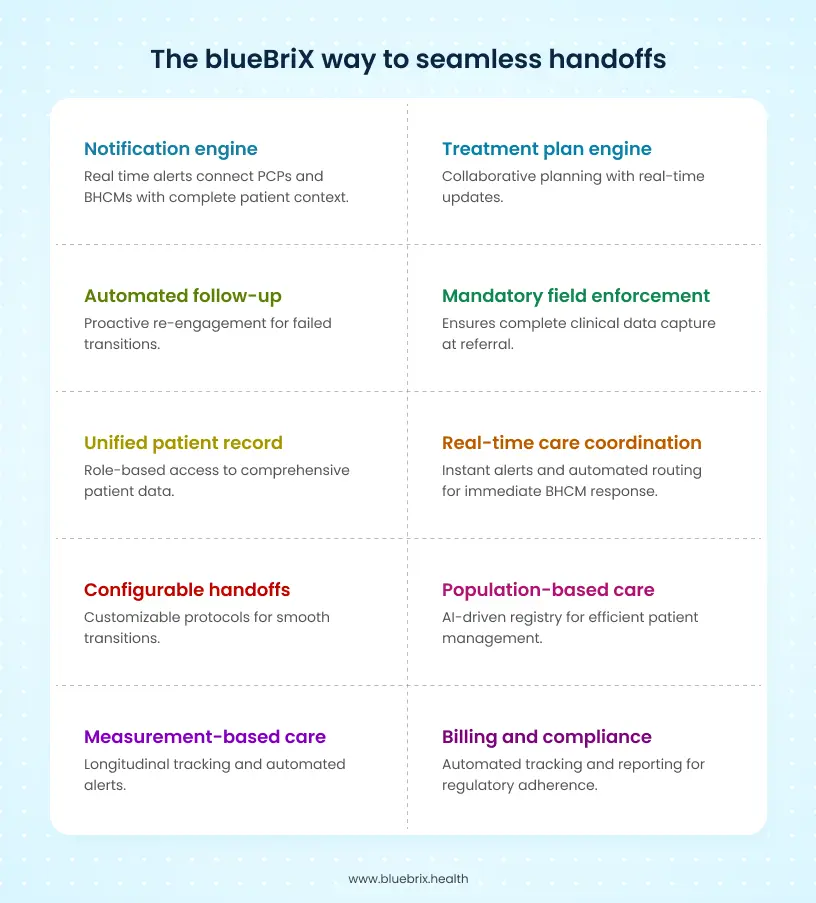
Real-time care coordination
Clinical notification engine delivers instant alerts to BHCM mobile device when PCP flags patient. Includes PHQ-9 score, presenting symptoms, medication list. BHCM can respond immediately or system auto-routes to next available resource.
Clinical notification engine
Delivers instant alerts to BHCM device when PCP flags patient, including PHQ-9 score, presenting symptoms, and medication list. BHCM can respond immediately or system auto-routes to next available resource if no response within a defined timeframe.
Mandatory field enforcement at referral
The platform allows practices to configure mandatory fields at the point of referral—ensuring baseline assessments, ICD-10 codes, and clinical indications are captured before handoff proceeds. This eliminates back-and-forth requests between providers for missing information and ensures complete clinical data is available from the start.
Population-based care infrastructure
Registry sorts caseload by AI risk scores and clinical priority. Morning dashboard auto-populates “no-show yesterday,” “due for reassessment,” “non-responder escalation” queues. BHCMs spend time on patient care rather than data organization.
Treatment plan engine with collaborative care coordination
Structured treatment planning tools enable BHCMs to create measurement-based care plans with specific interventions, target dates, and outcome goals. Plans are visible to entire care team in real-time. When psychiatric consultants make recommendations, they flow directly into the treatment plan with automatic task generation for PCPs—no manual transcription or separate communication needed.
Configurable warm handoff protocols
Low-code workflow builder lets teams define exact handoff rules. Example: PCP flags patient, system auto-checks insurance and prior auth requirements, pushes digital consents to patient portal, schedules same/next-day appointment, confirms attendance. For CoCM, enforces CMS-required packet (baseline scores, ICD-10 diagnosis, consent) as hard stop before BH intake proceeds.
Automated follow-up for failed transitions
No-show triggers three-attempt re-engagement protocol with PCP loop-back. The system makes failed transitions visible and actionable immediately rather than allowing patients to disappear.
Measurement-based care automation
Tracks PHQ-9/GAD-7 scores longitudinally with graphic visualization. Auto-flags non-responders (minimal improvement after 6-8 weeks) for psychiatric consultant review. Consultant recommendations instantly convert to PCP tasks—no spreadsheets, no manual tracking.
Role-based unified patient record
Single patient view with granular access controls tailored to each role. PCPs see latest BH notes and depression scores in real-time. BH team sees current medications and lab results without system switching. Care coordinators access scheduling and outreach history. Psychiatric consultants view symptom trajectories and treatment history. All updates live, all data secure under 42 CFR Part 2 encryption. Access permissions automatically adjust based on consent status.
Billing and compliance layer
Auto-tracks CoCM time against registry activity. Generates CMS-compliant reports for audits. Flags prior authorization needs. Monitors consent completion status. Practices see 25% revenue cycle improvement through reduced claim denials.