Pregnancy and the postpartum period represent critical phases where physiological and psychological changes converge. Hormonal shifts, neurobiological adaptations, and significant life transitions occur simultaneously, making integrated care essential. Yet most healthcare systems keep obstetric and behavioral health services separate, leaving patients to navigate fragmented care at precisely the time they need coordination most.
Without systemic involvement to coordinate these physiological and psychological needs, care gaps become inevitable. Two scenarios illustrate this challenge. In the first, an OB patient is diagnosed with a behavioral health condition during pregnancy and requires specialized mental health support. In the second, a behavioral health patient becomes pregnant and needs her existing treatment integrated with prenatal care. Both cases demand coordinated care between obstetric and behavioral health providers—yet most systems lack the infrastructure to deliver it.
In this blog, we’ll explore why perinatal behavioral health requires different clinical thinking, how these patients desperately need, and what successful integrated care models actually look like in practice.
Why the perinatal period demands different thinking
The perinatal window doesn’t play by normal rules. Biology shifts weekly. Symptoms that look benign can escalate in days. A mother’s mental health crisis becomes two patients’ emergency. Standard protocols fail here—not because providers aren’t skilled, but because the system wasn’t designed for this. Let’s deconstruct the current behavioral health landscape.
A unique clinical window
Pregnancy and postpartum represent one of the most dynamic phases in a woman’s life. Neurobiological changes aren’t subtle: fluctuating hormones, altered neurotransmitter systems, and structural brain adaptations create a window of both vulnerability and opportunity.
This is a heightened risk period for new-onset mental health conditions. Depression, anxiety, and even psychosis can emerge in patients with no prior psychiatric history. For those with pre-existing conditions, pregnancy often acts as a destabilizer—what was managed becomes unmanaged, sometimes rapidly.
What makes perinatal behavioral health fundamentally different: the stakes involve two patients. A mother’s mental health directly impacts fetal development, birth outcomes, infant attachment, and early childhood development. We’re not just treating symptoms; we’re influencing a critical developmental period for the next generation.
The complexity behavioral health providers face
Perinatal patients don’t fit neatly into standard workflows. Medication decisions become exponentially more complex: weighing risk-benefit of SSRIs during pregnancy, navigating breastfeeding while managing bipolar disorder. These conversations carry uncertainty and limited longitudinal data.
Medical complications intersect with mental health in ways we’re still understanding. Preeclampsia increases postpartum depression risk. Gestational diabetes correlates with anxiety. Preterm birth creates trauma that standard protocols may not address.
The rapid physiological and psychosocial changes complicate treatment further. What a patient needs at 12 weeks differs dramatically from 28 weeks or postpartum. Sleep deprivation affects mood regulation. Hormonal shifts actively influence symptom presentation. Identity transitions from woman to mother carry profound psychological weight that unfolds over months.
Why standard BH protocols fall short
Traditional behavioral health systems weren’t designed for perinatal timelines. Standard intake processes are too slow. By the time patients complete waitlists and assessments, they’ve moved from second trimester to postpartum—essentially a different clinical picture.
Treatment approaches miss perinatal-specific presentations. Postpartum depression doesn’t always look like major depressive disorder. Intrusive thoughts about infant harm are common yet often misinterpreted by providers without perinatal training.
Most critically, coordination with OB/GYN care isn’t optional—it’s clinically necessary. Yet behavioral health typically operates in a silo. Providers don’t see prenatal labs, aren’t notified of complications, and have no systematic way to track medical issues impacting mental health.
Then there’s the postpartum drop-off. Patients disappear after delivery not because they’re better, but because follow-up falls through the cracks. The six-week visit often becomes the last touchpoint, right when mental health risk peaks.
Why the system fails perinatal behavioral health
Perinatal specialization remains niche, creating capacity constraints. Most communities have far more demand than specialized providers, leaving generalists to fill gaps without adequate support.
Many behavioral health providers work isolated from medical teams, making treatment decisions without visibility into complications. They’re unaware that anxiety spikes coincided with preeclampsia, or that depression worsened after NICU admission.
Tracking patients across transitions is logistically difficult. A patient may start care with one provider, deliver at another hospital, and postpartum follow-up happens through yet another channel.
The result? Providers manage high-stakes cases without infrastructure to do it well. They know their patients need more, but the system wasn’t built to deliver it.
This is why perinatal behavioral health demands a fundamentally different approach—not incremental improvements, but reimagined care delivery that matches the complexity of this critical window.
The three critical gaps behavioral health providers can't close alone
Understanding why perinatal behavioral health is different is one thing. Recognizing where the system actually breaks down is another. Let’s examine the three critical coordination gaps that no individual provider can close alone—and why they persist despite everyone’s best efforts.
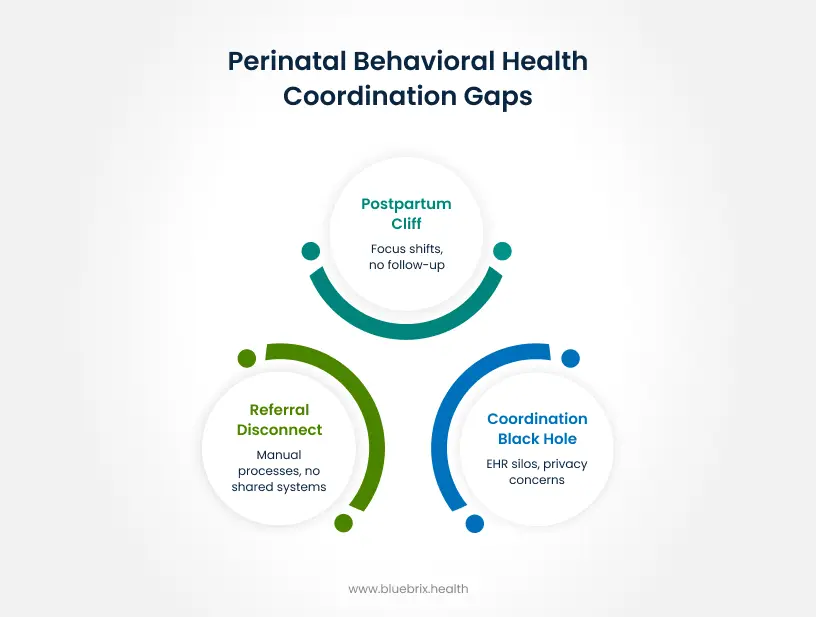
Gap 1: The referral disconnect
What providers experience:
An OB/GYN screens a patient at 20 weeks, identifies concerning depression symptoms, and refers to behavioral health. The patient never calls. Or she does call but after three weeks saying “my doctor told me to call you,” with zero clinical context. No screening scores, no history, no urgency indicators.
By the time the appointment happens, the clinical picture has shifted. What was moderate depression is now severe. What was anxiety is now panic attacks. And the referring provider? They have no idea whether their patient ever connected with care.
Why it happens:
Referral processes remain stubbornly manual. Paper lists of phone numbers. Business cards are handed over. “Here are some therapists who take your insurance—good luck.” Patients are left to navigate availability, insurance verification, and scheduling logistics while pregnant, working, and often already struggling.
There are no shared systems between OB and behavioral health practices. No digital handoffs. No automated follow-up. The referral leaves one system and enters a void, with both patient and referring provider left wondering what happens next.
The clinical impact:
Treatment delays during critical intervention windows. First trimester anxiety untreated becomes third trimester crisis. Patients fall through cracks between fragmented systems. The predictable result: increased emergency presentations when earlier, less intensive intervention could have prevented escalation.
Gap 2: The coordination black hole
What providers experience:
You’re treating a patient with perinatal anxiety. In the session, she mentioned being hospitalized last week for preeclampsia. You had no idea. Or you learn her OB just prescribed a medication that interacts with her psychiatric treatment—after the fact.
Or the reverse: you’ve been treating a patient for depression for months. She becomes pregnant. Suddenly, medication decisions become urgent—is this safe? Should we adjust? You need to coordinate with her OB/GYN, but there’s no established pathway, and you’re often making time-sensitive recommendations without direct communication with her medical team.
You’re making clinical decisions without the full picture, regardless of which direction the patient entered care.
Why it happens:
Different EHR systems that don’t talk to each other. Privacy concerns creating information silos—well-intentioned but counterproductive. Time constraints that make cross-discipline communication aspirational rather than routine.
The clinical impact:
Compromised treatment decisions. Medication safety concerns. Patients assessed multiple times by different providers asking the same questions, yet no one has the complete story. The promise of integrated care remains exactly that—a promise, not a reality.
Gap 3: The postpartum cliff
What providers experience:
Your patient was engaged throughout pregnancy. You built rapport, developed coping strategies, addressed trauma history. Then she delivers—and vanishes. Missed appointments. Unreturned calls.
Weeks later, a different patient appears: a postpartum referral already in crisis. Intrusive thoughts. Can’t sleep even when the baby sleeps. Feeling like a terrible mother. This could have been prevented.
Why it happens:
The medical system shifts focus after delivery. The six-week postpartum visit becomes the endpoint rather than a checkpoint. Meanwhile, patients are overwhelmed with newborn care, face childcare barriers to attending appointments, and instinctively deprioritize their own needs.
There’s no systematic mechanism to maintain connection during this vulnerable transition. Follow-up becomes the patient’s responsibility exactly when they have the least bandwidth.
The clinical impact:
Preventable postpartum depression, anxiety, and psychosis. Treatment starts from scratch instead of building on prenatal work. Higher acuity at presentation, requiring more intensive (and expensive) intervention. The momentum and trust built prenatally lost.
These gaps aren’t clinical failures. They’re system failures. And they can’t be solved by individual providers working harder. They require infrastructure that doesn’t yet exist in most perinatal care ecosystems.
These gaps aren’t abstractions. They’re daily realities for providers managing perinatal patients. So what would it actually take to close them? Not wishful thinking or incremental improvements—but fundamental infrastructure that makes coordination possible.
What coordinated perinatal behavioral health actually requires
The gaps are clear. The consequences are real. So, what does the solution actually look like?
It’s not about working harder or adding more referrals to already-overwhelmed providers. Coordinated perinatal behavioral health requires infrastructure—systems, workflows, and tools that make integration the default, not the exception. It requires rethinking how medical and behavioral health teams communicate, how patients move between services, and how care is tracked across the entire perinatal journey.
Here’s what that infrastructure must include:
Beyond co-location: true integration
True integration means a patient screened positive for depression at her OB visit doesn’t just get a business card. She gets a warm handoff, not a metaphor, but an operational reality. The medical assistant walks her down the hall, introduces her to the behavioral health care manager, and clinical context transfers instantly. The BH provider already knows her screening scores, pregnancy history, and medical complications before the conversation starts.
It means shared treatment planning where both the OB and therapist can see and update the same care plan. When the psychiatrist adjusts medication, the OB knows. When gestational diabetes is diagnosed, the therapist knows. Bidirectional communication is built into the workflow.
The essential infrastructure components
Systematic screening with action plans
Universal screening at every prenatal and postpartum visit isn’t enough if positive screens lead nowhere. The infrastructure must include risk stratification that triggers appropriate interventions automatically. Mild anxiety? Care manager follows up. Moderate depression? Expedited therapy referral. Suicidal ideation? Same-day crisis protocol.
Automated pathways ensure patients move from positive screen to treatment engagement without relying on them to “call this number.” And critically, tracking mechanisms flag when someone doesn’t show up, triggering outreach before they disappear entirely.
Intelligent referral management
When an OB refers a patient, clinical context should transfer automatically like screening results, medical history, current medications, urgency level. No more patients arriving saying “my doctor sent me” with zero background.
Provider matching happens based on specialization (perinatal experience), availability (next opening this week, not next month), and insurance. Referrals are tracked, and if a patient doesn’t schedule within 48 hours, alerts go out. Feedback loops close the circle: the referring provider gets confirmation that their patient is engaged or notification that they didn’t.
Real-time care coordination
Shared care plans need to be visible to everyone on the care team and updated in real time. The therapist documents a safety plan; the OB sees it immediately. The OB prescribes a new medication; the psychiatrist is notified.
Secure messaging between providers replaces phone tag. Questions get answered in hours, not days. Medication reconciliation happens across transitions—hospital discharge, specialist consultations, postpartum follow-up.
Documentation flows between systems while respecting privacy. Not every detail needs to be shared, but critical clinical information such as risk factors, treatment plans, medication changes—must be accessible.
Longitudinal patient tracking
Patients need to be followed across the entire perinatal period, not just pregnancy. Automated touchpoints at high-risk timeframes—first trimester, third trimester, two weeks postpartum, six weeks postpartum to ensure no one falls off the radar.
Transition planning from prenatal to postpartum care happens proactively, not reactively. And integration extends to pediatric systems: the baby’s first pediatric visit should trigger a maternal mental health check-in.
The role of specialized providers
Infrastructure alone isn’t enough without networks of perinatal-trained behavioral health providers. Communities need therapists who understand intrusive thoughts aren’t psychosis, psychiatrists comfortable managing medications during pregnancy, and peer support specialists who’ve lived the experience.
Crisis intervention protocols specific to perinatal presentations—differentiating postpartum psychosis from panic attacks, understanding infanticide risk factors are essential. Team-based care models with clear roles and communication pathways ensure everyone knows who’s responsible for what, and how to reach each other when things escalate.
This infrastructure isn’t theoretical. Technology platforms are finally making it operationally feasible. Here’s how the right tools transform each of those critical gaps from inevitable failures into coordinated care.
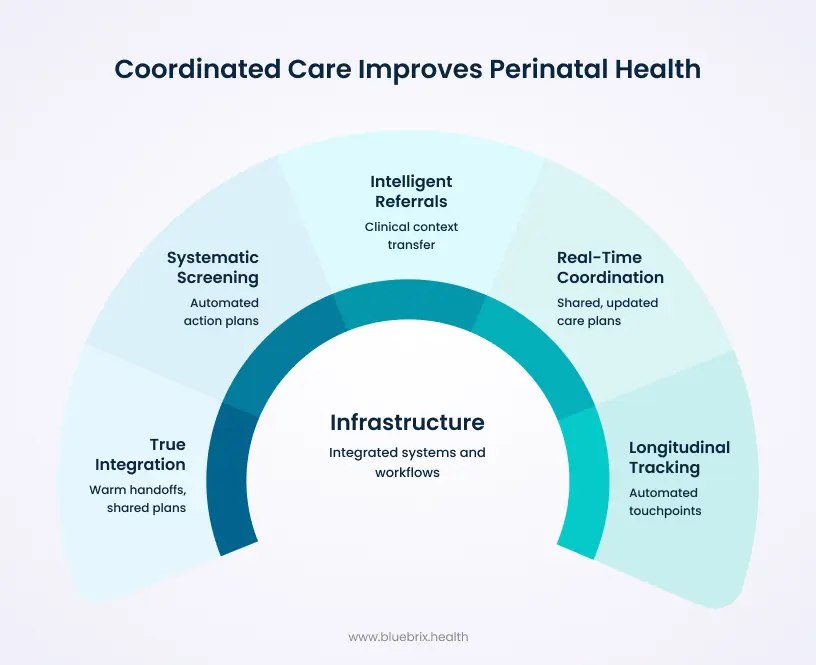
How technology transforms perinatal behavioral health coordination
Perinatal behavioral health isn’t just another specialty requiring referrals; it’s a time-sensitive, high-risk clinical scenario requiring seamless coordination across medical and behavioral health systems that traditionally operate independently. Manual processes cannot keep pace with the clinical urgency, the volume of screening, or the complexity of coordinating multiple providers across a nine-month (and beyond) care journey.
From screening to treatment: closing the first gap
The traditional failure point: Patient screens positive for depression at 28-week prenatal visit. OB provides phone numbers for three therapists. Patient calls all three: one doesn’t accept her insurance, one has a three-month wait, one doesn’t specialize in perinatal. Patient gives up. Depression worsens untreated.
How blueBriX changes the equation: blueBriX integrates validated screening tools directly into prenatal visit workflows. When a patient screens positive, the system automatically identifies appropriate perinatal-specialized providers based on insurance, location, availability, and clinical needs. Referrals include complete clinical context—screening scores, medical history, current medications, risk factors.
blueBriX’s notification engine eliminates manual tracking; it monitors referral status and automatically alerts care coordinators when referrals stall. No spreadsheets, no calendar reminders, no patients slipping through cracks. Referring OB/GYNs receive automatic confirmation when patients engage with treatment.
The difference: Time from positive screen to first BH appointment drops from weeks (or never) to days. No manual follow-up burden on providers.
Real-time coordination: closing the second gap
The patient has been in therapy for depression for six months. She becomes pregnant. Suddenly, her medication needs urgent review—is it safe? Should dosing change? Her therapist needs to coordinate with her OB/GYN, but there’s no established communication pathway. Meanwhile, the OB doesn’t know about her psychiatric history or current medications until the patient mentions it at a later visit. Critical decisions are being made in silos during a time-sensitive window.
How blueBriX changes the equation:
blueBriX’s treatment plan engine creates shared, dynamic care plans accessible to all team members. When a patient becomes pregnant, her existing BH provider and new OB team are automatically connected through the platform. Medical updates—prenatal appointments, lab results, complications—are visible to BH providers in real time. Mental health status, medication changes, and risk factors are immediately accessible to the OB team.
The engine maintains a single source of truth: medication lists reconcile automatically across all prescribers, interventions are documented centrally, and escalation protocols are clear to everyone—without anyone chasing information. Secure messaging enables quick consultations between providers when urgent decisions arise.
The difference: Complete clinical picture without administrative burden. BH and medical teams coordinate seamlessly from the moment pregnancy is confirmed. Everyone works from the same playbook, updated in real time. Reduced risk from medication interactions because reconciliation is automatic.
Sustained support: closing the third gap
The traditional failure point: Patient engaged in prenatal therapy delivers at 37 weeks. Focused on newborn care, she misses her next BH appointment. Therapist leaves voicemail but gets no response. Three months later, patient presents to the emergency department with severe postpartum depression and suicidal ideation.
How blueBriX changes the equation: blueBriX tracks patients longitudinally across the entire perinatal period, not just pregnancy. Automated outreach at critical timeframes (immediately postpartum, 2 weeks, 6 weeks, 3 months, 6 months) ensures patients don’t fall off the radar.
Telehealth options reduce barriers for new mothers who can’t easily leave home. Integration with pediatric care systems creates touchpoints at well-baby visits. Care navigators supported by blueBriX workflows proactively address barriers to continued engagement—childcare, transportation, insurance changes.
The difference: Continuity of care across pregnancy and postpartum period. Early intervention before symptoms reach crisis levels. Support sustained through the highest-risk postpartum period.
But technology that coordinates care is only half the equation. To improve systems, you need to see them clearly. That’s where analytics transform not just individual patient outcomes, but entire care networks.
Analytics that drive continuous improvement
Manual coordination doesn’t just fail patients; it also makes it impossible to see where and why it’s failing. Without data, quality improvement is guesswork. blueBriX changes that.
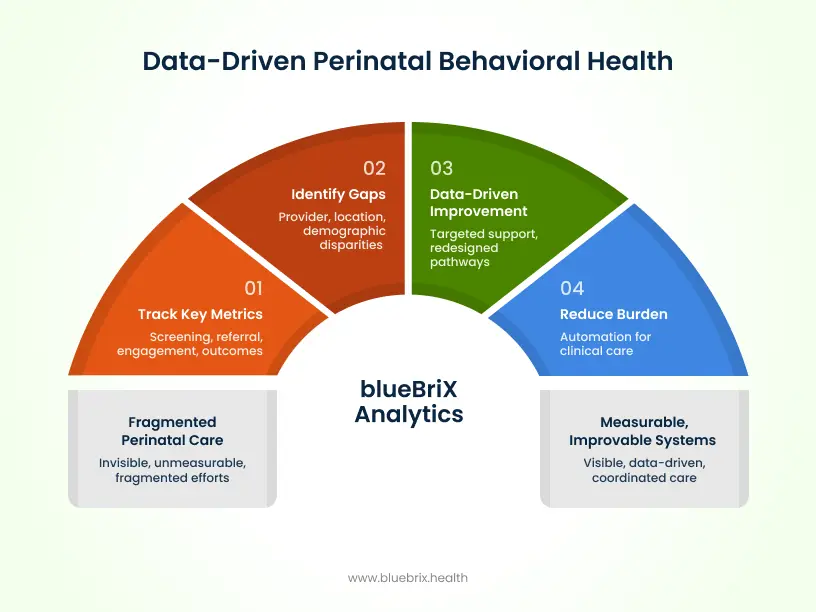
What blueBriX measures:
blueBriX tracks the metrics that matter for perinatal behavioral health coordination:
- Screening rates at each prenatal and postpartum visit, broken down by provider and location. Are patients being screened consistently, or are there gaps?
- Referral completion rates and time from screen to first appointment. How many patients who screen positive actually connect with treatment? How long does it take? Where do referrals stall?
- Treatment engagement and retention across the perinatal period. Are patients staying engaged prenatally? Are they dropping off postpartum? At what point does engagement decline?
- Clinical outcomes using validated perinatal mental health measures. Are symptoms improving? Are interventions working?
- Disparities in screening, referral, and treatment access by demographics—race, ethnicity, language, insurance status. Who’s falling through the cracks, and why?
How this changes practice
Network managers can identify providers or locations with screening gaps and provide targeted support—training, workflow adjustments, resource allocation. Referral pathways that consistently fail to get redesigned. High-performing workflows get documented and scaled across the network.
Quality improvement becomes data-driven rather than anecdotal. Instead of “I think referrals are taking too long,” it’s “our average time from screen to appointment is 18 days, and here’s where the delays happen.” Problems become visible, and solutions become measurable.
The provider benefit
For individual providers, blueBriX offers something rarely available: visibility into how your referrals actually perform. Did the patient you referred last month connect with care? Are your referrals completing at higher rates than average? You get recognition for your role in improved outcomes, not just the act of referring.
And critically, reduced administrative burden through automation means more time for clinical care, less time on coordination logistics. You’re not tracking referrals manually, chasing down information, or wondering what happened to patients after they left your care. The system handles it, and you stay informed.
blueBriX doesn’t just coordinate care—it makes the invisible visible, turning fragmented efforts into measurable, improvable systems.