Nearly 130 million Americans live in areas with mental health professional shortages, yet demand for behavioral health services continues to surge, outpacing workforce growth and stretching resources thin.
Traditional network-building strategies designed for medical-surgical care fail in behavioral health. Provider directories go stale within weeks. Patients struggle to find in-network therapists acceptin g new clients. Referrals disappear into black holes. The result? Delayed care, worsening outcomes, and growing organizational liability as regulatory scrutiny intensifies.
The stakes extend beyond compliance—they’re rising fast. Every access barrier costs health plans in medical expenses, impacts star ratings, and erodes member trust. For providers, fragmented networks mean administrative chaos and care coordination failures. Communities bear the ultimate burden—untreated conditions, preventable crises, and widening health disparities.
This guide outlines how modern health plans and provider organizations are building behavioral health networks that actually work—networks designed for the unique complexities of mental health and substance use care, powered by technology that turns fragmentation into coordination.
Understanding the behavioral health landscape
The current state of behavioral health access
The provider shortage isn’t uniform—it hits certain specialties harder than others. Child and adolescent psychiatrists are critically understaffed due to training pipeline limitations, while Licensed Clinical Social Workers and Licensed Professional Counselors face mounting capacity constraints from post-pandemic demand surges. Substance abuse counselors remain persistently undersupplied despite escalating need.
Geography deepens the crisis. Rural counties often have no behavioral health providers at all, with states like Wyoming and Utah reporting over 80% of their population living in shortage areas.
What “comprehensive” really means
Comprehensive behavioral health care requires an integrated continuum—from prevention programs and early intervention to acute treatment, crisis management, and sustained recovery support. It also means bridging the gap between physical and behavioral health, particularly since up to 75% of primary care visits include behavioral health components.
Building networks that deliver this level of care demands more than recruiting diverse provider types. It requires multi-disciplinary collaboration where psychiatrists, therapists, primary care providers, peer specialists, and care coordinators function as coordinated teams rather than independent silos. Without intentional network design and management, information doesn’t flow between providers, medication management becomes inconsistent, and patients—especially those with complex needs requiring multiple specialties—fall through the cracks. The result: episodic treatment replaces continuous care, and crisis intervention becomes the default instead of prevention. Effective provider network management transforms this fragmented reality into coordinated care delivery.
Core components of a strong behavioral health network
The foundation of any effective provider network lies in the providers themselves and the way the network is thoughtfully structured to meet the diverse needs of the populations served. Several essential components define the strength of such a network, ensuring it delivers comprehensive, accessible, high-quality, and equitable behavioral health care.
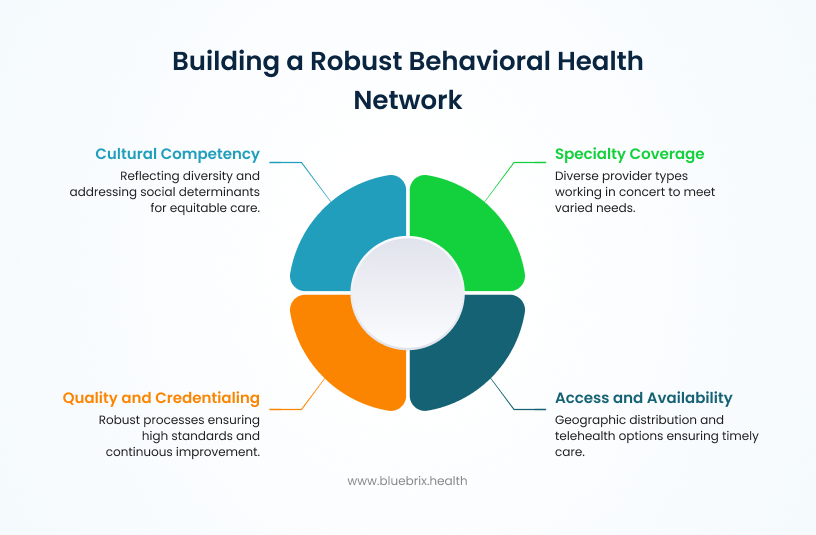
Specialty coverage and depth
Comprehensive networks require diverse provider types working in concert. Psychiatrists, psychologists, licensed clinical social workers, licensed professional counselors, psychiatric nurse practitioners, and substance abuse counselors each bring distinct capabilities. Population health planning considers appropriate ratios of each provider type relative to the served population, while subspecialty coverage addresses specific needs—eating disorders, trauma treatment, geriatric behavioral health, and child/adolescent services require specialized training and experience.
Access and availability
True network adequacy means providers are geographically distributed where patients live, appointment wait times are reasonable for both routine and urgent needs, and telehealth options expand access beyond physical locations. Telehealth’s effectiveness depends on providers holding appropriate interstate licenses to serve patients across state lines, particularly important for networks serving multi-state regions or patients who travel frequently. After-hours and crisis coverage capabilities ensure patients can access care when acute needs arise, not just during standard business hours.
Quality and credentialing
Beyond verifying basic licensure, robust credentialing processes assess providers’ evidence-based practice capabilities, outcomes tracking participation, and commitment to continuous education. Peer review processes support quality improvement while maintaining clinical independence and professional judgment.
Cultural competency and health equity
Networks must reflect the diversity of populations served. This includes recruiting providers from varied backgrounds, ensuring language access for non-English speakers, implementing trauma-informed care standards across all providers, and addressing social determinants of health that impact behavioral health outcomes. Cultural competency isn’t an add-on; it’s fundamental to care effectiveness.
These components work together to create networks where patients can find appropriate, accessible, quality care that respects their individual circumstances and needs.
Strategic approaches for sustainable provider network management
Building comprehensive behavioral health networks requires strategic planning that addresses current gaps, attracts quality providers, and creates partnerships that extend network reach. Here are some proven strategies for network success!
Assessment and gap analysis
Effective network development starts with understanding population health needs through demographic analysis, behavioral health prevalence data, and utilization patterns. Current network evaluation identifies where coverage falls short—specific specialties, geographic areas, or underserved populations facing access barriers. Data-driven decision making ensures network expansion addresses actual needs rather than assumptions, prioritizing investments where they’ll have the greatest impact on access and outcomes.
Recruitment and contracting strategies
In competitive labor markets, attracting quality providers requires more than competitive reimbursement rates. Value propositions should emphasize reduced administrative burden through streamlined processes, care coordination support that reduces provider workload, professional development opportunities, and practice support resources. Contract structures can incentivize quality care through performance metrics while maintaining flexibility that respects clinical judgment. Addressing administrative burden directly—through technology automation, simplified authorization processes, and efficient credentialing—makes networks more attractive to providers who want to focus on patient care.
Building strategic partnerships
Networks extend their reach through partnerships with community mental health centers that serve uninsured and underinsured populations, academic medical centers that provide specialized services and training programs, school-based programs that reach children and adolescents early, peer support organizations that complement clinical services with lived experience, and crisis intervention services that provide immediate response capabilities.
Integration with primary care
Behavioral health integration with primary care improves outcomes through co-location models that place behavioral health providers in primary care settings, collaborative care models where primary care and behavioral health teams work together on shared patients, warm handoff protocols that facilitate seamless referrals, and shared care planning tools that ensure all providers work from a unified treatment approach.
Strategic network development isn’t just about adding providers—it’s about creating an ecosystem where patients can access the right care at the right time through coordinated, supported provider networks.
Common challenges in building comprehensive provider networks
Building and maintaining comprehensive behavioral health networks involves navigating persistent challenges that require both systemic solutions and practical strategies.
Provider recruitment and retention
Provider burnout remains a critical concern in behavioral health, driven by heavy caseloads, administrative burden, and emotional demands of the work. Networks that prioritize burnout prevention through reasonable panel sizes, administrative support, and professional development opportunities see better retention. Competitive compensation matters, but reducing administrative friction through technology and streamlined processes often proves equally valuable in attracting and keeping quality providers.
Regulatory and compliance complexity
Multi-state licensure requirements complicate telehealth expansion, requiring providers to maintain credentials across multiple jurisdictions. Mental health parity compliance ensures behavioral health benefits match medical benefits in scope and coverage. Documentation requirements must balance clinical needs with regulatory demands, while evolving telehealth regulations require ongoing monitoring and adaptation as policies continue to shift post-pandemic.
Financial sustainability
Behavioral health reimbursement rates often lag behind medical specialties, creating financial pressure on networks. Value-based care models that reward outcomes rather than volume offer promising alternatives. Risk adjustment mechanisms ensure networks serving higher-acuity populations receive appropriate resources. Payment reform advocacy remains essential to creating sustainable funding structures that support comprehensive network development.
Addressing these challenges requires coordination between payers, providers, policymakers, and technology partners working toward shared goals of access, quality, and sustainability.
Technology: the operational backbone of comprehensive provider networks
The complexity of building and maintaining comprehensive behavioral health networks demands sophisticated technology infrastructure. Manual processes and disconnected systems cannot scale to meet the demands of coordinated care across diverse provider types, specialties, and geographic regions. Modern network management platforms transform how health plans, providers, and patients connect—turning fragmentation into coordination and administrative burden into streamlined workflows.
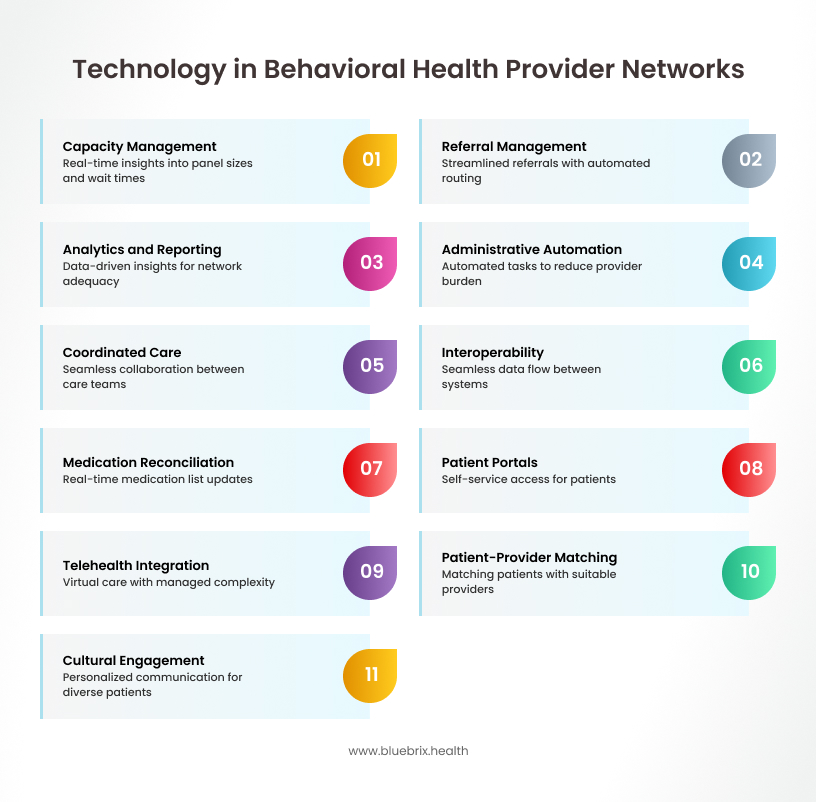
Network management technology
Capacity management and matching algorithms
Real-time insight into panel sizes, appointment availability, wait times, and patient acuity enables proactive management rather than reactive crisis response. Intelligent matching must consider clinical needs, geographic proximity, insurance coverage, language preference, cultural factors, and provider specialty simultaneously.
How blueBriX optimizes matching: blueBriX employs algorithms that analyze these dimensions in real-time to identify capacity constraints before they become access barriers. The platform tracks ownership of patient relationships across the care continuum, ensuring accountability. When a patient requires substance abuse counseling with Spanish language capability in a specific area, the system instantly identifies appropriate matches, reducing the critical time from referral to first appointment.
Closing the referral loop: No patient left behind
Referral management in behavioral health requires clinical information to flow seamlessly while capturing patient preferences, communicating urgency, and clarifying care coordination requirements. Manual referral processes lead to delays, lost information, and patients who never connect with referred providers.
blueBriX’s intelligent referral engine: blueBriX streamlines referrals through comprehensive documentation while automating routing based on configurable criteria including clinical protocols, network adequacy requirements, and contractual obligations. The platform’s rule engine automatically verifies network participation, benefit coverage, and authorization requirements at the point of referral. Complete audit trails document every handoff, while providers receive referrals with full clinical context that reduces duplicative assessments.
Analytics and reporting capabilities
Data-driven network management requires visibility into network adequacy by geography and specialty, utilization patterns, access metrics, referral completion rates, and care continuity indicators. Without robust analytics, network managers discover gaps only when patients complain or regulators identify deficiencies.
blueBriX analytics infrastructure: blueBriX provides real-time dashboards that surface actionable insights, enabling proactive network development. Reporting capabilities address diverse stakeholder needs from regulatory compliance reports to CMS requirements, utilization reports for contracting, and clinical quality metrics. Customizable dashboards give network managers, clinical leadership, and executive teams specific insights without manual data compilation.
Supporting provider success
Reducing administrative burden through automation
Administrative tasks like eligibility verification, benefit checks, authorization tracking, and appointment reminders consume time providers would rather spend on patient care. Technology should handle these routine processes automatically.
blueBriX’s automation philosophy: blueBriX automates these processes comprehensively. Form data collected during patient intake flows directly into clinical documentation systems. Authorization workflows run end-to-end automatically—the system initiates requests with clinical documentation, tracks submissions, and notifies relevant parties without provider involvement. Credentialing processes integrate with primary source verification systems, with automated notifications for credential renewals.
Coordination without the chaos: unified care communication
Behavioral health care coordination requires communication across diverse provider types who often don’t share electronic health record systems. Fragmented communication leads to duplicated services, medication errors, and conflicting treatment recommendations.
blueBriX’s coordination infrastructure: blueBriX provides secure messaging, care plan sharing, and care team directories that enable collaboration regardless of underlying technology systems. Continuity of care documentation flows automatically between providers at transition points. Medication reconciliation becomes systematic, with the platform maintaining current medication lists that update with each encounter and flag potential duplications, interactions, or gaps.
Making systems talk: seamless interoperability and data flow
Healthcare interoperability remains challenging, particularly in behavioral health where privacy considerations add complexity. Platforms must support standard health information exchange protocols while maintaining HIPAA compliance and 42 CFR Part 2 requirements.
blueBriX’s interoperability framework: blueBriX supports standard protocols (HL7, FHIR) while maintaining regulatory compliance. Integration with electronic health record systems enables bidirectional data flow—clinical information from provider EHRs enriches care coordination, while referral information and care plans flow back into provider systems, eliminating information silos.
Real-time medication reconciliation across prescribers
Behavioral health patients often receive prescriptions from multiple providers—psychiatrists, primary care physicians, specialists—creating risks for medication errors, dangerous interactions, and treatment gaps. When medication information exists in disconnected systems, providers lack visibility into what patients are actually taking, leading to polypharmacy risks and potentially dangerous drug interactions.
blueBriX’s medication reconciliation framework: blueBriX maintains a comprehensive, real-time medication list that updates automatically with each clinical encounter across the care network. The platform flags drug-drug interactions, duplicate therapies, dosing concerns, and gaps in expected refills. When patients transition between care settings or providers, medication reconciliation becomes automatic. Alerts notify prescribers of potential safety issues before prescriptions are finalized, ensuring every provider has access to accurate, current medication information without manual compilation.
Enabling patient access
The front door that’s always open: self-service patient portals
Patients increasingly expect digital-first experiences—searching for providers, viewing availability, and scheduling appointments online rather than through phone calls. These digital entry points must be intuitive, comprehensive, and integrated with backend systems.
blueBriX’s patient portal experience: blueBriX powers patient portals that serve as comprehensive entry points. Patients search for providers using criteria that matter to them, view real-time availability, and schedule appointments without phone calls. The experience extends to self-service capabilities including updating insurance information, completing intake forms, accessing educational resources, and communicating securely with care teams.
Care without boundaries: integrated telehealth that just works
Geographic barriers, transportation challenges, and scheduling constraints limit access to in-person services. Telehealth expands access, but implementation complexity around scheduling, consent, interstate licensure verification, and integration with in-person care creates operational challenges.
blueBriX’s telehealth integration: blueBriX-integrated telehealth capabilities expand access while managing operational complexity. The platform handles scheduling, ensures informed consent, verifies interstate licensure, and facilitates seamless transitions between in-person and virtual care modalities. Providers can offer hybrid care models with the platform managing logistics automatically.
Intelligent patient-provider matching
Finding the right behavioral health provider shouldn’t require extensive research and trial and error. Effective matching considers clinical requirements, logistical factors, personal preferences, and evidence about which provider-patient matches produce better outcomes.
blueBriX’s matching and navigation: blueBriX’s matching capabilities guide individuals to providers who fit their specific needs across all relevant dimensions. Care navigators, supported by blueBriX workflows, help patients overcome barriers including understanding insurance benefits, completing prior authorizations, and coordinating with multiple providers. The platform ensures no navigation task falls through the cracks.
Culturally appropriate engagement tools
One-size-fits-all approaches fail in behavioral health, where cultural context profoundly influences care engagement. Platforms must support multilingual communications, culturally adapted materials, and workflows that accommodate diverse preferences at scale.
blueBriX’s personalization at scale: blueBriX enables automated personalization, for instance, Spanish-language appointment reminders for Spanish-speaking patients, text-based communication for those who prefer it, simplified language for patients with literacy challenges, and culturally relevant mental health education. Also, we prioritize personalization based on medical conditions and patient preferences to ensure care is relevant, timely, and aligned with individual needs. This improves care engagement across diverse populations without adding administrative burden.




