For clinics specializing in behavioral health, where the nuances of patient data are particularly sensitive and the demands of value-based care are increasingly prominent, understanding the intricacies of data migration is essential. This blog delves into the critical considerations every behavioral health clinic must grasp before embarking on the journey of switching EHRs, especially when considering a purpose-built EHR which offers a comprehensive solution.
Why switching behavioral health EHRs demands careful consideration
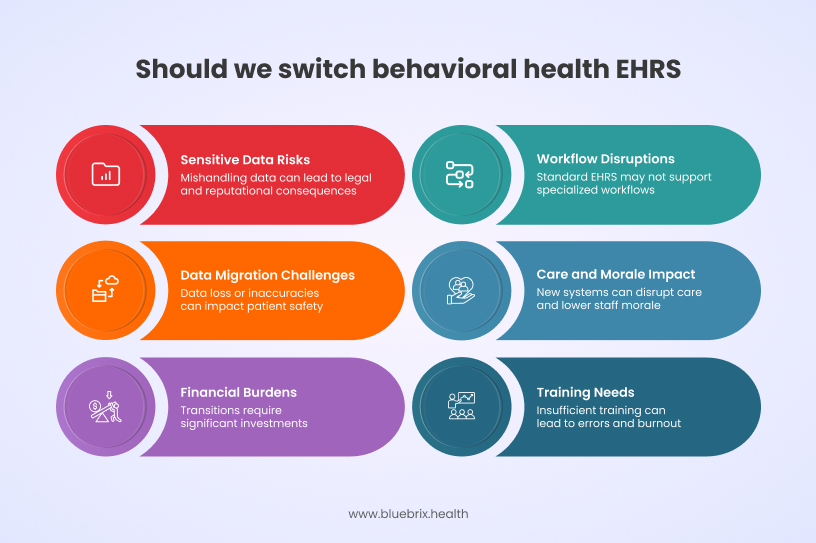
Switching behavioral health EHRs if rushed or underestimated, can lead to significant setbacks and risks. Several critical factors that make this transition particularly challenging and underscore the need for meticulous planning are listed below.
Sensitive data and regulatory compliance
Behavioral health records often contain highly sensitive patient information and are subject to stricter confidentiality regulations, such as HIPAA and 42 CFR Part 2. Mishandling data during migration or insufficient security in the new system can result in severe legal, financial, and reputational consequences.
Complex and specialized workflows
Behavioral health providers require EHR systems that support specialized workflows, including group therapy documentation, customized treatment plans, and unique reporting needs. Standard EHRs may lack these capabilities, leading to workflow disruptions and reduced care quality if not carefully addressed during the transition.
Data migration risks
Migrating data from legacy systems, paper records, or outdated digital platforms is inherently complex. Risks include data loss, duplication, or inaccuracies, which can directly impact ongoing treatment and patient safety.
Disruption to care and staff morale
Introducing a new EHR disrupts established workflows and requires staff to adapt to new processes, which can temporarily reduce efficiency and care quality. Resistance to change, especially among teams accustomed to manual or legacy systems, can further complicate adoption.
Financial and resource burdens
EHR transitions are costly, labor-intensive, and time-consuming. They require significant investments in training, support, and sometimes short-term consultants. Insufficient planning or resources can lead to unexpected expenses and operational strain.
Training and change management
Successful transitions hinge on comprehensive staff training and ongoing support. Without adequate preparation, staff may struggle with the new system, leading to errors, inefficiencies, and clinician burnout.
Recommended migration strategy for behavioral health clinics

The best migration strategy for a behavioral health clinic switching EHRs depends on the organization’s size, data complexity, and risk tolerance. A phased migration approach is generally recommended for behavioral health settings due to the sensitivity of patient data and the need for minimal care disruptions. Below is a structured strategy suggested by industry best practices:
Step 1: pre-migration planning
- Assess data needs: Identify critical data like patient histories, treatment plans, and progress notes. Archive outdated data to simplify migration.
- Workflow analysis: Map clinical and administrative workflows (e.g., group therapy documentation, billing) to align the new EHR with behavioral health needs.
- Regulatory compliance: Ensure the new EHR adheres to HIPAA, 42 CFR Part 2, and 21st Century Cures Act standards with encryption and role-based controls.
Step 2: phased migration approach
- Pilot phase: Migrate a small data subset (5-10%) for testing to identify mapping errors and workflow gaps early.
- Incremental migration: Transfer data in batches (e.g., by provider team or patient cohort) for gradual adaptation and reduced downtime.
- Final cutover: Complete the transfer after successful testing and training, ensuring full system readiness.
Step 3: data integrity and security
- Data cleansing: Remove duplicates, standardize formats, and validate records before migration.
- Secure transfer: Use encrypted pipelines and audit trails to protect sensitive data.
- Validation checks: Cross-check migrated data for accuracy, especially unstructured notes.
Step 4: stakeholder involvement
- Clinical champions: Involve providers in workflow design and testing for better usability.
- Vendor collaboration: Work closely with EHR vendors to address technical challenges.
Step 5: training and support
- Role-based training: Customize training for clinicians, billing staff, and administrators.
- Post-migration support: Designate “super-users” and provide ongoing support to address issues quickly.
Step 6: contingency planning
- Backup and rollback: Maintain secure backups and have a rollback plan ready for critical failures.
- Downtime protocols: Establish temporary workflows to avoid care disruptions during migration.
Common pitfalls and how to avoid them
Below are the most common pitfalls and proven strategies to avoid them, based on current best practices and expert guidance.
Data integrity issues
Pitfalls:
- Data loss, corruption, or inconsistency during migration.
- Unstructured data (e.g., clinical notes, historical documents) failing to map correctly, leading to fragmented information.
- Duplicate records or formatting incompatibilities causing confusion in patient care.
How to avoid:
- Conduct thorough data validation and reconciliation before, during, and after migration.
- Clean and standardize data prior to migration to resolve duplicates and correct errors.
- Perform test migrations with sample data to identify and fix issues early.
Patient safety risks
Pitfalls:
- Incomplete or inaccurate transfer of critical clinical data (e.g., medication lists, allergy information), leading to treatment errors.
- Limited access to legacy records during transition, risking delays or mistakes in care delivery.
How to avoid:
- Ensure clinicians have timely access to accurate legacy data throughout the migration.
- Implement real-time supervisory reviews and validation of migrated data, especially for high-risk information like medications and allergies.
- Maintain parallel access to legacy systems until the new EHR is fully validated.
Security and compliance failures
Pitfalls:
- Data breaches or unauthorized access during migration, particularly with sensitive behavioral health information.
- Non-compliance with HIPAA, 42 CFR Part 2, or the 21st Century Cures Act, risking legal penalties and reputational harm.
How to avoid:
- Use end-to-end encryption for all data in transit and at rest.
- Implement multi-factor authentication and strict role-based access controls.
- Conduct regular security audits and compliance checks before, during, and after the migration.
Inadequate planning and stakeholder engagement
Pitfalls:
- Poorly defined migration scope leading to unnecessary data transfer, increased costs, and extended downtime.
- Lack of collaboration among clinical, administrative, and IT teams, resulting in workflow disruptions and missed requirements.
How to avoid:
- Define clear migration goals, scope, and success metrics at the outset.
- Engage all stakeholders early and throughout the process to ensure alignment and address concerns.
- Develop a detailed migration timeline with contingency plans for unexpected issues.
Insufficient training and change management
Pitfalls:
- Staff resistance to the new EHR due to unfamiliarity, leading to workflow inefficiencies and increased error rates.
- Lack of ongoing support post-migration, resulting in unresolved user challenges and poor adoption rates.
How to avoid:
- Provide comprehensive, role-based training before and after go-live, tailored to clinical and administrative needs.
- Establish a dedicated IT support team and super-users to assist with troubleshooting.
- Offer continuous learning resources and refresher sessions to reinforce best practices and system updates.
Overlooking post-migration monitoring
Pitfalls:
- Failing to monitor system performance and data quality after migration, allowing errors to persist unnoticed.
- Neglecting to audit for security vulnerabilities or compliance gaps post-migration.
How to avoid:
- Schedule structured post-migration evaluations, including data integrity checks and system audits.
- Track user adoption, gather feedback, and address usability issues promptly.
- Perform regular risk assessments and update security protocols as needed.
Key questions to ask your potential EHR vendor (including blueBriX)
Before committing to a new EHR, it’s crucial to ask potential vendors detailed questions about their data migration process and capabilities, especially in the context of behavioral health. Here are some key inquiries to consider when evaluating vendors like blueBriX:
- What is your experience with behavioral health data migration? – Behavioral health records have unique data types (e.g., therapy notes, group sessions, 42 CFR Part 2 data). Vendors with proven experience are more likely to anticipate and address these complexities.
- Can you describe your migration process step-by-step? – A transparent, well-documented process ensures you understand each migration phase, from pre-migration assessment to post-migration validation, reducing the risk of data loss or workflow disruption.
- How do you ensure data integrity, accuracy, and completeness during migration? – Ask about data cleansing, mapping, validation, and reconciliation steps to ensure all critical information is transferred correctly.
- What security measures are in place to protect data during migration? – Ensure the vendor uses end-to-end encryption, role-based access, and audit trails to comply with HIPAA and 42 CFR Part 2.
- How do you handle regulatory compliance (HIPAA, 42 CFR Part 2, 21st Century Cures Act)? – Non-compliance can result in legal penalties and reputational harm. The vendor must demonstrate robust compliance protocols throughout the migration process.
- Do you offer phased or “big bang” migration options and which do you recommend for our organization? – Phased migrations minimize risk and disruption, especially for larger or more complex organizations. Understanding options helps you choose the best fit for your needs.
- What support and training do you provide before, during, and after migration? – Comprehensive support prevents workflow disruptions and ensures staff are comfortable with the new system, which is especially important in behavioral health settings.
- Can you provide references from similar behavioral health organizations? – Real-world examples validate the vendor’s capabilities and reliability in handling behavioral health data migrations.
- How do you handle legacy data, including attachments, scanned documents, and unstructured notes? – Behavioral health records often include non-standard data types. Ensure all relevant information, not just structured fields, will be migrated and accessible.
- What is your contingency plan if data migration encounters issues or failures? – A clear rollback or recovery plan is vital to prevent data loss or extended downtime during migration.




