The Centers for Medicare and Medicaid Services (CMS) has unveiled a transformative successor to ACO REACH that fundamentally reshapes how accountable care organizations can participate in Medicare value-based care. The Long-term Enhanced ACO Design (ACO LEAD) model represents a significant evolution in the way CMS supports providers moving away from traditional fee-for-service arrangements toward outcome-focused partnerships with their patients. With less than 12 months until the model launches on January 1, 2027, this is no longer a future consideration—it is an immediate strategic decision for every practice evaluating its financial sustainability beyond 2026.
For the past few years, ACO REACH (Realizing Equity, Access, and Community Health) served as CMS’ primary testing ground for advanced value-based care. Launched in 2023, it introduced critical innovations specifically, a focus on health equity and a shift toward provider-led governance rather than hospital-centric control. However, as a short-term model set to expire at the end of 2026, REACH presented a challenge: its volatility and limited timeline made it difficult for smaller, independent, and rural practices to invest in the necessary long-term infrastructure.
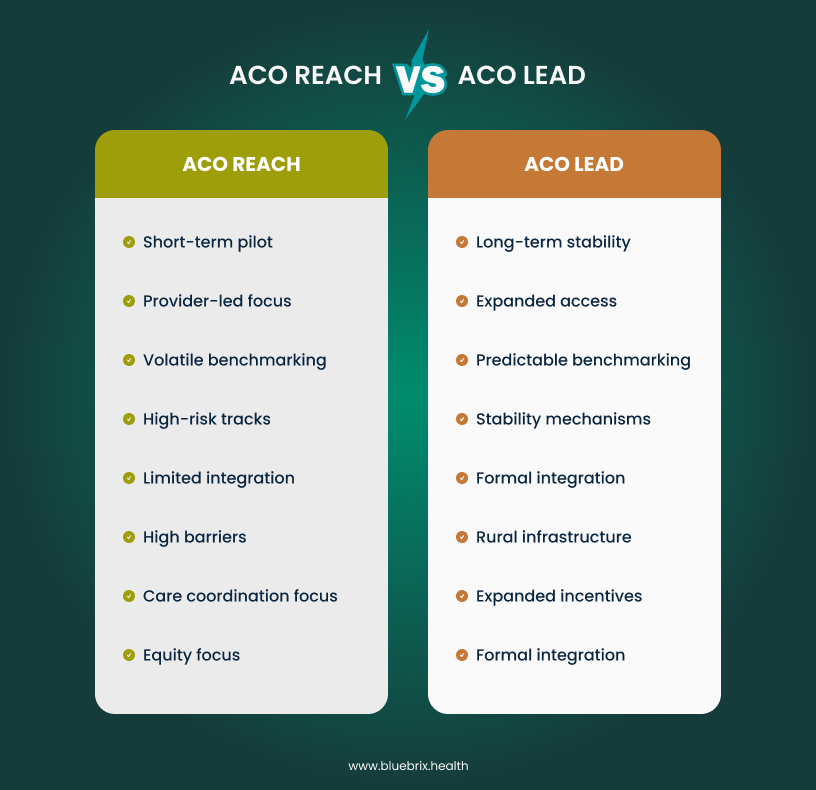
While ACO REACH proved that equity and risk could coexist, ACO LEAD provides the predictability and financial support required to make that model viable for the next decade.
For independent practices, small physician groups, and rural healthcare providers struggling with the complexity of prior ACO models, this announcement signals a critical opportunity. But only for those who understand what makes LEAD different, how to prepare for it, and crucially, how much time they have left to make it happen. If you’re still operating under the assumption that you have “time to think about it,” you’re already behind.
Understanding ACO LEAD: The next generation of accountable care
The ACO LEAD model, which will begin operations on January 1, 2027, is purposefully designed to address the barriers that have discouraged provider participation in advanced value-based care arrangements over the past several years. Rather than continuing with the iterative tweaks that characterized earlier CMS approaches, LEAD represents a comprehensive rethinking of how to make accountable care sustainable for diverse provider types.
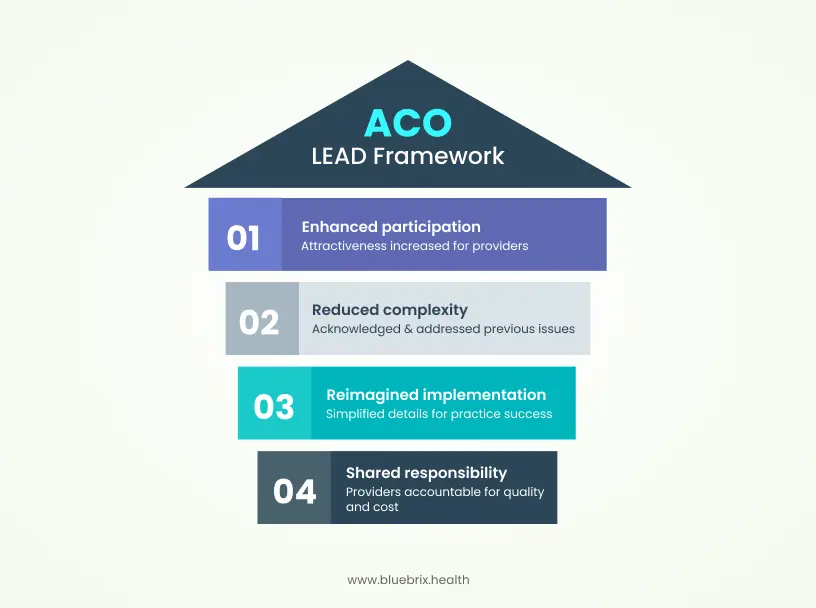
At its core, ACO LEAD maintains the fundamental principle underlying all accountable care organizations: providers accept shared responsibility for both the quality and cost of care delivered to a defined population of Medicare beneficiaries. However, the implementation details have been substantially reimagined. This distinction is critical. CMS leadership explicitly acknowledged that previous ACO models, while well-intentioned, created unnecessary complexity and financial risk that made participation unattractive to many providers, particularly those without large hospital system backing.
The financial architecture: How payment changes in ACO LEAD
One of the most substantive differences between ACO LEAD and its predecessors involves how payments flow to participating providers. ACO LEAD introduces a 10-year performance period with stable benchmarks, a dramatic departure from models that rebased benchmarks periodically. For a practice evaluating whether to participate, this change directly affects cash flow predictability and long-term financial planning.

Prospective capitated payments and monthly cash flow
Rather than waiting for year-end settlement based on actual claims experience, ACO LEAD provides prospective monthly capitation payments. This means practices know in advance what payment they can expect, enabling more confident investment in care infrastructure and staff. The predictability is intentional—CMS heard consistently from providers that retrospective risk arrangements created cash flow volatility that made it nearly impossible to invest in the care coordination capabilities that actually drive better outcomes.
Practices in ACO LEAD will have two voluntary risk-sharing tracks available:
- Global risk track: ACOs can retain up to 100% of savings but bear responsibility for up to 100% of losses relative to an established benchmark.
- Professional risk track: ACOs can receive up to 50% of savings while assuming responsibility for up to 50% of losses.
This optionality is deliberate. Not every practice has the same tolerance for downside risk, and CMS explicitly rejected the one-size-fits-all mentality that characterized earlier models.
Enhanced financial support for rural and independent providers
Recognizing that infrastructure investment represents a genuine barrier for smaller providers, ACO LEAD includes add-on payments specifically for rural healthcare providers to help them develop the operational foundations necessary for accountable care participation. This is actual financial assistance to offset the genuine costs of implementing the systems and workflows that value-based care requires.
Additionally, providers new to ACOs, a category that disproportionately includes independent practitioners, can participate with smaller minimum patient panels than traditionally required. This recognition is important: forcing a small practice to manage risk across 5,000 patients when their existing panel is 800 patients creates untenable financial volatility. By allowing scaled participation based on realistic organization size, CMS has removed a critical participation barrier.
Risk adjustment and complex patient integration
Previous ACO models inadvertently created perverse incentives around patient risk. Providers caring for complex, costly populations faced higher benchmarks that were difficult to beat, while those with healthier populations could more easily claim savings. This dynamic discouraged providers from actively engaging with high-needs populations, counteracting the entire purpose of accountable care.
ACO LEAD addresses this through more accurate risk adjustment and enhanced integration of complex patients. CMS has recognized that caring for dual-eligible beneficiaries (those eligible for both Medicare and Medicaid), patients with behavioral health conditions, and individuals with multiple chronic diseases requires different capabilities than managing a general population. Rather than forcing complexity into a standardized framework, LEAD creates specific accommodations.
The model also includes initial planning for Medicare-Medicaid partnerships at the state level, beginning with a planning phase from March 2026 through December 2027. This represents a fundamental shift in how CMS approaches patients who experience fragmentation across two payment systems. For providers serving populations with substantial Medicaid overlap, this coordination capability will ultimately prove more valuable than any single payment mechanism.
Episode-based risk and the specialist coordination problem
A persistent challenge in earlier ACO models involved how to fairly and efficiently coordinate care with specialists. Primary care physicians felt the pressure of bearing risk for specialist-driven costs without having real influence over specialist decision-making or access to timely data about specialist activities.
ACO LEAD introduces CMS administered risk arrangements (CARA), a mechanism specifically designed to enable specialists to participate in shared risk arrangements without requiring primary care ACOs to manage complex contracting relationships. Under CARA, CMS administers the arrangement on standardized terms, and specialists can share in savings from specific episodes they help manage. This is not semantic complexity but genuine operational simplification that removes a significant barrier to specialist engagement.
As a concrete example, CMS has designed a falls prevention episode as part of the CARA framework. This reflects evidence that falls are the leading cause of injury-related hospitalization and death among seniors, and yet previous models made it difficult to coordinate systematic falls prevention across multiple providers. By creating a standardized episode structure, CMS enables ACOs to easily contract with physical therapy practices, geriatric assessment programs, and home modification services to deliver coordinated prevention.
Technology infrastructure: the foundation nobody mentions during announcements
The most striking aspect of ACO LEAD, from an operational perspective, receives minimal discussion in CMS announcements but proves absolutely essential to success: the model is explicitly designed to function with integrated data, real-time analytics, and intelligent workflow support. This is not optional infrastructure or nice-to-have functionality. It is foundational to the model’s design.
Abe Sutton addressed this directly during the AMA discussion of LEAD: previously, CMS had created the right incentive structure, but then “failed to give you data in a timely manner to let you know, all right, I need to intervene in a different manner with that patient.” This acknowledgment signals that ACO LEAD assumes participating organizations will have the technological capabilities to see patients approaching risk thresholds, identify care gaps in real time, and execute coordinated interventions before costs accumulate.
It means ACOs must be able to:
- Ingest and normalize data from multiple sources (claims, clinical records, pharmacy, lab, social determinants) into a unified patient view accessible to care teams
- Calculate risk scores and identify high-need patients prospectively, not retrospectively after costs have already been incurred
- Embed insights directly into clinician workflows so that risk information, care gaps, and recent utilization appear where physicians actually work, in their EMR or daily schedule, rather than forcing them to navigate separate portals
- Automate post-discharge workflows and event triggering, so that when a patient is hospitalized, care coordination tasks automatically generate for the care team
- Monitor utilization patterns and “leakage“ (care received outside the ACO’s preferred network) to maintain the connection between invested resources and financial performance
- Manage coding accuracy and risk stratification in a continuous, real-time manner rather than handling it as a year-end cleanup process
The capacity to do these things is not a competitive advantage in ACO LEAD but a baseline requirement. Practices that attempt to operate this model using legacy systems, manual processes, or point-solution tools bolted onto fee-for-service infrastructure will find themselves structurally disadvantaged.
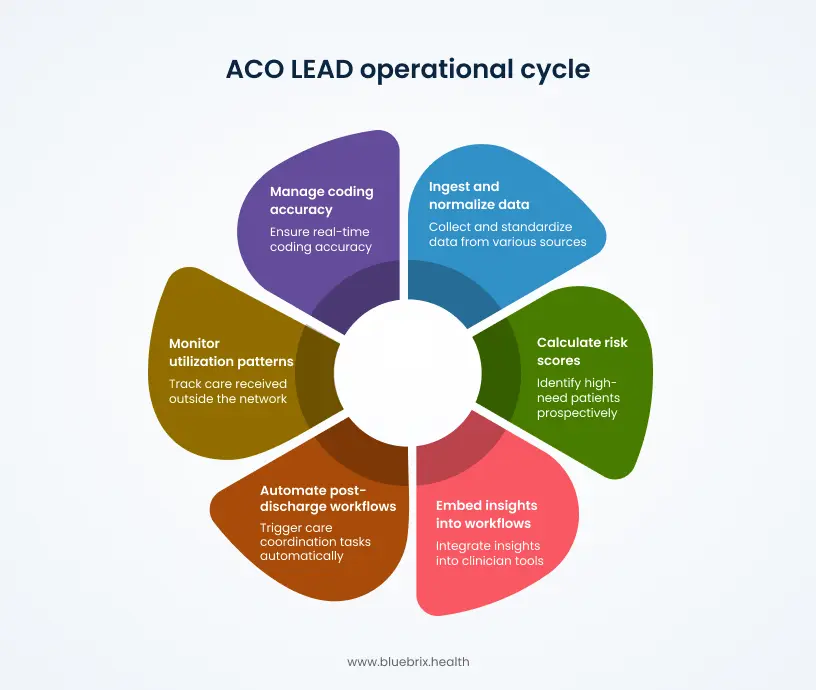
This is where care coordination orchestration platforms become essential. Organizations like blueBriX specialize in exactly this infrastructure challenge: creating a unified ecosystem where clinical data, claims information, and patient-centric analytics inform care coordination in real time, without requiring providers to operate across fragmented systems. The operational pressure of ACO LEAD where monthly prospective payments create immediate accountability for performance and where data quality directly impacts financial results makes integrated technology not just valuable but necessary.
The quality reporting evolution
ACO LEAD includes modifications to quality reporting requirements that aim to reduce administrative burden while maintaining meaningful performance measurement. The model creates focused accountability around a defined set of quality measures while allowing practices flexibility in how they achieve those targets.
Unlike models where quality reporting feels disconnected from daily clinical work, ACO LEAD is designed to integrate quality measurement into routine documentation and care delivery. This means that the clinical decisions providers make every day whether to screen for depression, manage blood pressure targets, or ensure medication reconciliation automatically generate the data needed for quality reporting rather than requiring separate, retrospective data abstraction.
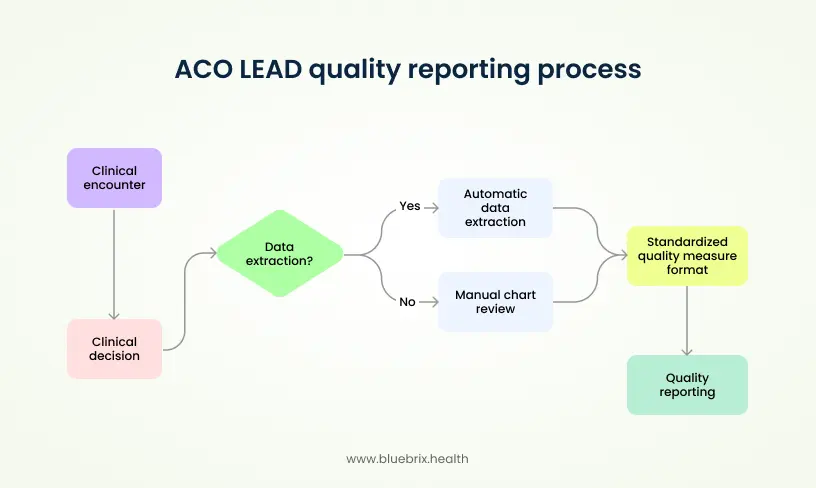
This integration depends entirely on having clinical systems capable of extracting data automatically from clinical encounters and translating it into standardized quality measure formats. The alternative manual chart review and administrative abstraction is both expensive and error-prone.
Beneficiary engagement and patient experience
While ACO LEAD fundamentally restructures the financial incentives and operational requirements for providers, it simultaneously creates new tools to engage beneficiaries themselves. Starting with the model’s launch, beneficiaries can enjoy enhanced cost-sharing benefits, including reductions in copayments for outpatient services. By 2029, the model will expand to allow beneficiaries to “buy down” their Medicare prescription drug premiums using savings generated by the ACO.
This direct link between ACO financial performance and beneficiary benefit improvements is intentional. It acknowledges that accountable care only succeeds when patients understand why they should engage with coordinated care and when they have tangible reasons to do so. A patient whose copay is reduced or whose medications cost less has a direct incentive to use the ACO’s preferred providers and to engage in preventive care rather than waiting for acute problems.
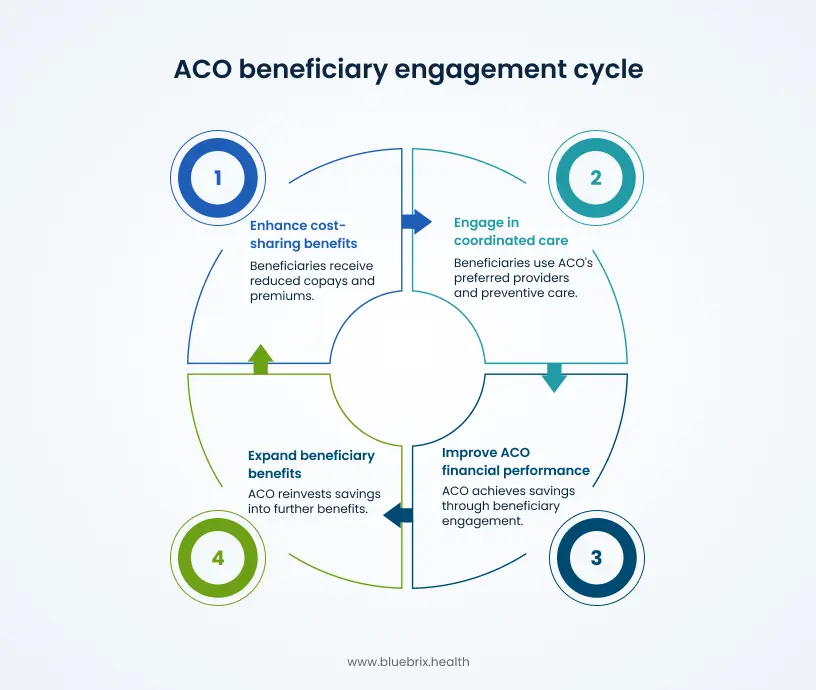
From a care coordination perspective, this also creates additional tools for outreach and engagement. Care teams can communicate clearly to patients: “By staying engaged in our care coordination program and using our network, you save money on your premiums and copays.” This value proposition is far simpler and more motivating than abstract discussions of “better outcomes.”
The geographic expansion opportunity
ACO LEAD explicitly targets geographic expansion and the participation of previously underserved markets. CMS has committed to actively recruiting rural practices, small independent practices, and practices caring for specialized or complex patient populations. For regions that have historically been overlooked in value-based care adoption, particularly rural areas, underserved urban markets, and practices focused on behavioral health, LEAD creates a genuine opportunity.
The minimum patient panel requirements are substantially lower for new entrants, the financial benchmarks include special adjustments for new ACOs, and the infrastructure investment support targets exactly the organizations most likely to lack capital for technology and hiring. If you practice in an area where value-based care has felt irrelevant or inaccessible, ACO LEAD may represent the first genuinely viable pathway to participation.
Timeline and transition planning
For providers currently in ACO REACH, the transition to ACO LEAD is direct. ACO REACH ends December 31, 2026, and ACO LEAD begins immediately afterward. This creates a specific decision window: providers must evaluate whether to continue in accountable care, remain in REACH through its final year, or return to fee-for-service. For those committed to value-based care, LEAD offers substantially more favorable terms than remaining in REACH.
For organizations currently operating under other ACO models (MSSP, Pioneer, etc.), the decision is more complex and depends on the specifics of your current arrangement and patient population. However, the general trajectory is clear: CMS is consolidating its various ACO pilot models into LEAD and expects most Medicare ACOs to eventually operate under this framework.
The critical question is not whether to participate in some form of value-based care—the financial trajectory of fee-for-service is clear. The question is whether you’ll participate strategically with adequate preparation, or reactively with inadequate infrastructure. The difference between those two approaches is substantial.
Why ACO LEAD matters now
The announcement of ACO LEAD represents CMS’s most explicit acknowledgment to date that previous value-based care models created unnecessary barriers, particularly for independent and small practices. The 10-year benchmark stability, the enhanced financial support for rural providers, the simplified specialist contracting, and the prospective payment structure are structural changes designed to make accountable care sustainable for a broader range of organizations.
For providers who have watched value-based care become increasingly dominated by large hospital systems, ACO LEAD offers a genuine alternative pathway. For practices that have attempted ACO participation and found it operationally overwhelming, the simplified framework and technology assumptions may make a second attempt worthwhile.
However, success in ACO LEAD requires honest assessment of your current capabilities. Most critically, it requires technology infrastructure robust enough to deliver real-time insights to care teams, integrate data across multiple sources, and support the workflows that actually drive coordinated care. Organizations that attempt to operate ACO LEAD with fragmented, legacy systems will find themselves unable to translate the model’s financial incentives into actual performance improvement.
The window to evaluate, prepare, and implement these capabilities is now—specifically in the first half of 2026. Practices that begin this work immediately will be positioned to launch successfully in January 2027. Those that wait will find themselves playing catch-up in an increasingly competitive value-based care marketplace.
The decision isn’t whether value-based care is your future that’s increasingly inevitable. The decision is whether you’ll be ready for ACO LEAD in January 2027, or whether you’ll be scrambling to implement it reactively.
The clock is ticking. Let’s have a conversation about where your practice stands and what readiness actually looks like.