This blog post will delve deep into the critical issue of fragmentation in US healthcare, outlining its profound impact and presenting a compelling vision for a future of truly coordinated care, with blueBriX leading the change.

The vision for US healthcare is seamless access, personalized treatment, and superior outcomes. We want patient journeys that are smooth, diagnoses that are swift and precise, and every care provider to have a complete understanding of their patient’s health history. However, everyday experience for many often falls short of this ideal. We are battling a pervasive issue: fragmented care.
What exactly is fragmented care? It’s the antithesis of integration. It’s when critical patient information is siloed across different healthcare organizations, specialties, and even within departments of the same hospital. It’s when workflows are manual, redundant, and prone to errors, causing delays, inefficiencies, and frustration for both patients and providers. Essentially, it’s a system where vital connections are missing, hindering effective care delivery.
The Root Causes of Fragmentation: Unpacking the “Why”
To effectively combat fragmentation, we must first understand its origins. It’s rarely a single culprit but rather a complex interplay of interconnected factors deeply embedded in the US healthcare landscape.
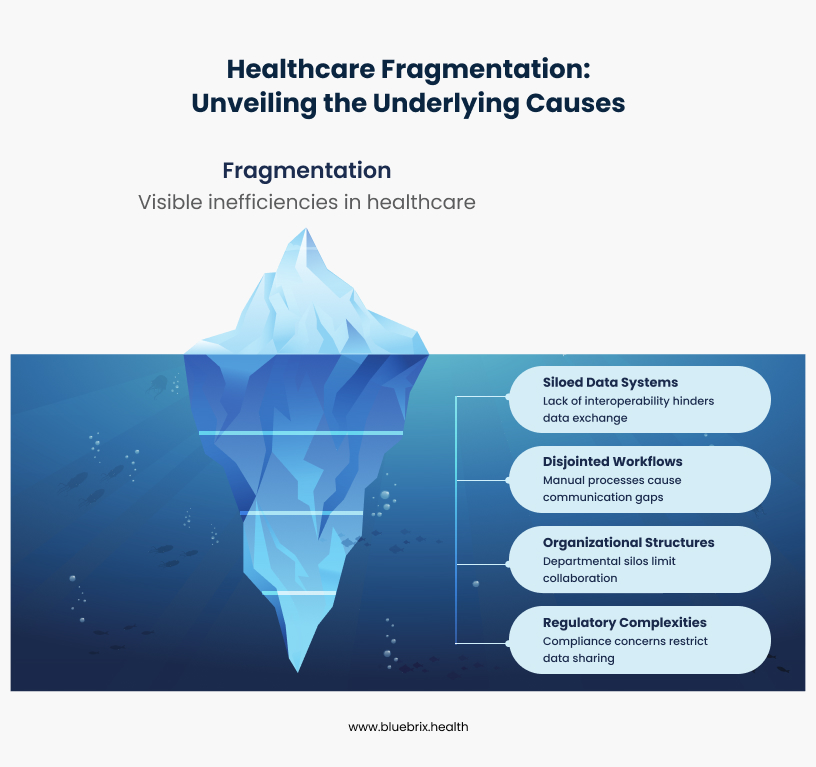
1. Siloed Data Systems
While Electronic Health Records were introduced with the promise of digitalization and efficiency, they’ve often become paradoxically part of the problem.
- Proprietary Systems and Interoperability Challenges: A significant challenge in the US is the prevalence of diverse, proprietary EHR systems from various vendors (e.g., Epic, Cerner, Meditech, athenahealth). Each vendor often uses its own data structures and formats, making it incredibly difficult for different systems to “talk” to each other seamlessly. This lack of true plug-and-play interoperability means a patient’s record in one hospital’s EHR often cannot be easily accessed or understood by another hospital using a different system, or even by an outpatient clinic using a separate EHR.
- Lack of Standardization in Data Formats: Even when data is digital, the absence of universal, strict standards for how clinical information (like lab results, medication lists, or diagnoses) is represented further exacerbates the problem. Imagine trying to integrate patient data where one system records blood pressure as “BP,” another as “Blood Pressure,” and a third uses “Systolic/Diastolic” in separate fields – the data simply isn’t consistently structured for easy exchange.
- The “My System” Mentality and Data Blocking: A cultural and sometimes even competitive hurdle exists where individual healthcare facilities or health systems prioritize their own internal systems and data “ownership” over a collaborative, system-wide approach to data sharing. The issue of information blocking, where healthcare providers or IT vendors knowingly and unreasonably interfere with the access, exchange, or use of electronic health information, has been a significant concern, leading to regulatory efforts by the ONC (Office of the National Coordinator for Health Information Technology) to curb this practice.
2. Disjointed Workflows and Communication Gaps
Beyond data, the way healthcare is delivered is often riddled with inefficiencies:
- Manual Processes and Paper-Based Handoffs: Despite technological advancements, many critical patient handoffs, referrals, and information exchanges still rely on manual, paper-based processes or faxes, even in large health systems. This is not only time-consuming but also highly susceptible to errors, delays, and lost information, such as missed follow-up appointments after an emergency room visit.
- Lack of Centralized Communication Platforms: Healthcare teams, even within the same organization, often communicate through fragmented channels – phone calls, unsecured emails, faxes, and even personal messaging apps. This lack of a secure, centralized, and auditable platform makes it challenging to track conversations, ensure information reaches the right person at the right time (e.g., during shift changes), and maintain a comprehensive communication log.
- Inefficient Scheduling and Referral Management: Booking appointments across multiple specialties or referring a patient to an external specialist can be a cumbersome, manual process involving phone calls, faxes, and long wait times. This leads to delays in care, patient frustration, and revenue leakage for practices.
3. Organizational Structures and Cultural Barriers
The very structure and culture within US healthcare organizations can inadvertently contribute to fragmentation:
- Departmental Silos and Lack of Cross-Functional Collaboration: Departments often operate in isolation, focusing on their specific functions rather than viewing the patient journey holistically. For example, a hospital’s discharge planning team might not have direct, real-time communication with the patient’s primary care provider, leading to poor post-discharge follow-up.
- Resistance to Change and Adoption of New Technologies: Implementing new systems and workflows requires significant change management. Resistance from staff due to fear of the unknown, a perceived increase in workload, lack of adequate training, or simply a preference for established (even if inefficient) methods can be a major barrier.
- Insufficient Training and Support for Digital Transformation: Even with the best technology, inadequate training and ongoing support can lead to low adoption rates, user frustration, and a failure to realize the full potential of digital tools, resulting in underutilized features and continued reliance on old, fragmented processes.
4. Regulatory and Compliance Complexities
While regulations like HIPAA (Health Insurance Portability and Accountability Act) are vital for protecting patient privacy and ensuring data security, their complexity can sometimes inadvertently create perceived barriers to legitimate data sharing. Healthcare organizations often err on the side of caution, leading to reluctance in sharing information even when legally permissible and clinically beneficial. Efforts like the 21st Century Cures Act aim to clarify and enforce interoperability and prevent information blocking.
The Consequences of Fragmented Care
The cumulative impact of these fragmented systems and workflows extends far beyond mere inconvenience. It can have severe, even life-threatening, consequences across the entire healthcare ecosystem.
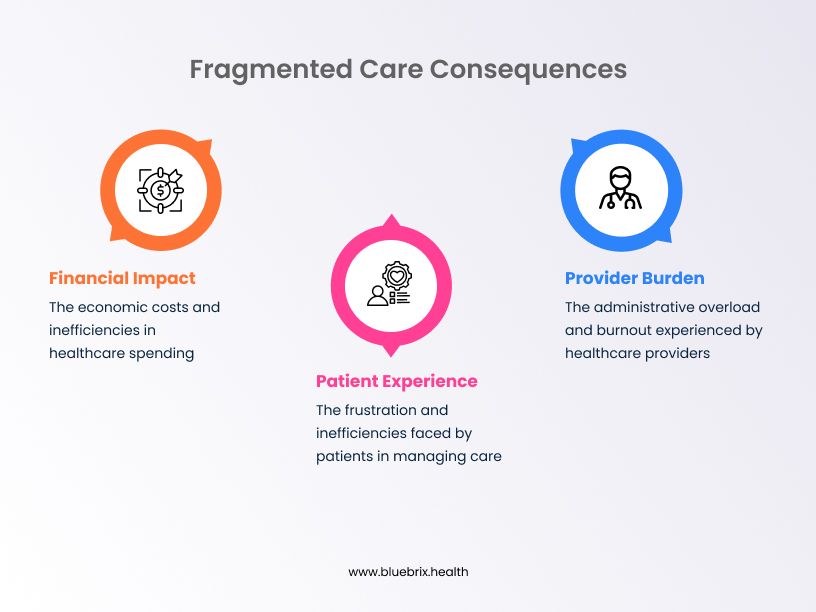
For Patients
- Delayed or Missed Diagnoses: Critical information scattered across different providers can lead to a delay in connecting crucial symptoms or test results, postponing essential diagnoses and interventions. A patient visiting an ER might have vital information in their PCP’s EHR that the ER physician can’t access, leading to an incomplete clinical picture.
- Medication Errors and Adverse Events: Without a consolidated, real-time view of a patient’s complete medication list, allergies, and existing conditions, the risk of prescribing errors, adverse drug interactions, or contraindications increases significantly. This is a leading cause of preventable harm in healthcare.
- Duplicative Tests and Unnecessary Procedures: When information isn’t readily shared, patients frequently undergo repeated diagnostic tests (e.g., blood work, imaging scans like MRIs or CTs) or procedures simply because the new provider isn’t aware of previous ones. This leads to unnecessary costs for patients and payers, increased radiation exposure, and discomfort.
- Poor Adherence to Treatment Plans: Patients can become overwhelmed and disengaged when their care plan is disjointed, receiving conflicting advice or struggling to coordinate appointments across multiple specialists. This often leads to lower adherence to prescribed treatments and ultimately, poorer health outcomes.
- Erosion of Trust and Dissatisfaction: The constant friction, inefficiency, and feeling of being “just a number” erode patient trust in the healthcare system. This leads to dissatisfaction, negative patient reviews, and a reluctance to seek necessary care, impacting patient loyalty and health-seeking behaviors.
For Healthcare Providers
- Increased Administrative Burden and Documentation Overload: A significant portion of a clinician’s day can be consumed by administrative tasks – searching for patient information, chasing down lab results, calling other providers, and inputting redundant data into multiple systems – instead of focusing on direct patient care. This is a major driver of physician burnout.
- Missed Patient Information and Incomplete Records: The inability to access a complete and accurate patient history due to fragmented records can lead to suboptimal clinical decisions, increased diagnostic uncertainty, and potential safety risks, especially in emergency situations or complex cases.
- Communication Breakdowns and Misunderstandings: Ambiguous, delayed, or missed communication between care team members (e.g., during patient handoffs from the ICU to a general ward, or between primary care and specialists) can result in critical errors, impacting patient safety and care quality.
- Legal and Compliance Risks: Incomplete documentation, failure to share critical information, or breaches in data security due to uncontrolled sharing methods can expose healthcare organizations to significant legal liabilities, malpractice claims, and non-compliance penalties from regulatory bodies.
- Burnout and Decreased Job Satisfaction: The constant struggle against inefficient, fragmented systems, coupled with overwhelming administrative tasks, takes a heavy toll on healthcare professionals. This leads to high rates of burnout, compassion fatigue, and a decline in overall job satisfaction, contributing to workforce shortages.
For Healthcare Organizations
- Financial Losses Due to Inefficiency and Rework: The costs associated with duplicated services, wasted resources (e.g., unnecessary supplies for repeated tests), administrative overhead due to manual processes, and penalties for poor outcomes (e.g., readmission penalties) can be substantial, directly impacting an organization’s bottom line.
- Reduced Patient Throughput and Capacity Issues: Inefficient workflows lead to longer wait times for appointments, delayed patient discharges, and ultimately, a reduced capacity to serve more patients effectively, impacting revenue and access to care.
- Damaged Reputation and Loss of Patient Loyalty: In an increasingly competitive and patient-centric healthcare market, organizations known for fragmented, disjointed care risk losing patient trust and loyalty to competitors offering a more seamless and integrated experience. This can directly impact patient volume and market share.
- Hindered Innovation and Growth: The energy and resources spent on managing fragmented, legacy systems detract from an organization’s ability to innovate, adopt new value-based care models, invest in advanced technologies, and strategically expand its services to meet evolving community needs.
But there is a good news! There’s a powerful and growing movement towards coordinated care – a holistic, integrated approach that seeks to bridge these gaps, ensuring that all aspects of a patient’s care are connected and aligned.
Strategies for Eliminating Fragmentation
The path to coordinated care requires a strategic, multi-pronged approach, leveraging advanced technology, streamlining processes, and fostering a deeply collaborative culture. This is where blueBriX steps in, as your dedicated partner in building a truly connected and efficient healthcare ecosystem across the United States.
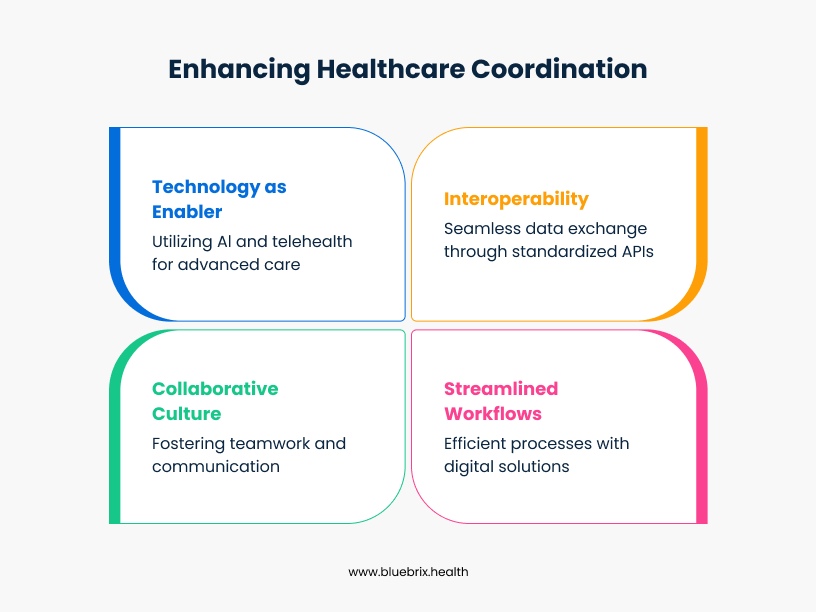
1. The Power of Interoperability: Breaking Down Data Silos
This is the foundational element of connected care. Without the ability to seamlessly exchange patient information, true coordination remains elusive.
- The Role of Standardized APIs (Application Programming Interfaces): APIs act as sophisticated bridges between different software applications, allowing them to communicate and share data securely and efficiently. By adopting standardized APIs, healthcare systems can unlock their data, making it programmatically accessible to authorized users and applications, moving beyond batch file transfers to real-time data exchange.
- FHIR (Fast Healthcare Interoperability Resources) as New Standard: FHIR is rapidly emerging as the global and de facto standard for exchanging healthcare information electronically. It’s designed to be flexible, developer-friendly, and to facilitate real-time data sharing through modular “resources” (e.g., Patient, Observation, Medication). The 21st Century Cures Act strongly promotes FHIR as the basis for interoperability, mandating its adoption for certified EHRs.
- Data Warehousing and Analytics for Holistic Views: Beyond real-time exchange, consolidating and normalizing data from various disparate sources into a central, cloud-based data warehouse (often a Health Data Platform) enables powerful population health analytics. This allows organizations to gain a holistic, longitudinal view of patient populations, identify trends (e.g., chronic disease prevalence), stratify risk, and make data-driven decisions for improving care delivery and population health management initiatives.
- Centralized Patient Portals and Shared Records: Empowering patients with a single, secure, and user-friendly portal to access their complete health records, schedule appointments, request refills, and communicate with their care team fosters transparency and active participation in their own care. Initiatives like the CommonWell Health Alliance and Carequality in the US are working to establish networks for shared medical records among participating organizations.
2. Streamlining Workflows for Seamless Coordination
Technology must be strategically applied to transform disjointed, manual processes into smooth, integrated workflows that follow the patient’s journey.
- Digital Patient Intake and Onboarding: Moving away from clipboards and paper forms, digital intake solutions streamline the patient registration process, capture accurate demographic and clinical information upfront, and integrate it directly into the patient’s electronic record, reducing administrative burden and errors.
- Automated Appointment Scheduling and Reminders: Advanced online scheduling platforms, often integrated with EHRs, reduce no-shows, optimize clinic capacity, manage waitlists, and provide convenience for patients through automated text or email reminders.
- Electronic Referrals and Consultations: Secure, integrated electronic referral systems ensure that patient information, clinical notes, and specific referral questions are transmitted seamlessly and securely to the appropriate specialist, reducing delays, lost paperwork, and ensuring proper handoffs.
- Secure Messaging and Collaboration Platforms: Integrated communication tools within EHRs or dedicated, HIPAA-compliant platforms allow care teams (e.g., physicians, nurses, social workers, case managers) to communicate securely, in real-time, about patient care. This ensures everyone is on the same page, especially during complex cases or transitions of care.
- Task Management and Workflow Automation Tools: Automating repetitive administrative tasks, such as insurance eligibility verification, prior authorizations, prescription refills, or even patient outreach for preventive screenings, frees up staff time, reduces errors, and accelerates critical processes.
3. Fostering a Culture of Collaboration and Communication
Technology is merely an enabler; a deeply collaborative culture is the essential engine that drives its successful adoption and sustained impact.
- Cross-Departmental Training and Workshops: Breaking down organizational silos requires a conscious and sustained effort. Regular training and workshops that bring together different departments to understand each other’s roles, challenges, and the collective benefits of integrated workflows can be transformative. This includes interdisciplinary grand rounds and shared learning opportunities.
- Establishing Clear Communication Protocols: Defining standardized communication channels, escalation procedures, and expectations ensures that critical information flows efficiently, effectively, and transparently across the entire care continuum, from inpatient to outpatient settings.
- Promoting a Patient-Centric Mindset: Reorienting the entire organization around the patient’s comprehensive journey, rather than individual departmental or specialist functions, helps foster a collective commitment to coordinated care and shared accountability for patient outcomes.
4. Leveraging Technology as an Enabler (Beyond Interoperability)
The ongoing digital health revolution offers even more powerful tools to enhance and solidify coordinated care, pushing beyond basic data exchange.
- AI and Machine Learning for Predictive Analytics and Risk Stratification: AI algorithms can analyze vast amounts of structured and unstructured patient data (e.g., EHR notes, lab results, claims data) to identify at-risk patient populations for specific conditions (e.g., readmissions, chronic disease exacerbations), predict potential health issues, and enable proactive interventions. This shifts healthcare from a reactive “fix-it” model to a proactive, preventative approach.
- Telehealth and Remote Patient Monitoring for Continuity of Care: These technologies extend care beyond the traditional clinic walls, enabling virtual consultations, continuous monitoring of vital signs and biometric data for patients with chronic conditions, and proactive management of health. This is particularly vital for improving access to care in rural or underserved areas of the US.
- Mobile Health Applications for Patient Engagement: User-friendly, secure mobile apps empower patients to actively manage their appointments, access their health information, track their progress, adhere to medication schedules, and communicate directly and securely with their care team, significantly increasing engagement and self-management capabilities.
blueBriX’s Role in Building a Coordinated Care Ecosystem
At blueBriX, we understand these intricate challenges within the US healthcare landscape intimately. Our mission is to empower healthcare organizations across the nation to overcome fragmentation, improve patient outcomes, and achieve operational excellence.
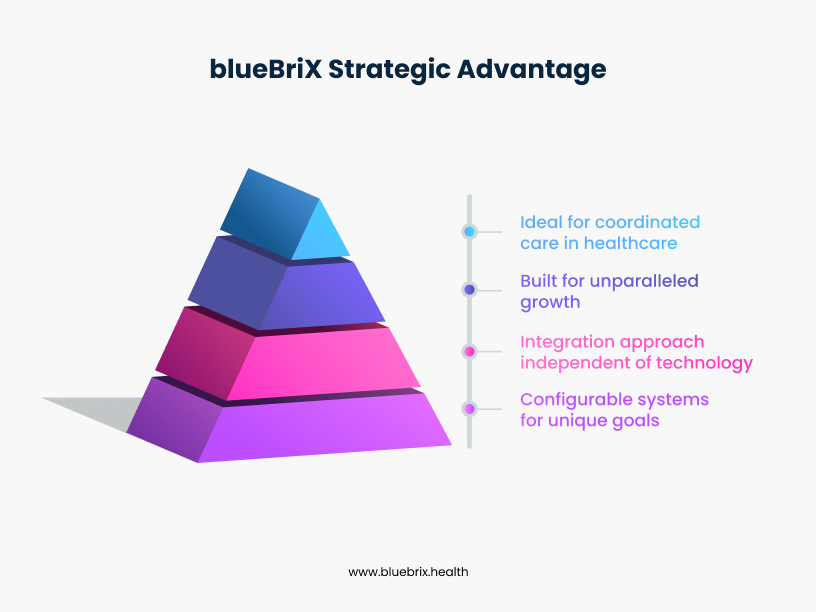
How blueBriX Addresses Key Fragmentation Challenges
blueBriX provides a comprehensive platform specifically designed for digital health solutions, offering modularity, deep interoperability, and a relentless focus on user-centric design. Our solutions directly address the very pain points we’ve discussed:
- Seamless EHR & HIS Integration: blueBriX is engineered to integrate effortlessly with virtually all major US Electronic Health Records (EHRs) and Hospital Information Systems (HIS), including Epic, Cerner, Meditech, and athenahealth. We support open APIs, including FHIR standards, and provide access to over 2,000 APIs to consolidate patient information and ensure data consistency across disparate systems. This directly tackles the “siloed data systems” issue by creating a unified patient view.
- Advanced Care Coordination Platform: Our customizable care management solution offers robust features like collaborative care planning, dynamic care pathway adjustments based on patient needs, and real-time insights into patient progress. This enables seamless, multi-disciplinary collaboration among care teams, streamlining workflows, and eliminating communication gaps across the care continuum.
- No-Code App Builder for Tailored Workflows: Our intuitive, enterprise-grade low-code/no-code platform empowers healthcare organizations to rapidly build and deploy highly tailored applications and workflow solutions without extensive, costly engineering expertise. This allows for rapid customization to address specific organizational needs (e.g., unique discharge processes, specialized referral tracking) and fosters agility in adapting to evolving healthcare requirements.
- AI Agents for Optimized Workflows and Clinical Decision Support: blueBriX PULSE, our suite of intelligent AI agents, are designed to collaborate across workflows. They can automate mundane tasks (e.g., appointment scheduling, insurance eligibility verification), reduce administrative burden on staff, and provide intelligent clinical decision support at the point of care, significantly enhancing efficiency and accuracy.
- Robust Population Health Management and Predictive Analytics: blueBriX provides powerful tools to aggregate and analyze patient data to identify at-risk patient groups, enhance preventative care through predictive analytics (e.g., identifying patients at high risk for readmission), and optimize resource allocation across a population. This empowers organizations to succeed in value-based care models and move towards a proactive rather than reactive model of care.
- Uncompromising Security and Compliance: We ensure all integrated modules and our platform adhere to the strictest US healthcare industry standards and regulations, including HIPAA, HITECH, and the 21st Century Cures Act information blocking rules. This provides absolute peace of mind regarding data security, patient privacy, and regulatory compliance, which is paramount in the US healthcare environment.
Real-World Impact: Imagine a patient who arrives at a blueBriX-enabled facility. Their digital intake is smooth and expedited. Their entire medical history, including relevant data from previous providers in different systems and SDOH, is instantly accessible to their current care team. Their specialist consultation is seamlessly scheduled with real-time availability. Their care team can securely message each other about their progress and receive AI-driven alerts for potential risks. This translates directly into tangible benefits for our clients: significantly fewer no-shows, faster patient check-ins, reduced readmissions, and ultimately, a more positive and effective healthcare experience for everyone.
The Future of Coordinated Care: A Vision for Connected Health
The journey to eliminate fragmented systems and workflows in US healthcare is an ongoing evolution, but the destination is clear and compelling: a truly integrated, patient-centric healthcare system.
We envision a future where:
- Information Flows Freely and Securely: Patient data is accessible to authorized providers whenever and wherever it’s needed, across the care continuum, empowering informed decision-making and significantly reducing preventable medical errors.
- Care is Proactive, Personalized, and Preventative: Through sophisticated analytics, AI, and continuous monitoring, healthcare shifts definitively from a reactive “sick care” model to a proactive, precision health approach, anticipating patient needs and promoting lifelong wellness.
- Patients are Empowered Partners: Patients are active, informed participants in their own health journeys, with convenient access to their health information, intuitive tools for self-management, and direct, secure communication channels with their entire care team.
- Providers Thrive in an Efficient Environment: Clinicians spend significantly less time on administrative tasks and more quality time on direct patient care, leading to improved efficiency, reduced burnout, and renewed passion for care.
- Healthcare is Equitable and Accessible: Digital solutions bridge geographical, socioeconomic, and infrastructural barriers, ensuring that high-quality, coordinated care is accessible to all Americans, from major metropolitan areas to remote rural communities.
This is a future where “connecting the dots” is the fundamental and unwavering principle guiding every aspect of healthcare delivery in the United States.
Conclusion: Embracing the Journey Towards Seamless Care
The challenges posed by fragmented healthcare systems in the US are significant, complex, and deeply ingrained. However, the solutions are not only within our grasp but are actively being deployed and refined. By strategically embracing true interoperability, rigorously streamlining workflows, fostering a deeply collaborative and patient-centric culture, and leveraging cutting-edge digital health technologies, healthcare organizations can profoundly transform the patient experience, empower their dedicated providers, and achieve demonstrably better health outcomes for entire populations.
Are you ready to eliminate the silent epidemic of fragmented care within your organization and embark on a transformative journey towards a truly coordinated, efficient, and patient-centered healthcare future?