IV pushes and infusions are clinically vital—but financially risky when mishandled. Denied IV claims are quietly draining revenue, bloating A/R days, and overloading RCM teams with avoidable rework. Whether you're on the frontlines of documentation, managing billing operations, or steering your organization's financial strategy, understanding key CPT coding conflicts is critical. In this blog, we unpack the top 5 CPT conflicts sabotaging your IV claims—and show you how to stop the revenue bleed before it gets worse.

IV services involve high volumes and come with built-in complexity. A single patient encounter can include multiple medications, different administration methods (like pushes and infusions), and varying time durations—all of which add layers to the coding process. When small errors occur across a large number of claims, the financial impact can add up quickly.
Managing IV claims accurately isn’t just about billing—it plays a key role in maintaining a healthy revenue cycle. Clean claims help ensure quicker reimbursements, lower A/R days, and more financial stability. On the other hand, frequent denials can slow down revenue flow and shift focus away from patient care toward administrative rework.
Why IV Claim Accuracy Matters More in the Value-Based Care Era
Since the focus is shifting from fee-for-service to value-based care (VBC), optimizing reimbursement for IV services is crucial for immediate financial health.
Denials & VBC Metrics
Claim denials, particularly those stemming from CPT conflicts, directly undermine your ability to succeed in Value Based Care arrangements. Persistent denials indicate inefficiencies that can lead to higher administrative costs, reduced patient satisfaction (due to billing issues), and a negative impact on quality metrics if resources are perpetually tied up in rework rather than patient care improvements. Payers in Value Based Care models are looking for efficiency and quality, and a high denial rate signals the opposite.
Quality & Financial Health
Accurate and timely reimbursement from clean claims helps create financial stability, allowing organizations to support quality initiatives, strengthen patient safety efforts, and invest in programs that improve outcomes. When revenue is more predictable, it’s easier to allocate resources toward areas that support value-based care goals, like preventive services, chronic care management, and population health efforts.
Sustainable Care Delivery
Effective Revenue Cycle Management for IV services is not just about maximizing profit; it’s about ensuring the financial viability required to deliver high-quality, sustainable patient care under Value Based Care arrangements. By minimizing denials and optimizing revenue, healthcare organizations can maintain the operational capacity to meet the demands of value-based contracts, fostering a healthier patient population and a stronger financial foundation.
Top 5 CPT Conflicts Derailing Your IV Claims
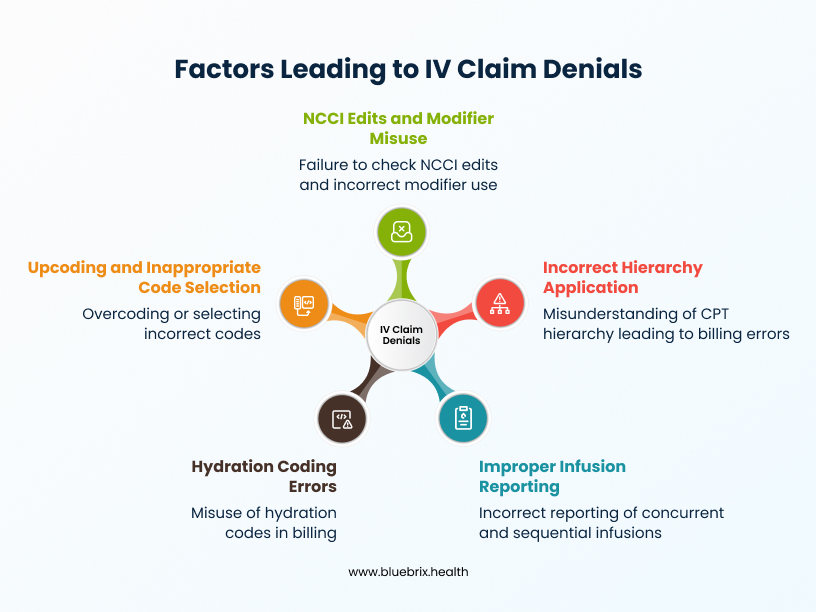
The top 5 CPT conflicts that are most commonly undermining IV push and infusion claims stem from misunderstandings of, hierarchy, and payer edits. These errors can lead to denials, underpayments, or even accusations of improper billing. Here are the most critical conflicts:
Conflict 1: Incorrect Application of the Hierarchy for Initial Services
- The Challenge: CPT guidelines are very specific about how to report initial IV services. Only one initial service code (e.g., for hydration, therapeutic infusion, or chemotherapy) should be reported per patient encounter per day. This rule is designed to prevent over-billing for the initial setup and administration. An exception exists if a second IV site is medically necessary, but this requires explicit documentation and appropriate modifier use (e.g., modifier -59 for a distinct procedural service). The established hierarchy dictates which service takes precedence when multiple types of IV administrations occur:
- Chemotherapy services are considered primary to therapeutic, prophylactic, and diagnostic services.
- Therapeutic, prophylactic, and diagnostic services are primary to hydration.
- Infusions (longer duration) are primary to pushes (bolus administration), which are primary to injections.
Understanding and applying this hierarchy correctly is crucial for accurate billing.
- Why Claims Die: Claims frequently face denials when organizations report multiple initial codes without clear, documented medical necessity for each. Common errors include billing an initial hydration code alongside an initial therapeutic infusion code when only one initial service is truly warranted, or failing to follow the established hierarchy, leading to the primary service being under-reimbursed or denied because a secondary service was incorrectly coded as initial.
- Impact: This conflict directly results in denials for “duplicate services” or “incorrect initial service.” It leads to significant underpayment, as payers will only reimburse for one initial service based on their interpretation of the hierarchy, forcing the organization to absorb the cost of the other incorrectly billed initial services. This also increases rework and appeal efforts.
- Solution: To prevent denials related to incorrect application of the initial service hierarchy, providers and administrators must ensure coders strictly follow CPT’s hierarchy rules, apply only one initial service code per encounter unless medically justified, and use modifiers like -59 appropriately when billing distinct services. blueBriX streamlines this process with a built-in hierarchy logic engine, smart modifier suggestions, real-time documentation prompts, and automated pre-bill audits—ensuring compliant coding, minimizing denial risk, and protecting reimbursement.
Conflict 2: Improper Reporting of Concurrent and Sequential Infusions
- The Challenge: Distinguishing between concurrent and sequential infusions, and applying the correct CPT codes and modifiers, is a complex area. Concurrent infusions (e.g., CPT 96368 for concurrent therapeutic infusion) can only be reported once per day, regardless of how many additional substances are administered simultaneously. This code covers the additional complexity of running multiple infusions at the same time. Sequential infusions, on the other hand, involve administering a new substance or drug after a prior infusion has completed. While CPT 96376 can be used for a sequential IV push of the same drug in certain facility situations, generally, a new substance is required for a sequential infusion code.
- Why Claims Die: A common error is over-reporting concurrent infusions, attempting to bill CPT 96368 multiple times for different concurrent substances on the same day. Another frequent mistake is incorrectly reporting sequential codes for the same substance when it should be considered part of the initial infusion, or billing sequential codes multiple times for events that are not distinct sequential administrations. This often stems from a misunderstanding of what constitutes a “new” substance or a truly separate sequential event.
- Impact: These errors lead to denials for “duplicate reporting” or “incorrect bundling.” Payers will often bundle these services, paying only for the initial or primary infusion and denying the concurrent or sequential codes. This results in significant under-reimbursement and can trigger audits due to patterns of incorrect billing, potentially leading to recoupments.
- Solution: Proper training, clear infusion documentation—including timestamps, drug names, and sequencing—and vigilant bundling awareness are critical. blueBriX simplifies this complexity with intelligent infusion mapping, automatic CPT code validation, and real-time documentation guidance that distinguishes concurrent from sequential events. The platform also flags duplicate or bundled services before claims go out, reducing denials and safeguarding revenue integrity.
Conflict 3: Hydration Coding Errors
- The Challenge: Hydration codes (CPT 96360 for initial hydration infusion, and 96361 for each additional hour) are specifically for the administration of fluids for the purpose of rehydration. Their use is highly scrutinized by payers, and there are strict guidelines on when they can be billed. They should not be used:
- When fluids are administered simply to keep the vein open (KVO) or to maintain IV access for future use. These are considered incidental to the primary service or part of routine care.
- For infusions that last less than 31 minutes, as CPT guidelines typically require a minimum duration for infusion codes.
- Concurrently with other therapeutic or chemotherapy infusions, or as a free-flowing IV during these administrations, as the hydration is generally considered incidental to the primary therapeutic service.
- Why Claims Die: Claims for hydration are frequently denied when documentation fails to clearly support the medical necessity for rehydration (e.g., signs of dehydration, patient symptoms). Missing or unclear start and stop times for hydration infusions are also major culprits.
- Impact: Hydration coding errors lead to widespread denials and potential recoupments. Since hydration codes often have lower reimbursement rates than therapeutic infusions, incorrect billing not only leads to denials but also represents a missed opportunity for appropriate reimbursement when a therapeutic infusion was indeed performed but incorrectly coded as hydration.
- Solution: blueBriX reinforces compliance by guiding clinicians through structured documentation templates that capture all required hydration details, automatically validating duration thresholds, and flagging improper code use based on context. This ensures appropriate code selection, eliminates incidental billing errors, and protects revenue from unnecessary denials or audits.
Conflict 4: Failure to Check NCCI Edits and Modifier Misuse
- The Challenge: The National Correct Coding Initiative (NCCI) edits are a crucial component of Medicare’s payment policies and are widely adopted by commercial payers. NCCI edits identify code pairs that should not be billed together (mutually exclusive edits) or where one service is considered a component of another (comprehensive/component edits). Failure to review these edits before claim submission leads to improper code pairings. Furthermore, the correct application of modifiers (e.g., -25, -59, -XU, -XP, -XS, -XU) is essential to bypass certain NCCI edits when clinically appropriate and documented.
- Why Claims Die: Claims are automatically denied when submitted with code combinations that violate NCCI edits without the appropriate modifier. For example, some code combinations like CPT 96375 (therapeutic, prophylactic, or diagnostic injection) with 96360 (initial hydration infusion) might be disallowed by NCCI edits unless a specific modifier is used to indicate a distinct service. Incorrect modifier use, or the complete absence of a required modifier, is a pervasive reason for claim rejections, as payers interpret these as incorrect bundling or duplicate billing.
- Impact: This conflict results in a high volume of automatic denials, requiring significant manual intervention for correction and resubmission. It directly impacts cash flow due to delayed payments and increases administrative costs associated with denial management and appeals. Persistent errors can also lead to payer audits and potential penalties.
- Solutions: Coders should be trained to differentiate between mutually exclusive and component services, and to use modifiers like -59 or its subsets (-XS, -XU, etc.) only when distinct procedural circumstances exist. blueBriX automates this layer of compliance with built-in NCCI edit checks that run in real time during claim generation. The platform intelligently suggests correct modifiers based on documentation context and blocks claims with invalid code pairings, drastically reducing downstream rework, denials, and audit risk.
Conflict 5: Upcoding and Inappropriate Code Selection
- The Challenge: This isn’t just about mistakenly choosing the wrong code—it’s about the deeper systemic issues that lead to patterns of overcoding or misrepresentation. In the high-pressure environment of IV therapy billing, where services often overlap and time tracking gets murky, it’s easy for coding to drift from what’s supported in documentation. This includes subtle but critical missteps like inflating service duration, misclassifying administration methods (e.g., coding a prolonged infusion instead of a push), or defaulting to higher-complexity codes in ambiguous cases.
- Why Claims Die: Claims are flagged and denied when the billed code does not align with the clinical documentation. For example, billing a complex therapeutic infusion when only a simple IV push was administered, or consistently billing the highest level of an Evaluation and Management (E/M) code regardless of the actual patient encounter’s complexity, raises red flags. Payers use sophisticated algorithms to detect patterns of upcoding, which can trigger extensive audits, investigations, and severe penalties.
- Impact: This is a high-risk conflict that can lead to not only denials and recoupments but also serious legal ramifications, including accusations of improper billing or even fraud. Organizations face significant financial penalties, reputational damage, and increased administrative burden from responding to audits and investigations.
- Solution: Regular audits, peer reviews, and feedback loops are essential to identify trends and correct behaviors early. blueBriX supports this with AI-assisted code validation, real-time documentation-to-code matching, and alerts that flag inconsistencies between chart notes and selected CPT codes. By embedding compliance into the workflow, blueBriX helps providers bill accurately, reduce audit exposure, and maintain payer trust.
Strategies for Claim Survival & RCM Optimization
Addressing these CPT conflicts requires a multi-pronged approach involving collaboration across clinical, coding, and administrative departments.
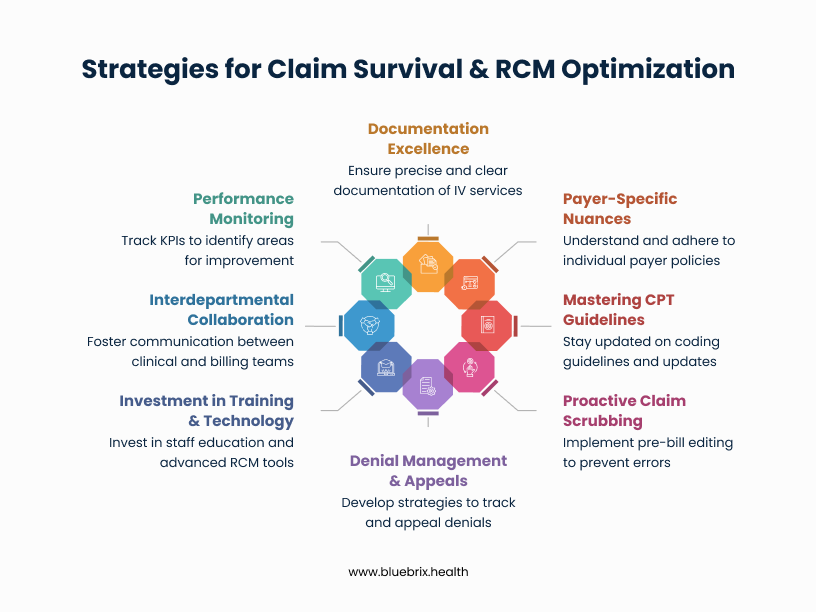
- Documentation Excellence: This cannot be overstressed. Ensure precise start and stop times for all infusions and pushes. Clearly document the substance administered, including dosage, route, and the specific medical necessity for the IV service. If it’s not documented, it’s as if it never happened in the eyes of a payer.
- Payer-Specific Nuances: While general CPT guidelines apply, individual payers often have unique policies or interpretations. Clinicians should be aware of common payer-specific requirements that impact IV services for their patient population.
- Mastering CPT Guidelines: Continuous education on the latest CPT updates, NCCI (National Correct Coding Initiative) edits, and specific nuances for IV services is non-negotiable. Similarly, regular training sessions and access to coding resources are vital.
- Proactive Claim Scrubbing: Implement robust pre-bill editing and claim scrubbing processes. Utilize software that can flag potential CPT conflicts, missing modifiers, or documentation gaps before claims are submitted. This front-end prevention saves immense time and resources compared to post-denial appeals.
- Denial Management & Appeals: Develop efficient processes for tracking, analyzing, and appealing denials. Identify trends in denials for IV services to pinpoint systemic issues and implement corrective actions. A strong appeal strategy can recover significant lost revenue.
- Investment in Training & Technology: Recognize the significant return on investment from investing in comprehensive staff education (for both clinical and RCM teams) and advanced RCM technology, including platform built EHR systems that support accurate coding and documentation.
- Interdepartmental Collaboration: Foster seamless communication and collaboration between clinical departments, coding specialists, and billing teams. Regular meetings to discuss denial trends and process improvements can bridge gaps and prevent recurring errors.
- Performance Monitoring: Implement key performance indicators (KPIs) specifically for IV claim denial rates. Regularly monitor these metrics to identify areas of improvement, track the effectiveness of interventions, and ensure accountability across departments.
Reduce Denials with blueBriX
Outsourcing your IV claim management to blueBriX means tapping into a specialized RCM team that understands the nuances of infusion billing, CPT hierarchies, and payer-specific rules. Our experts proactively identify and correct coding errors, ensure accurate application of modifiers, and validate documentation for medical necessity before claims go out—drastically reducing denials and rework. From auditing complex concurrent/sequential infusions to handling appeal strategies for high-risk denials, blueBriX delivers end-to-end revenue cycle support that improves reimbursement, accelerates cash flow, and keeps your organization compliant and audit-ready.
Don’t let CPT conflicts drain your revenue.