Scaling behavioral health across multiple locations is complex especially when clinical quality and regulatory compliance can’t be compromised. This blog explains why centralizing scheduling and documentation is essential for sustainable growth of multi-location behavioral health clinics.

As behavioral health organizations expand to meet growing demand, the complexity of managing care across multiple sites has intensified. Leaders face mounting pressure to scale and do so in a way that preserves clinical quality, operational agility, and regulatory compliance. In this context, the question is no longer if centralization is necessary, it’s how quickly and efficiently it can be implemented. Let’s explore the challenges of decentralization, benefits of centralization, and most-importantly, a roadmap to implementing a purpose-built behavioral health EHR for centralized scheduling and documentation.
Challenges of Decentralized Behavioral Health Systems
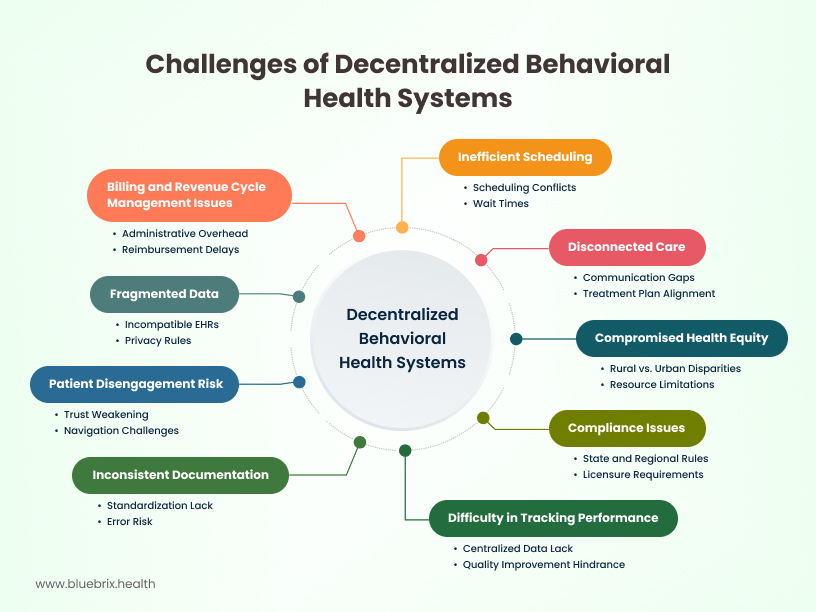
Imagine a scenario where a client seeks consistent therapy across your network, perhaps transitioning from an intensive outpatient program at one clinic to individual sessions at another. Without a unified system, their journey becomes a labyrinth of duplicated paperwork, disjointed communication, and the frustrating need to retell their story. This undermines their care experience and reveals cracks in operational continuity.
What looks like minor friction at the surface often translates into deeper, systemic issues across locations. A few are listed below.
Disconnected care: When each location operates independently, it’s harder to coordinate care across inpatient, outpatient, and community settings. Patients can fall through the cracks during transitions, especially when clinical teams don’t communicate or align on treatment plans.
Fragmented data: Incompatible EHRs, privacy rules, or lack of shared workflows can block the flow of vital clinical information between sites. As a result, providers may lack complete patient histories, which can lead to redundant or conflicting care.
Patient disengagement risk: Patients often see different providers at different locations, weakening trust and continuity in care. Severely ill or high-needs patients may struggle to navigate complex systems, increasing the risk of disengagement or non-adherence.
Compromised health equity: Rural or underserved sites often lag urban centers in both care quality and access. Some locations may have fewer trained staff, limited beds, or inadequate outpatient support—resulting in lower care standards and early discharges.
Compliance issues: Providers must navigate different state or regional rules on licensure, documentation, and reporting—slowing down service delivery and increasing risk exposure.
Inconsistent documentation: Lack of standardized processes leads to variability in documentation quality, increasing the risk of errors and compliance violations. This also hinders data analysis and reporting, making it difficult to assess overall performance.
Inefficient scheduling: Disparate scheduling systems create scheduling conflicts, increase wait times, and reduce staff productivity.
Billing and revenue cycle management issues: Decentralized billing processes increase administrative overhead, delay reimbursements, and make it difficult to track revenue.
Difficulty in tracking performance: Lack of centralized data makes it challenging to monitor key performance indicators (KPIs) across all locations, hindering quality improvement efforts.
How Centralization Fixes the Problem
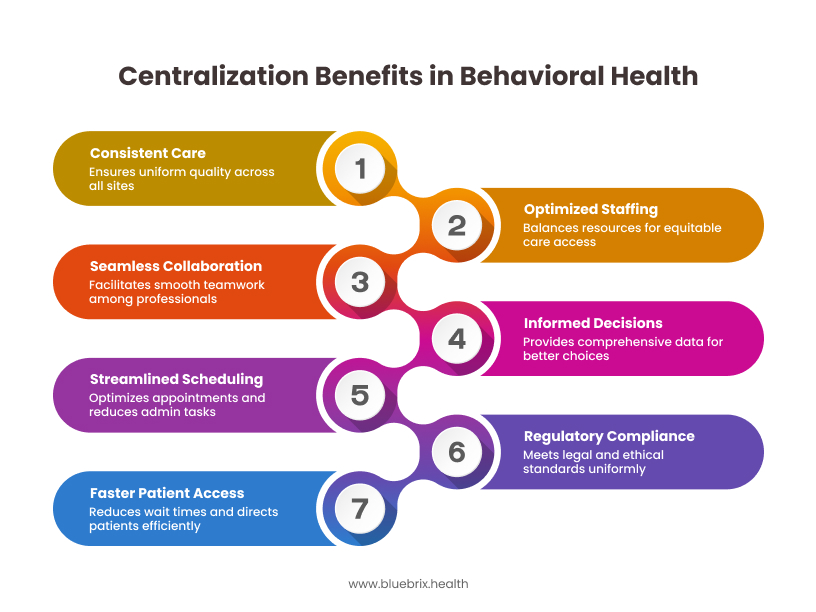
Ensuring consistent and high-quality care through standardized workflows: Aligns behavioral health documentation, assessment protocols, and treatment plans across all sites, ensuring consistent care delivery.
Facilitating seamless collaboration across the continuum of care: Enables seamless collaboration between therapists, psychiatrists, and case managers across inpatient, outpatient, and community programs.
Streamlined scheduling and admin: Central oversight optimizes scheduling for therapy sessions, intake assessments, and medication management, reducing duplication and admin overload.
Faster, smarter patient access: Centralized intake and referral systems reduce wait times and direct patients to the most appropriate level of behavioral health care (e.g., IOP, group therapy, crisis care).
Centralized systems for simplified and robust regulatory compliance: Supports uniform documentation, licensure tracking, and quality reporting to meet HIPAA, Medicaid, and multi-state compliance requirements.
Empowering informed decisions with a unified technology infrastructure: Enables enterprise-wide use of EHRs, patient portals, and analytics tools—giving clinicians access to a full behavioral health history for informed decisions.
Optimizing staffing and resource allocation for equitable care access: Balances staffing needs across locations by centrally managing clinician schedules, support roles, and specialized care teams.
Main Challenges in Centralizing Behavioral Healthcare Clinics
Different rules and needs across locations – State laws, local funding, and patient needs vary, making it hard to standardize.
Fragmented service networks – Public and private behavioral health services often operate separately, complicating system integration.
Outdated or inconsistent workflows – Manual processes and lack of clear protocols can slow down the transition to centralized systems.
Lack of flexibility – Central systems may not easily adapt to the local population’s needs or specialized services.
Tech and data issues – Integrating multiple systems, ensuring data quality, and dealing with incompatible formats is challenging.
Limited resources – Many clinics don’t have enough funding, IT support, or staff to manage system changes.
Essential Behavioral Health EHR Features for Multi-location Clinics
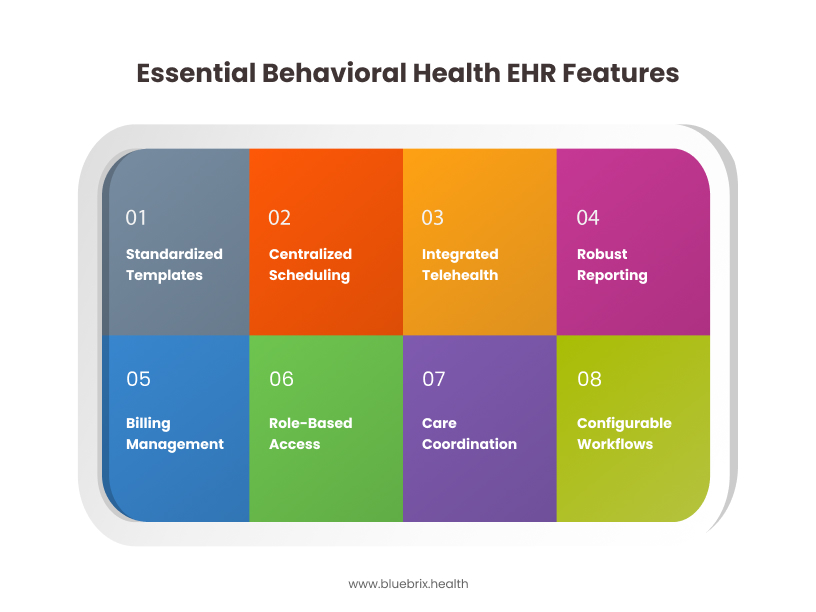
To effectively manage care across multiple sites, behavioral health clinics require an EHR system purpose-built for centralization, coordination, and compliance. Below are the key features that drive operational efficiency and care quality in a multi-location setup:
Standardized template library: Enforces consistent documentation across all sites, reducing errors and improving compliance. This allows for the creation and deployment of customizable templates, ensuring data integrity and streamlining workflows.
Centralized scheduling: Optimizes appointment management across all locations, minimizing scheduling conflicts and maximizing resource utilization. A purpose built behavioral health EHR provides a real-time view of clinician availability and patient scheduling across your entire network.
Integrated telehealth capabilities: Enables seamless virtual care delivery, expanding access to services and improving patient convenience. This offers secure and integrated telehealth functionality, allowing for virtual appointments (group or one-on-one), remote monitoring, and enhanced patient engagement.
Robust reporting and analytics: Provides real-time insights into key performance indicators (KPIs) across all sites, facilitating data-driven decision-making and quality improvement. It offers customizable dashboards and reports to track patient outcomes, operational efficiency, and financial performance.
Comprehensive billing and revenue cycle management: Streamlines billing processes, automates claims submission, and improves revenue cycle management. EHRs with integrated billing module simplifies billing workflows and optimizes reimbursement rates.
Role-based access controls: Ensures data security and compliance by granting appropriate access to patient information based on user roles and responsibilities. This provides granular access controls, protecting patient privacy and crucial for HIPAA, 42 CFR Part 2, and other behavioral health regulations.
Care coordination tools: Facilitates seamless communication and collaboration among care teams across different locations. Behavioral health EHRs secure messaging and task management features such as sharing progress notes, treatment plans, and referral management across locations enhance care coordination, referral management and improve patient outcomes.
Configurable clinical workflows for behavioral health: Customizable templates and workflows for individual and group therapy, psychiatric evaluations, substance use treatment, and other specialized programs.
Roadmap for Implementing Centralized Scheduling and Documentation for Behavioral Health
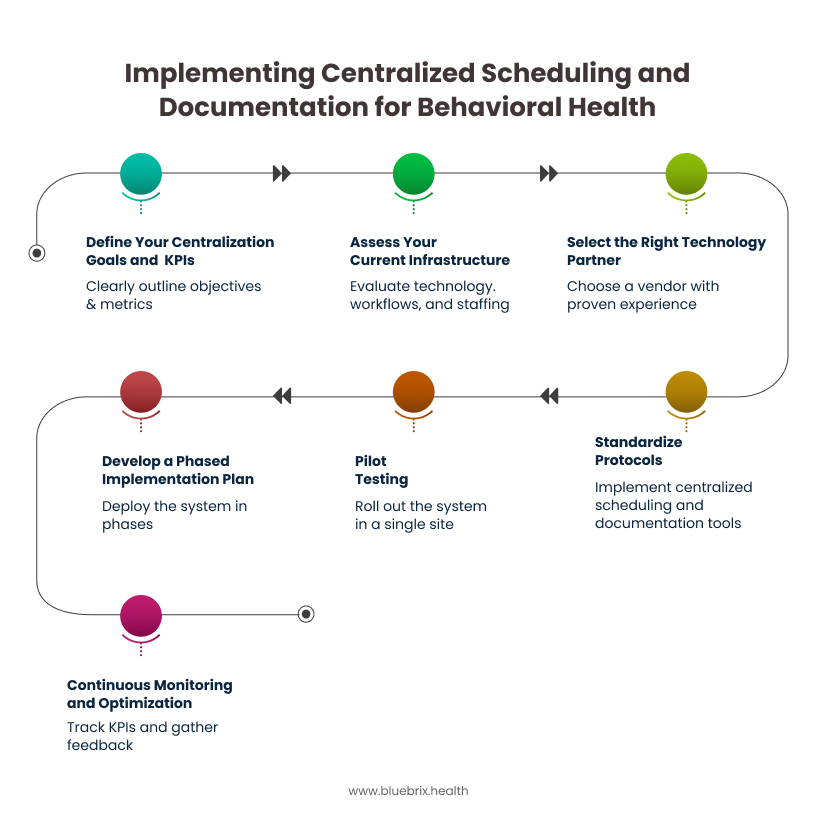
Step 1: Define Your Centralization Goals and KPIs
Clearly outline what you aim to achieve with centralization (e.g., reduce patient wait times by 20%, improve documentation compliance to 95%). Align these goals with specific, measurable, achievable, relevant, and time-bound (SMART) KPIs that will be tracked throughout the implementation and post-implementation phases.
Step 2: Assess Your Current Infrastructure
Evaluate your existing technology, workflows, and staffing models to identify gaps and areas for improvement. Audit current scheduling and documentation processes at each location to expose inconsistencies, redundancies, and system limitations. Form a cross-functional implementation team—including clinicians, administrators, IT leads, and compliance officers—to align objectives and understand location-specific nuances. Determine how a new EHR like can integrate with or replace your current systems.
Step 3: Select the Right Technology Partner
Choose a behavioral health EHR vendor that meets your specific needs and offers comprehensive support. Consider the following vendor capabilities:
- Proven experience in implementing EHRs for multi-location behavioral health practices.
- Robust functionality, including centralized scheduling, standardized documentation, and integrated billing.
- Comprehensive implementation support, including project management, data migration, and training.
- Ongoing technical support and maintenance.
- Scalability to accommodate future growth.
- Strong security and compliance features.
Step 4: Standardize Protocols
Implement centralized scheduling tools with multi-site visibility, calendar syncing, and double-booking safeguards. Create standardized, regulatory-compliant templates for treatment plans, clinical assessments, group therapy notes, and other documentation types commonly used in behavioral health settings.
Step 5: Pilot Testing
Roll out the system in a single site or region to assess real-world performance—particularly with EHR integration, telehealth compatibility, and user adaptability. Address workflow mismatches and resolve interoperability issues between sites and systems.
Step 6: Develop a Phased Implementation Plan
Deploy the new system in phases. This approach minimizes disruption and allows for adjustments based on feedback. The implementation team can provide a detailed project plan and support throughout this process.
Step 7: Continuous Monitoring & Optimization
Use real-time dashboards and reporting tools to track the KPIs defined in Step 1. Monitor patient flow, revenue cycle, clinical outcomes, and staff productivity. Conduct regular audits and gather feedback from staff to identify areas for improvement and optimize workflows. A purpose built EHR provides customizable dashboards to track these metrics and generate reports for ongoing performance analysis.
Ready to Scale? Start with Centralization
For behavioral health organizations aiming to scale with purpose, centralized scheduling and documentation is important. By unifying workflows, standardizing care delivery, and enabling real-time data visibility across locations, centralization eliminates silos, boosts operational efficiency, and ensures clients receive consistent, high-quality care, no matter where they enter your network.
It positions your organization for sustainable growth in a value-driven healthcare environment. At blueBriX, we understand the unique complexities of multi-location behavioral health clinics. Our platform is purpose-built to help you centralize operations, stay compliant, and scale confidently without sacrificing quality or control. The fastest-growing behavioral health networks are already centralizing.