Health equity is not about giving everyone the same thing—it’s about giving everyone what they need to be healthy. Some people have more barriers to good health—like not having enough money for doctor visits, access to fresh food, reliable transportation, or safe living conditions. Health equity means removing these barriers so that everyone can get the care they need.

Health equity means ensuring everyone has a fair and just opportunity to be as healthy as possible. For providers, this means offering care that is tailored to the unique needs of each patient, regardless of their background, income, or location. For patients, it means having access to the resources and support they need to achieve their best health, without facing barriers like discrimination or lack of access to services. Essentially, it’s about leveling the playing field so that everyone can achieve good health.
Health equity has become a central focus in the evolving landscape of value-based care, as recent regulatory changes emphasize the need to address disparities that have long affected underserved communities. By integrating health equity into value-based care models, policymakers aim to create more inclusive healthcare systems that reward providers for closing gaps in access, quality, and outcomes. These changes not only reflect a growing recognition of the systemic barriers many populations face but also introduce new incentives for healthcare organizations to actively promote equity as a measurable component of care delivery. In this blog, we’ll explore the importance of health equity, key concepts driving this shift, and the profound impact that health disparities have on underserved communities.
Recent Regulatory Changes Promoting Health Equity
Recent legislative developments introduce competitive bidding and a streamlined application review process to boost efficiency and expand access to care. In 2025, updates to the Medicare Advantage (MA) Value-Based Insurance Design (VBID) Model continue to prioritize care quality, health equity, and cost-effectiveness, with expanded efforts to address social determinants of health (SDOH) and health-related social needs (HRSNs). These changes aim to reduce disparities in healthcare access and outcomes for underserved populations.
Key updates include:
- Competitive Bidding: Designed to enhance affordability and fairness, competitive bidding encourages cost-effective plan designs, ensuring that high-quality care remains accessible to all beneficiaries, particularly those in low-income and marginalized communities.
- Enhanced Application Review Process: By strengthening oversight, CMS ensures that Medicare Advantage Organizations (MAOs) effectively implement equitable benefit structures that address the needs of diverse populations.
- Flexibility in Hospice Coverage: Greater flexibility allows for culturally competent, end-of-life care options, ensuring that individuals from different backgrounds receive hospice benefits that align with their values and needs.
- Focus on Health-Related Social Needs (HRSNs): Medicare Advantage Organizations are now required to offer benefits that address food insecurity, housing instability, and transportation barriers, directly targeting key health equity challenges that disproportionately affect underserved groups.
- Stronger Reporting Requirements: Enhanced data collection and reporting enable CMS to assess whether Value Based Insurance Design effectively reduces health disparities, ensuring that resources reach the communities that need them most.
Despite these advancements, CMS has announced that the Value Based Insurance Design Model will end after 2025 due to unmitigable costs to the Medicare Trust Funds. However, many of its health equity-driven interventions will continue to be integrated into broader value-based care frameworks, ensuring long-term sustainable and inclusive healthcare innovation.
Incentives for Addressing Disparities
Recent legislative changes have introduced stronger incentives for healthcare organizations to address health disparities, particularly within Medicare Advantage (MA) and value-based care models. These changes focus on equity-driven reimbursements, reporting mandates, and expanded benefit flexibility to ensure vulnerable populations receive adequate care.
Key legislative changes:
- Risk Adjustment Enhancements – Adjustments in Medicare risk scoring models now account for social determinants of health (SDOH), incentivizing providers to focus on underserved populations.
- Health Equity Index (HEI) in Medicare Advantage Star Ratings – Health Equity Index in Medicare Advantage and Part D integrates equity metrics into performance evaluations, encouraging plans to reduce disparities.
- Expanded Supplemental Benefits – Medicare Advantage plans now have greater flexibility in offering targeted benefits such as transportation, food security programs, and housing support, which directly address health disparities.
- Mandatory Health Equity Reporting – CMS now requires Medicare Advantage Organizations (MAOs) to collect and report demographic and social risk data, ensuring accountability in reducing disparities. Financial incentives linked to Health-Related Social Needs (HRSNs) further motivate providers to address SDOH.
- Value-Based Care Payment Adjustments – New payment structures reward providers who reduce gaps in preventive care, chronic disease management, and maternal health outcomes among at-risk groups.
These policy shifts ensure that health equity is no longer an optional goal but a financially incentivized priority across the healthcare system.
Challenges in Implementing Health Equity Initiatives

Implementing health equity initiatives is a complex and multifaceted endeavor. Here are some of the key challenges:
Data Collection and Sharing Issues: Accurate and comprehensive data is crucial for identifying health disparities and measuring progress. However, collecting and sharing this data can be challenging due to privacy concerns, inconsistent data standards, and lack of interoperability between systems.
Alignment of Goals Across Sectors: Health equity requires collaboration across various sectors, including healthcare, education, housing, and transportation. Aligning goals and strategies across these sectors can be difficult due to differing priorities, resources, and timelines.
Funding Limitations: Health equity initiatives often require sustained financial investment, but securing long-term, flexible funding can be challenging. Budget constraints, competing priorities, and limited grant opportunities can hinder the development and scalability of programs aimed at reducing disparities.
Complexity of Health Issues: Health equity initiatives address complex, systemic issues that require multifaceted solutions. These issues often involve social determinants of health, such as poverty, education, and housing, which are interconnected and challenging to address comprehensively. Addressing these multifaceted issues requires comprehensive strategies that go beyond traditional healthcare interventions, making implementation more difficult.
Resistance to Change: Implementing health equity initiatives often requires significant changes in organizational culture, policies, and practices. This resistance may stem from a lack of awareness, fear of increased workload, or discomfort with confronting systemic biases. Resistance to change from stakeholders, including healthcare providers, policymakers, and community members, can hinder progress.
Community Engagement Challenges: Effective health equity initiatives must be community-driven and involve ongoing engagement with community members. Building trust and ensuring meaningful participation can be challenging, especially in communities that have historically been marginalized or underserved.
Long-Term Commitment Required: Achieving health equity is a long-term goal that requires sustained effort and commitment. Short-term projects and initiatives may not be sufficient to address deep-rooted inequities, and maintaining momentum over time can be difficult.
Ensuring Compliance with New Regulations: New regulations aimed at promoting health equity can create additional administrative burdens for organizations. Ensuring compliance while maintaining focus on the broader goals of health equity can be challenging and requires resources, training, and continuous monitoring, which can strain already stretched systems.
Addressing Structural Racism: Health inequities are often rooted in structural racism, which requires systemic changes to policies, practices, and cultural norms. Addressing these deep-seated issues is complex and requires coordinated efforts across multiple levels of society.
Measuring Impact: Evaluating the impact of health equity initiatives can be challenging due to the long-term nature of the work and the difficulty in attributing outcomes to specific interventions. Developing appropriate metrics and measurement frameworks is essential for demonstrating progress and securing ongoing support.
By understanding and addressing these challenges, stakeholders can develop more effective strategies to advance health equity and ensure that everyone has the opportunity to achieve their best possible health.
The Role of Technology in Ensuring Health Equity
- Electronic Health Records (EHRs): Electronic Health Records improve the coordination of care by providing healthcare providers with comprehensive and up-to-date patient information. This helps in identifying and addressing health disparities by ensuring that all patients receive consistent and high-quality care.
- Telehealth Services: Telehealth breaks down geographical barriers, offering remote consultations to underserved and rural communities, ensuring timely medical support without the need for travel.
- Mobile Health Applications: Mobile apps provide health education, medication reminders, and self-care resources, empowering individuals to take control of their health, especially in low-resource settings.
- Data Analytics and Artificial Intelligence: By identifying health disparities through data-driven insights, AI and analytics help healthcare providers develop targeted interventions, optimize resource allocation, and improve outcomes for vulnerable populations.
- Digital Health Technologies (DTHs): Digital Health Technologies, such as wearable devices and remote monitoring tools, enable continuous health monitoring and early detection of health issues. These technologies support proactive and preventive care, which is essential for achieving health equity.
- Health Information Exchange (HIE): Health Information Exchange facilitates seamless sharing of patient data across healthcare systems, promoting coordinated care and reducing gaps in treatment for marginalized groups.
- Cultural Competency Training: Technology-enabled training programs help healthcare professionals develop cultural awareness, improving communication and care delivery to diverse patient populations.
- Community Outreach Programs: Digital platforms support community outreach efforts, connecting healthcare organizations with at-risk groups through virtual education, health campaigns, and mobile clinics.
- Addressing the Digital Divide: Recognizing that technology access is a determinant of health equity, initiatives aimed at providing affordable devices, and digital literacy programs are critical to ensuring no one is left behind in the digital health revolution.
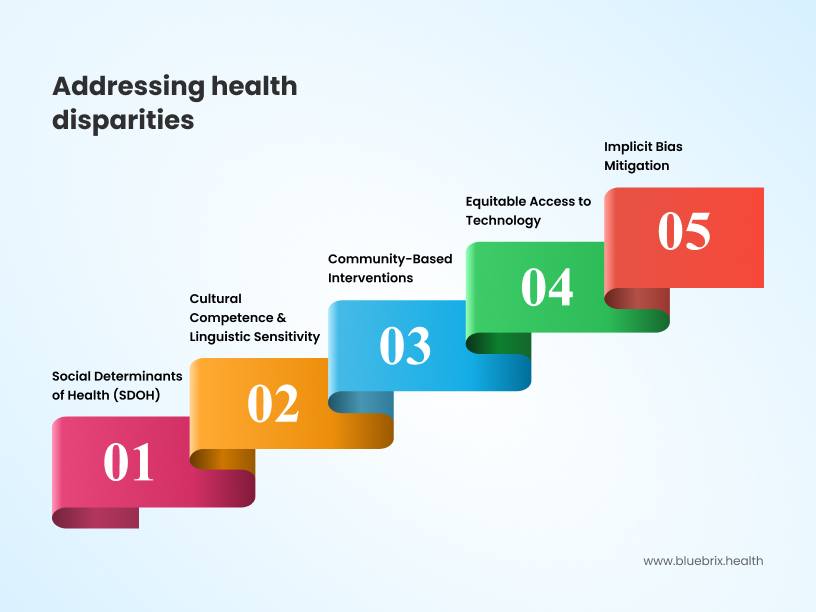
Strategies for Healthcare Organizations to Reduce Health Disparities
To effectively reduce health disparities, healthcare organizations must implement data-driven, patient-centered, and equity-focused strategies that enhance access, quality, and systemic change. The following comprehensive strategy integrates collaboration, patient engagement, continuous improvement, and policy advocacy to promote long-term health equity:

1. Strengthen Data Collection, Sharing & Analytics
- Implement comprehensive demographic and social risk data collection to identify and address disparities.
- Enhance data-sharing practices among providers, payers, and community organizations to improve care coordination and informed decision-making.
- Utilize AI and predictive analytics to track disparities, personalize interventions, and align with CMS’s Health Equity Index (HEI).
2. Expand Access to Culturally Competent Care
- Train providers in cultural competence, implicit bias mitigation, and equitable care delivery.
- Increase workforce diversity to reflect and understand patient populations more effectively.
- Offer multilingual health materials, interpretation services, and culturally sensitive care models to ensure accessibility.
3. Address Social Determinants of Health (SDOH)
- Incorporate routine screenings for food insecurity, housing instability, transportation barriers, and financial hardship.
- Partner with community-based organizations and public health agencies to provide essential social services and wraparound support.
- Expand non-medical benefits under Medicare Advantage (MA) to cover nutrition, transportation, and home modifications that impact health outcomes.
4. Incorporate Patient Feedback for Personalized, Responsive Care
- Establish patient advisory councils to gain direct insights from diverse communities.
- Use real-time patient feedback mechanisms (e.g., surveys, digital check-ins) to adjust care delivery and outreach strategies.
- Implement personalized engagement programs to improve preventive and chronic disease management, particularly for high-risk populations.
5. Monitor Outcomes & Enable Real-Time Adjustments
- Implement continuous outcome monitoring to detect emerging disparities and care gaps.
- Use real-time data and predictive modeling to adjust care protocols before disparities worsen.
- Align monitoring efforts with value-based care models to drive equity-focused performance incentives.
6. Enhance Incentives & Align Payment Models with Health Equity Goals
- Participate in value-based payment models that reward equity-driven outcomes and reduce disparities in chronic disease management, maternal health, and preventive care.
- Utilize CMS’s Health Equity Index (HEI) to improve Medicare Advantage Star Ratings and reimbursement models.
- Offer provider performance-based incentives for addressing health inequities through targeted interventions.
7. Foster Collaboration & Strengthen Community Partnerships
- Build strong collaborations with local health departments, faith-based organizations, and advocacy groups to extend care access and trust in underserved communities.
- Establish community health programs and mobile health clinics to serve rural and disadvantaged areas.
- Partner with public and private stakeholders to scale initiatives addressing social determinants of health.
8. Advocate for Policy Changes & Systemic Reforms
- Engage in policy advocacy to support long-term equity-driven reimbursement models and regulatory changes.
- Support legislative efforts that promote payment adjustments for high-risk populations and greater flexibility in Medicare Advantage supplemental benefits.
- Work with lawmakers, public health officials, and industry leaders to drive systemic reforms that reduce structural barriers to health equity.
The Future of Health Equity in Value-Based Care
As healthcare evolves, health equity is becoming a top priority for policymakers, providers, and technology innovators. Here are the key future trends shaping health equity:
AI & Data-Driven Health Equity Solutions
- Predictive Analytics for Health Disparities – AI can identify at-risk populations and predict health outcomes based on social determinants of health (SDOH).
- Bias Detection in AI & Algorithms – Healthcare organizations are working to eliminate racial and socioeconomic biases in AI-driven diagnostics and decision-making.
- Personalized Care Plans – AI-based solutions will enable customized treatment plans tailored to individual patient needs and backgrounds.
Policy & Regulatory Push for Equity
- CMS Health Equity Index (HEI) – Medicare Advantage and Medicaid plans will be required to report on health equity measures, impacting reimbursement.
- Value-Based Care (VBC) with Equity Incentives – Future payment models will reward providers for reducing disparities in healthcare access and outcomes.
- Stronger Social Services Integration – Government policies will push for greater collaboration between healthcare providers and social service organizations (food security, housing, and mental health support).
Expansion of Virtual Care & Telehealth for Underserved Communities
- Rural & Low-Income Access to Virtual Care – Telehealth platforms will expand into rural and underserved urban areas, reducing the gap in specialist access.
- AI-Powered Remote Monitoring – Wearables and home monitoring tools will help track chronic conditions, ensuring early intervention for high-risk patients.
- Culturally Tailored Digital Health Apps – Mobile health solutions will incorporate multiple languages, cultural preferences, and accessibility features to improve patient engagement.
SDOH (Social Determinants of Health) Becoming Standard in Care Models
- Routine SDOH Screening & Risk Scoring – Providers will integrate housing, food security, and transportation risk factors into medical records.
- AI-Driven SDOH Resource Matching – Platforms will match patients with social service programs based on their needs (e.g., connecting a diabetic patient with free meal services).
- Employer & Community-Based Health Initiatives – Companies will offer preventive health programs to improve workforce health and reduce disparities.
Advancements in Community-Based Healthcare Models
- Mobile Health Clinics & Pop-Up Care Centers – To reach underserved communities, healthcare will become more mobile and localized.
- Community Health Worker (CHW) Expansion – CHWs will play a larger role in navigating care, patient education, and connecting individuals to resources.
- Faith-Based & Grassroots Health Programs – Churches, local organizations, and non-traditional health hubs will partner with healthcare systems to increase trust and participation in care programs.
Inclusive Clinical Trials & Personalized Medicine
- Diverse Representation in Medical Research – Regulations and funding initiatives will push for greater participation of minority and underserved populations in clinical trials.
- Genomics & Precision Medicine for Equity – Tailored treatments based on genetic and demographic factors will reduce racial disparities in disease treatment (e.g., heart disease in Black communities).
- Decentralized Clinical Trials – Virtual and remote trial participation will increase access for underrepresented populations.
Employer-Driven Health Equity Initiatives
- Diversity & Inclusion in Workplace Health Programs – Employers will design health benefits tailored for diverse employee needs.
- Health Equity Scorecards for Employers – Companies will track their employee wellness programs’ impact on health disparities.
- Mental Health Parity Enforcement – Future regulations will push for equal access to mental health services across different demographics.
- Health equity is moving beyond just policy discussions—it’s becoming an essential business, technology, and regulatory focus. Data, AI, and personalized care models will drive the future of equitable healthcare. Collaboration between providers, tech companies, and social services will be key to eliminating health disparities.
Bridging the Gap between Intent and Impact
As value-based care continues to evolve, the integration of health equity is no longer just a regulatory requirement—it’s a moral and economic imperative. The frameworks are being put in place, the data is becoming more actionable, and incentives are aligning toward better outcomes for all. But regulations alone won’t close the gaps.
The real question is: How do we ensure that health equity doesn’t just remain a compliance checkbox, but truly transforms patient care?
For providers, this means rethinking care delivery—moving beyond traditional models to proactively address social determinants, cultural barriers, and accessibility gaps. For policymakers, it’s about designing regulations that not only encourage equity but also make it sustainable and scalable in real-world settings.
So, as we push forward, we must ask ourselves: Are we building a healthcare system where value-based care truly values everyone? Or are we just creating another set of rules that look good on paper but fail to change lives? The future of healthcare equity depends on the answer.
Ready to address health equity for your patient cohorts? Discover how blueBriX’s transformative healthcare platform can help you identify disparities, streamline care delivery, and support data-driven decisions that promote inclusivity.