Not all patients are the same—so why treat them that way? In healthcare, a one-size-fits-all approach just doesn’t work. Some patients need a routine check-up, while others are one missed appointment away from a hospital visit. How can care teams identify who needs what and when? Read on to know how the Risk Stratification piece of healthcare works!

In modern healthcare, risk stratification isn’t just a strategy—it’s a necessity. In a world shifting toward value-based care, where outcomes matter more than procedures, treating all patients the same is like navigating a storm without a compass. Some patients need a gentle nudge toward preventive care, while others require constant vigilance to avoid a health crisis. Risk stratification helps care teams focus on the right patients at the right time, ensuring that resources aren’t wasted and that those at highest risk receive proactive, life-changing interventions. Without it, value-based care loses its backbone—precision, efficiency, and most importantly, better patient outcomes.
Risk stratification is a powerful tool that enables healthcare providers to align patients with appropriate clinical initiatives based on their diagnoses and illness burden. By integrating data from clinical records and social determinants of health (SDOH), risk stratification fosters better resource allocation, enhances care management, and ultimately reshapes healthcare delivery. This blog explores the process of risk stratification, including its benefits, applications, and more.
The Critical Need for Risk Stratification in Modern Healthcare
In an era where value-based care is the driving force behind healthcare transformation, organizations can no longer afford a reactive approach to patient management. Risk stratification is essential for identifying high-risk populations, optimizing resource allocation, and improving patient outcomes. However, manual or outdated methods of stratification are no longer sufficient—technology-driven risk stratification is now a necessity, not a luxury.
Why Prioritize Risk Stratification?
- Proactive, Not Reactive Care – Technology enables real-time risk assessment, allowing providers to intervene early rather than responding to crises.
- Optimized Resource Utilization – With finite healthcare resources, prioritizing high-risk patients ensures efficient deployment of care teams, reducing unnecessary hospitalizations.
- Personalized Treatment Plans – AI-driven analytics enhance precision, ensuring that care plans are tailored to a patient’s specific risk profile, improving adherence and outcomes.
- Reduced Costs & Improved Financial Performance – By lowering hospital readmissions and emergency visits, risk stratification directly supports cost containment and financial sustainability in a value-based care model.
- Regulatory & Quality Compliance – Payers and regulatory bodies increasingly expect data-driven risk management to improve quality metrics and reimbursement rates.
Why Technology is the Key
Traditional risk stratification methods—often reliant on spreadsheets or static scoring models—fail to capture real-time patient data and evolving health risks. Advanced analytics, AI, and machine learning enable dynamic risk stratification, leveraging EHR data, claims history, social determinants of health, and wearable device inputs to create a comprehensive, continuously updated risk profile.
For healthcare organizations looking to improve outcomes, reduce costs, and excel in value-based care, technology-driven risk stratification is no longer optional—it’s a strategic imperative.
Segmentation of Patient Populations
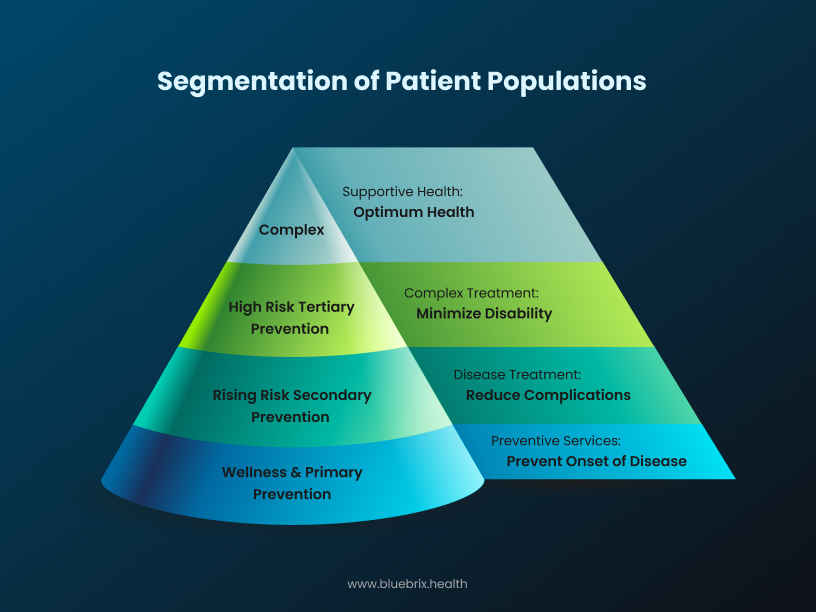
Risk stratification divides patients into distinct risk groups based on their health status:
- Low-Risk Patients: Generally healthy individuals who require minimal intervention, with a focus on maintaining health through preventive care.
- Rising-Risk Patients: Individuals showing early signs of chronic conditions or healthcare needs, who benefit from early intervention to prevent escalation.
- High-Risk Patients: Patients managing multiple chronic conditions or frequent hospitalizations, requiring coordinated, ongoing care to prevent complications.
- Catastrophic-Risk Patients: Those with life-threatening or terminal conditions requiring intensive, specialized care management.
This segmentation enables healthcare providers to deliver tailored care, ensuring that resources are allocated effectively, and interventions are appropriately matched to each patient’s needs.
Benefits of Risk Stratification

Risk stratification offers numerous benefits that enhance patient care and system efficiency:
- Targeted Intervention: By identifying high-risk patients, healthcare providers can implement targeted interventions tailored to the specific needs of these individuals. This ensures that those who require immediate attention receive it promptly, while lower-risk patients can focus on preventive measures.
- Streamlining Resource Allocation: By understanding the distribution of risk within a patient population, providers can direct their efforts and resources to areas where they will have the most significant impact, optimizing care delivery.
- Reducing Health Disparities: Through targeted interventions, risk stratification helps address health disparities by focusing more on underprivileged and vulnerable populations, ultimately improving community health outcomes.
- Cost-efficiency: By reducing unnecessary interventions and focusing on preventive care, risk stratification contributes to significant cost savings and optimized spending across healthcare systems.
- Enhanced Patient Engagement: When patients understand their health risks through risk stratification, they are empowered to take proactive steps in managing their conditions. This fosters a collaborative relationship between patients and healthcare providers, encouraging active participation in their own care.
- Reduction in Hospital Readmissions: Early identification of high-risk patients enables healthcare providers to implement preventive measures that can reduce the likelihood of hospital readmissions. By addressing potential issues before they escalate, organizations can improve overall patient outcomes and reduce healthcare costs.
- Value-based Care Support: Risk stratification aligns with value-based care models by enabling providers to focus on patient outcomes rather than volume of services. This strategic approach helps healthcare organizations meet performance metrics and improve reimbursement rates tied to quality of care.
Risk Stratification Process for Value-based Care
Risk stratification isn’t just a checkbox—it’s how providers make sure patients get the right care at the right time. Let’s break it down step by step.
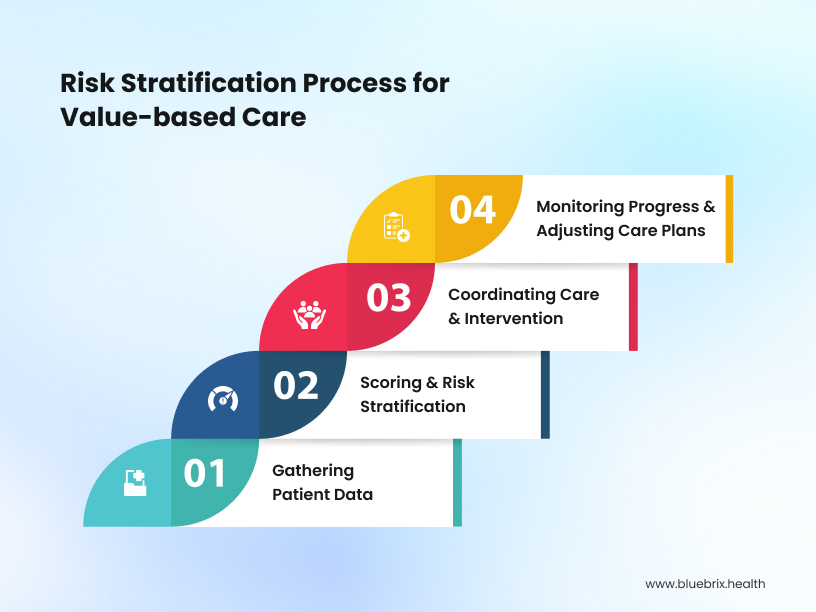
Step 1: Gathering Patient Data
Before providers can assess risk, they need good data. This means pulling in everything from EHRs, insurance claims, lab results, and even social factors like access to transportation and food. Remote monitoring devices (like smartwatches and glucose monitors) can provide real-time insights, too.
The Challenge? Data is scattered across different systems that don’t always talk to each other.
How to Fix It: Use FHIR & HL7 standards to integrate records and connect to Health Information Exchanges (HIEs).
Tech to the Rescue: AI-powered data integration pulls patient records together, making it easier for doctors to see the big picture.
Step 2: Scoring & Risk Stratification
Once all the data is in one place, it’s time to determine which patients need proactive care. Providers rely on scoring models like HCC, Charlson Index, and LACE to assign risk levels.
The Challenge? Traditional risk models are static and don’t account for real-time changes in a patient’s health.
How to Fix It: AI-driven analytics can adjust risk scores dynamically as new patient data comes in.
Tech to the Rescue: Predictive dashboards help care teams see who’s at high risk before they land in the ER.
Step 3: Coordinating Care & Intervention
Knowing who’s high-risk is only half the battle. Providers must also take action by coordinating care across different teams—primary care, specialists, social workers, and case managers.
The Challenge? Poor communication between teams can lead to delayed interventions.
How to Fix It: Care coordination platforms like blueBriX keep everyone on the same page.
Tech to the Rescue: Telehealth and remote monitoring help providers intervene faster, improving patient engagement and reducing hospitalizations.
Step 4: Monitoring Progress & Adjusting Care Plans
Risk isn’t static—it changes as patients recover or their conditions worsen. Continuous tracking is essential.
The Challenge? Manually tracking outcomes is time-consuming and prone to errors.
How to Fix It: AI-driven remote monitoring tools (like Dexcom for glucose tracking or Omron for blood pressure) can send alerts when a patient’s condition worsens.
Tech to the Rescue: IoT-enabled devices feed real-time vitals into EHRs, allowing risk models to adjust dynamically.
Why Technology is a Game-Changer
Risk stratification has always been an essential part of healthcare, but technology has completely transformed how providers can identify and manage high-risk patients. Here’s how:
Better Data Integration Means No More Guesswork
Without technology, patient data sits in silos—EHRs, insurance claims, lab results, and even social determinants of health. The result? Providers spend hours chasing down information instead of focusing on care. Modern data analytics platforms and vendor-neutral solutions now integrate patient records across systems, ensuring a complete, real-time view of health histories. This means fewer gaps in care and faster, more informed decision-making.
AI-Driven Analytics Adapt Risk Scores in Real Time
Static risk models are a thing of the past. Predictive analytics and machine learning algorithms continuously analyze patient data, updating risk scores based on new information. For example, AI can detect subtle trends—like a patient’s increasing blood pressure over several months—and flag them for early intervention before they land in the hospital. Hospitals using AI-powered predictive models have reduced avoidable ER visits by up to 30%.
Care Coordination Tools Ensure Timely Interventions
Identifying high-risk patients is just the first step—getting them the right care is where the real challenge lies. Care coordination platforms ensure primary care physicians, specialists, social workers, and case managers are aligned, preventing gaps in treatment. With real-time dashboards, automated reminders, and patient registries, providers can intervene at the right moment, improving outcomes and reducing readmissions.
Wearables & Remote Monitoring Keep Patients Engaged
Technology is shifting care beyond clinic walls. IoT devices and wearables allow patients to monitor their health from home, sending real-time vitals like glucose levels, oxygen saturation, and blood pressure directly to their providers. Remote monitoring has been shown to reduce hospital readmissions by 25%, as providers can intervene before a small issue becomes a crisis.
The Future: More Precision, Less Reactive Care
Looking ahead, technology will continue to push risk stratification further into preventive and precision medicine. Advanced AI algorithms, computational models, and real-time data streaming will refine risk assessments, allowing interventions to happen earlier and with greater accuracy. As data integration improves through HL7 and FHIR standards, providers will have a seamless, holistic view of each patient, ensuring value-based care achieves its full potential.
The Bottom Line
Technology isn’t just improving risk stratification—it’s revolutionizing how healthcare operates. By leveraging AI, data integration, and remote monitoring, providers can make smarter, faster decisions, ensuring patients receive personalized, proactive, and effective care. The result? Better patient outcomes, reduced costs, and a healthcare system that works smarter, not harder.
The Role of Social Determinants of Health
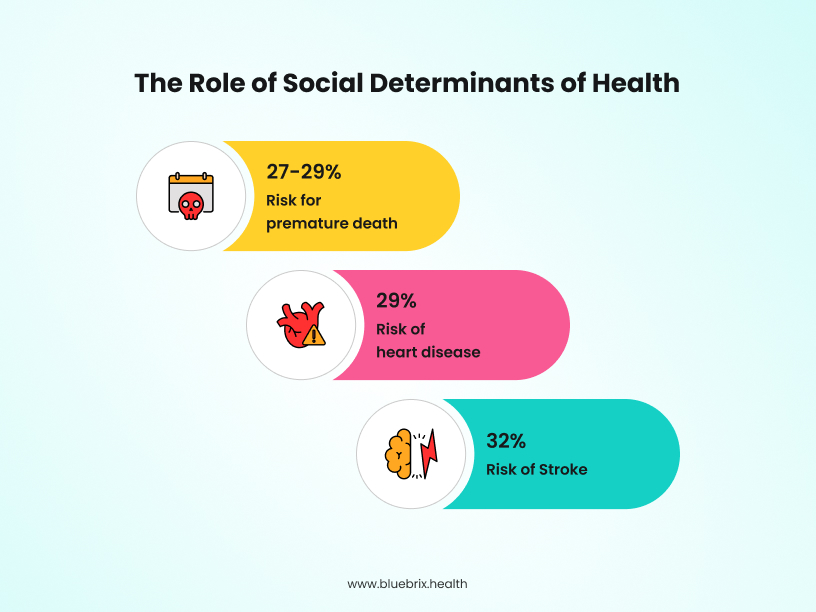
A key component of effective risk stratification is the integration of social determinants of health (SDOH), as socioeconomic factors account for approximately 47% of health outcomes, highlighting their significant role in shaping individual and population health. By addressing these factors, healthcare systems are not only promoting equity but also improving overall patient health. Advanced technologies are enabling these insights, helping healthcare providers break down barriers to care and deliver high-quality, cost-effective solutions in a rapidly evolving healthcare environment.
Shifting From Risk Stratification to Risk-Stratified Care Management
Identifying high-risk patients is just the beginning. The real impact comes from risk-stratified care management—delivering targeted interventions based on a patient’s specific risk profile. Simply knowing that a patient is at high risk isn’t enough. Providers must use that information to tailor care strategies that prevent hospitalizations and improve long-term health outcomes.
What Does Risk-Stratified Care Management Look Like?
Take two diabetic patients—one is stable with well-managed blood sugar levels, while the other has a history of uncontrolled A1C and frequent ER visits. Risk-stratified care management ensures they receive different levels of intervention. The first patient may just need routine check-ins, while the second requires continuous remote monitoring, medication management, and regular engagement with a care team.
Why This Shift Matters
Studies show that 60% of healthcare costs come from the top 10% of high-risk patients. By moving from static risk scoring to proactive care management, hospitals have seen hospitalization rates drop by 20% and healthcare costs decrease by 15%.
How Technology Makes the Shift Possible
- AI-Powered Patient Segmentation helps tailor care plans based on real-time risk factors.
- Telehealth and Remote Patient Monitoring extend care beyond clinic visits, ensuring early interventions.
- Care Coordination Platforms streamline communication among providers, ensuring high-risk patients don’t fall through the cracks.
Risk stratification is the first step, but true success comes from turning insights into action. By embracing risk-stratified care management, providers can deliver more personalized, efficient, and effective care—reducing hospitalizations, improving patient outcomes, and driving real value in healthcare.
Conclusion
Risk stratification has long been a critical tool in healthcare, but it’s only valuable when paired with meaningful action. The future of healthcare lies not just in identifying high-risk patients but in actively managing their care, personalizing interventions, and leveraging technology to prevent avoidable complications.
With advanced analytics, real-time data integration, and AI-driven insights, providers can shift from reactive healthcare to proactive, precision-driven care management. This transformation is not just an ideal—it’s a necessity for value-based care models that prioritize outcomes over volume.
At blueBriX, we understand that technology should be more than just a tool—it should be a strategic partner in improving patient outcomes. Our solutions empower providers with seamless data integration, predictive analytics, and automated workflows to make risk-stratified care management a reality.
The time to act is now. If you’re ready to take your risk stratification efforts beyond scoring and into truly impactful care management, blueBriX can help you make that leap.
Reach out today and see how we can help you transform your approach to value-based care.