Forward-thinking behavioral health clinics are considering models that reduce administrative burden, improve patient outcomes, and strengthen the therapeutic relationship. Direct psychiatry or subscription-based behavioral health model eliminates the challenges of insurance billing. This model offers a simpler, patient-focused approach.
Inspired by the success of direct primary care, this model holds strong promise for transforming psychiatric care delivery. Direct primary care (DPC) is rapidly growing in the US, with over 1,400 practices and 15,000+ DPC or concierge physicians as of 2024. The market was valued at $55.8 billion in 2022 and is projected to reach over $82 billion by 2032. Employer adoption is accelerating, with an 801% increase in employer sponsors from 2017 to 2022. Patient satisfaction is notably high—90% for DPC compared to 67% in traditional models—and both patients and employers report strong satisfaction scores. This growth is fueled by demand for personalized, accessible care and predictable costs.
For clinics and providers evaluating the future of their practice, direct psychiatry is not just an alternative—it’s a strategic opportunity to create sustainable, personalized, and value-driven mental healthcare.
What is direct psychiatry?
Direct psychiatry or subscription-based behavioral healthcare is built on a membership model, where patients pay a recurring fee—typically monthly or quarterly—directly to the practice. This fee covers a clearly defined set of services, such as extended therapy sessions, medication management, and direct communication with the psychiatrist via secure messaging or telehealth.
By cutting out the middleman—insurance companies—clinics can simplify operations, streamline finances, and focus entirely on care delivery.
Why clinics are making the shift
Here’s why more behavioral health providers are considering this model:
-
Stable, predictable revenue
The subscription model creates financial predictability, allowing practices to manage cash flow more effectively. Without the delays and denials associated with insurance claims, practices can reinvest in care quality and technology, rather than administrative overhead.
-
Reduced administrative burden
Direct psychiatry removes the need for coding, pre-authorizations, and appeals, freeing up time for both providers and support staff. This translates into lower overhead costs and fewer barriers between patients and care.
-
Improved patient access and continuity
By capping patient panels and focusing on fewer, more engaged members, psychiatrists can offer shorter wait times, longer appointments, and more consistent follow-ups. This model enhances therapeutic outcomes while fostering patient loyalty.
-
Customizable services and clinical autonomy
Clinics can tailor their membership tiers to focus on niche populations—such as adolescents, veterans, or those with chronic mood disorders—and offer treatment modalities that align with their strengths without being limited by payer contracts.
-
Stronger provider-patient relationships
When freed from the time constraints imposed by fee-for-service models, psychiatrists can invest more deeply in each patient, creating stronger alliances and more effective long-term treatment outcomes.
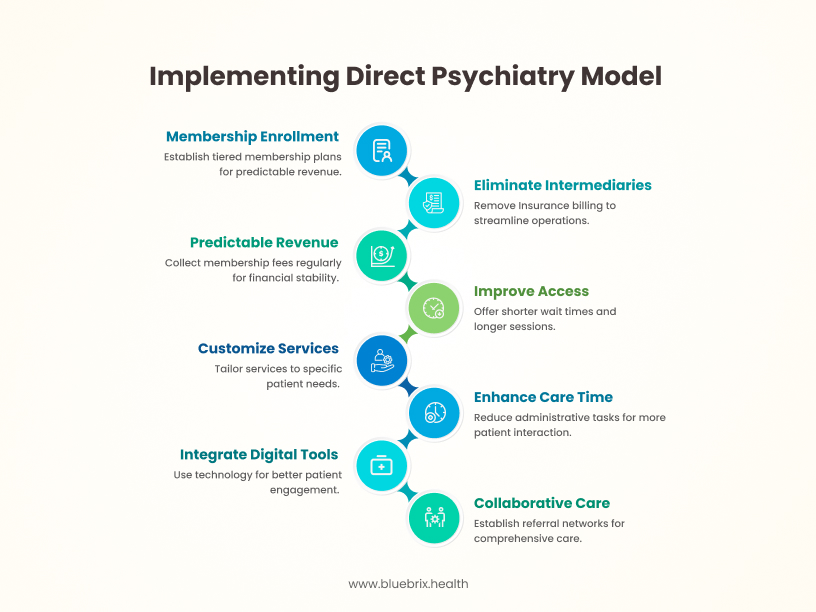
Operationalizing direct psychiatry: A Blueprint
For clinics considering implementation, the shift to direct psychiatry involves both clinical redesign and business model transformation. Here’s how to get started:
-
Membership structure
Develop tiered membership plans with clearly defined services and transparent pricing. Some practices may offer core plans focused on medication management, with add-ons for extended therapy sessions or digital support tools.
-
Technology and infrastructure
Invest in technology that supports the model:
- Secure communication tools for messaging and scheduling
- Telehealth platforms with integrated EHR support
- Digital tools for symptom tracking, medication reminders, and engagement analytics
Avoid generic EHRs designed for insurance-based care. Instead, opt for a purpose-built behavioral health EHR like blueBriX that includes membership management, cash-based billing, customizable workflows, and telehealth integration.
-
Staffing and workflow design
Reconfigure scheduling and staffing to accommodate longer appointments, reduced patient panels, and proactive outreach. Support staff should focus on member experience and care coordination, rather than insurance-related tasks.
-
Referral networks
While the membership covers core psychiatric services, clinics should build a robust network of specialists and inpatient providers. Offer guidance for navigating insurance when members require external care, and collaborate with providers who offer transparent cash pricing or accept common insurance plans.
Challenges in subscription-based behavioral health model and how to overcome them
Transitioning to subscription-based or direct behavioral health model isn’t without hurdles—but with foresight and strategy, these can be addressed effectively.
-
Out-of-pocket costs for patients
Not all patients can afford an additional monthly healthcare expense. Solutions include:
- Tiered memberships for different budgets
- Sliding scale fees or financial assistance
- Partnerships with employers to offer memberships as a benefit
- Educating patients on potential long-term savings from preventive mental healthcare
-
Insurance limitations for external services
Memberships don’t typically cover hospitalization, neuropsych testing, or IOPs. Practices should:
- Be clear about what is and isn’t included
- Provide support with insurance navigation
- Consider hybrid models for certain billable services
- Build relationships with affordable referral providers
-
Patient education and adoption
Since the model is still new, potential patients may be unsure how it works. Address this by:
- Offering educational content on your website
- Hosting informational webinars or Q&As
- Sharing testimonials from current members
- Highlighting key differences from traditional psychiatry
The role of technology: enabling scalable, personalized care
Technology is the backbone of a thriving direct psychiatry practice. A purpose-built behavioral health EHR ensures you can:
- Manage memberships, billing, and reminders effortlessly
- Communicate securely with patients between visits
- Integrate with telehealth and remote monitoring tools
- Track patient outcomes, satisfaction, and retention
- Operate securely and remain HIPAA compliant
blueBriX offers all this in a unified platform tailored for subscription-based psychiatry, helping you scale while maintaining a high standard of care.
Is subscription-based behavioral health model right for your practice?
If your clinic is:
Frustrated with administrative complexity
Seeking greater financial sustainability
Committed to personalized, proactive care
Looking to differentiate in a competitive landscape
… Subscription-based Behavioral Health model may be a perfect fit.
It allows you to build a practice centered on your values, focus on clinical excellence, and deliver mental healthcare that feels more human—for both patients and providers.