As mental health needs rise and payers double down on care quality, providers are being pushed to rethink their strategies. But beyond the industry-wide shift, the real question is: What does this mean for your organization? This blog goes beyond the surface-level overview. We’ll dive into the practical implications of VBR adoption in behavioral health—how it’s reshaping care delivery, influencing reimbursement models, and creating new opportunities for efficiency and growth.

Let’s face it—behavioral health is rapidly evolving. Rising demand, payer pressure, and evolving care expectations are forcing providers to rethink how they operate. At the heart of this transformation? Value-Based Reimbursement (VBR).
value-based reimbursement isn’t just another healthcare trend. It’s a seismic shift that’s redefining how behavioral health providers deliver care, get paid, and scale impact. This isn’t your typical high-level overview. This deep dive is for behavioral health leaders who want to move past buzzwords and get clear on what value-based reimbursement really means for their organization—today, and five years from now.
Why Value-Based Reimbursement in Behavioral Health Is Finally Taking Off
Behavioral health has historically lagged behind other sectors in adopting value-based care (VBC). But that’s changing—fast.
Today, the pressure to align outcomes with reimbursement is growing from all sides: payers, regulators, employers, and, increasingly, patients themselves. Value based care models are designed to reward real results—like fewer ED visits, lower hospitalization rates, improved treatment adherence, and stronger patient quality of life. And behavioral health, with its chronic underfunding and fragmented service delivery, is ripe for transformation.
But while the potential is massive, providers are still stuck at a critical crossroads: balancing the promise of VBC with the real-world constraints that come with it.
The Roadblocks Keeping Behavioral Health from Thriving Under VBC
You don’t need a white paper to tell you that behavioral health operates differently from other medical fields. But when VBR enters the chat, those differences become even more pronounced. Let’s break down the five big barriers keeping providers from realizing the full benefits of VBC.
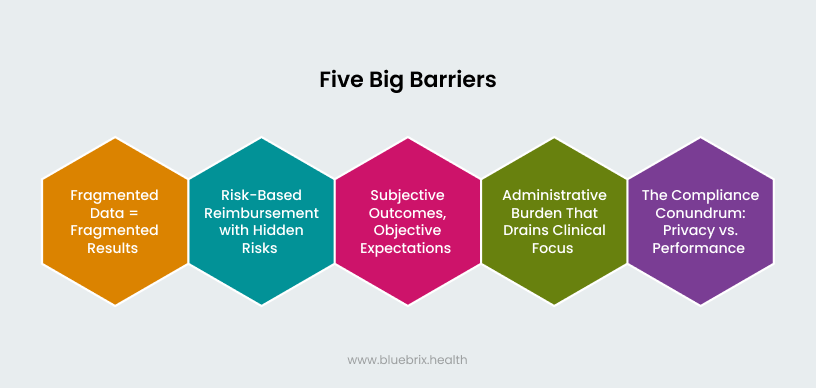
1. Fragmented Data = Fragmented Results
If you’re struggling to pull together a full picture of your patients’ progress, you’re not alone. Disconnected EHRs, patchy data sharing, and limited integration between behavioral and physical health systems are all too common.
Without reliable data, you can’t measure outcomes—and without outcomes, you can’t prove value. And that means missing out on key performance incentives and stronger payer relationships.
2. Risk-Based Reimbursement with Hidden Risks
Shared savings and bundled payments sound appealing—until you realize you’re flying blind without the right financial forecasting tools.
Most smaller and mid-sized behavioral health practices don’t have the financial runway to gamble on risk-based models without strong data to back them. The result? Caution, hesitation, and slow adoption.
3. Subjective Outcomes, Objective Expectations
Unlike a diabetes diagnosis or surgical outcome, mental health improvement isn’t always easy to quantify. And payers want standardized, repeatable measures.
That creates a mismatch: clinically meaningful progress that’s hard to translate into claimable metrics. If your organization hasn’t adopted measurement-based care tools, you’re already behind.
4. Administrative Burden That Drains Clinical Focus
Documentation, quality reporting, compliance audits—it all adds up. And in many cases, it takes away from what matters most: time with patients.
VBC shouldn’t feel like trading clinical impact for clerical overload. Yet, that’s the current reality for many providers.
5. The Compliance Conundrum: Privacy vs. Performance
Behavioral health data is sacred—and rightly so. But with VBC pushing for more transparency and interoperability, providers are walking a tightrope between HIPAA compliance and operational efficiency.
The fear of overstepping privacy boundaries can limit crucial data sharing—and that limits your ability to deliver integrated care or prove value.
The Bright Side: Why VBC Is Still Worth the Climb
For all its challenges, value-based care isn’t just a headache—it’s a high-value opportunity. For providers ready to adapt, the rewards are tangible and transformational. From delivering better patient outcomes to driving operational efficiency, the payoff makes the effort worthwhile.
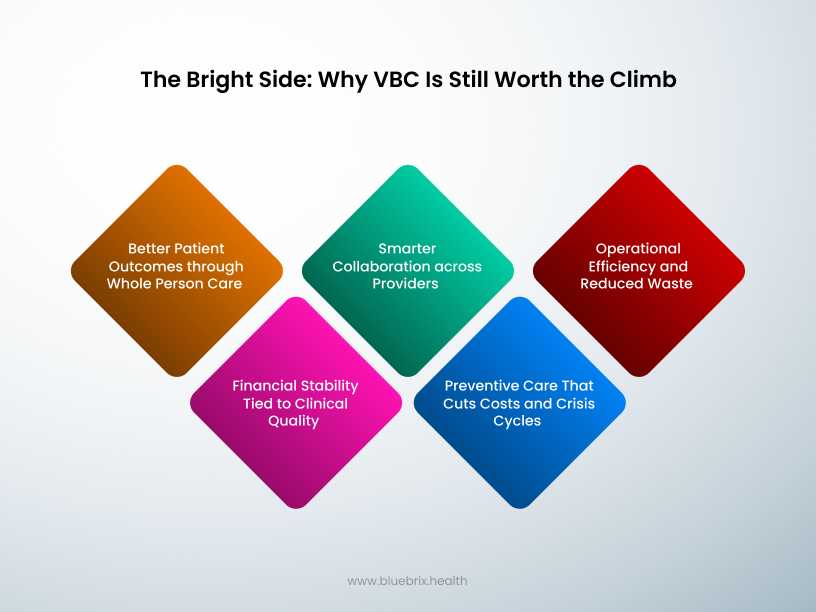
1. Better Patient Outcomes through Whole Person Care
Value based care(VBC) pushes you to break down silos and treat the whole person—not just the symptom. Integrated care models that connect behavioral and physical health are now not just possible, but encouraged (and reimbursed).
That means better outcomes, fewer relapses, and higher patient satisfaction.
2. Financial Stability Tied to Clinical Quality
With Value based care, quality and efficiency drive financial incentives. Think fewer no-shows, better care coordination, and stronger engagement—all of which lead to higher performance bonuses and more secure payer contracts.
3. Smarter Collaboration across Providers
In the old model, data stayed locked in separate systems. In Value based care, integration is the name of the game. When care teams share insights, the results speak for themselves: streamlined care, better medication management, and more complete treatment plans.
4. Preventive Care That Cuts Costs and Crisis Cycles
Proactive care = fewer emergency interventions. Value based care creates the incentive structure for early identification, ongoing support, and targeted interventions that prevent crises before they start.
5. Operational Efficiency and Reduced Waste
With the right tech stack, your team can spend less time documenting and more time delivering care. Automated workflows, real-time reporting, and better care planning free up your resources.
How blueBriX Helps Behavioral Health Providers Own the VBC Transition
Let’s be real: No provider should have to navigate this transition alone. That’s where blueBriX steps in—with purpose-built digital solutions that make value-based care work for behavioral health providers, not against them.
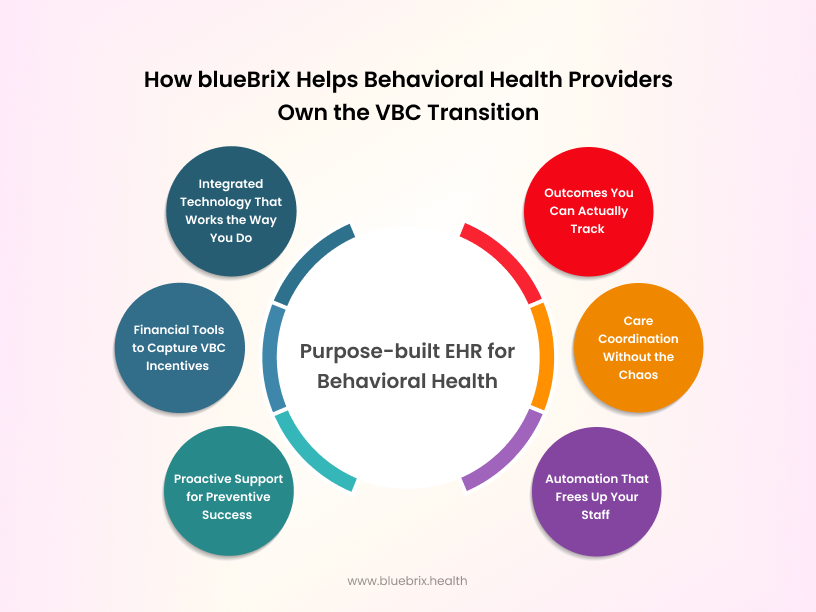
Here’s how blueBriX gives you the edge:
Integrated Technology That Works the Way You Do
Forget the clunky, one-size-fits-none platforms. blueBriX integrates seamlessly into your workflows—no overhaul required.
From care management tools to patient engagement to EHR interoperability, the platform is designed to simplify your day-to-day while powering long-term performance.
Outcomes You Can Actually Track
No more guessing. With real-time healthcare data analytics, risk stratification, and personalized care plans, blueBriX gives you the ability to measure what matters—and show payers you’re delivering results.
Financial Tools to Capture VBC Incentives
Every quality metric, every positive outcome—you’ll have the reporting to back it up. That means stronger payer negotiations, shared savings opportunities, and a more sustainable revenue stream.
Care Coordination Without the Chaos
blueBriX eliminates data silos by connecting behavioral health, primary care, and specialty providers into a single ecosystem. The result? More collaborative care and fewer patient fall-throughs.
Proactive Support for Preventive Success
With built-in tools for outreach, reminders, and automated follow-ups, you’ll stay connected to high-risk patients before things escalate—and support better long-term outcomes.
Automation That Frees Up Your Staff
The platform automates documentation, reporting, and quality tracking, cutting admin time and burnout so your team can focus where it counts: on patient care.
What Comes Next: Future-Proofing Your Strategy for VBR
The shift to value-based reimbursement is accelerating. So, what should behavioral health providers be preparing for next?
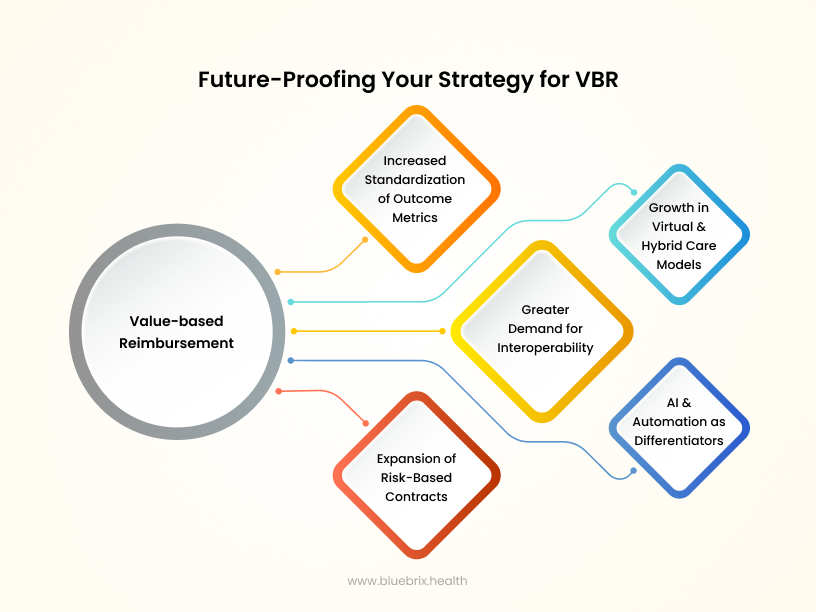
- Increased Standardization of Outcome Metrics: Expect tighter definitions around quality benchmarks. The ability to measure and prove mental health outcomes will become non-negotiable.
- Greater Demand for Interoperability: Payers will expect seamless data-sharing across care teams, systems, and settings. Providers must invest in tech that bridges the gap without compromising privacy.
- Expansion of Risk-Based Contracts: Value-based reimbursement(VBR) will evolve beyond pilots and small programs. Broader, more complex contracts will reward not just outcomes, but cost control, patient experience, and equity.
- Growth in Virtual and Hybrid Care Models: As payers recognize the value of accessibility, expect to see incentives for telebehavioral health and integrated care models.
- AI and Automation as Differentiators: Organizations that harness AI to reduce administrative burdens, identify risks, and personalize care will gain a significant competitive edge.
To stay ahead, behavioral health leaders must adopt an innovation-first mindset—proactively shaping their care models, workflows, and payer strategies to thrive in a value-driven ecosystem.
Ready to Lead the Way in Behavioral Health VBC?
The future of behavioral health is value-based—and the organizations that lean in now will be tomorrow’s leaders. blueBriX helps you turn a complex transition into a clear, competitive advantage. Less paperwork. More impact. And real, measurable value from every care interaction.
Book a demo today and see how blueBriX can help your team thrive in the VBC era.
Frequently Asked Questions
VBR is a payment model that ties provider reimbursement to patient outcomes rather than the number of services delivered. In behavioral health, this means focusing on long-term improvement, reduced emergency visits, and overall well-being.
Behavioral health providers often face hurdles like limited EHR adoption, data-sharing constraints, subjective outcome measures, and fragmented systems—all of which make tracking and reporting outcomes more complex.
Key challenges include siloed data, financial risk in bundled/shared savings models, difficulty quantifying outcomes, administrative overload, and navigating HIPAA-compliant data sharing.
VBR can lead to improved patient outcomes, more coordinated care, financial incentives for high-quality service, increased operational efficiency, and a shift toward preventive, whole-person care.
blueBriX offers integrated digital tools for care management, analytics, patient engagement, and outcome tracking—empowering providers to meet payer demands, streamline operations, and enhance patient care without increasing administrative burden.