
If you’ve ever run a group therapy session, you already know the feeling—what’s transformative for your clients can be exhausting for you.
While your group connects, supports each other, and makes progress, you’re left staring at your EHR thinking: “How do I capture all of this; accurately, compliantly, and for every participant?”
That’s the paradox of modern behavioral health care tools!
Group therapy is clinically powerful but operationally painful. The culprit? Technology that was never built for it. Most EHR systems were designed for one provider, one patient, one chart and not for six participants, shared interventions, and individualized notes.
The result: hours of redundant documentation, compliance anxiety, and a creeping sense of burnout that steals time away from real clinical work.
So let’s fix that.
In this blog, we’ll unpack what’s actually broken in today’s documentation workflows, explore how purpose-built behavioral health EHRs are reshaping the process, and explain why intelligent documentation isn’t just a tech upgrade, but is a clinical necessity.
The Real Documentation Problem Holding Back Behavioral Health Practices
Here the problem isn’t you. It’s your system.
Most clinicians aren’t struggling with documentation because they don’t know what to record. They’re struggling because their EHR wasn’t built for the reality of behavioral health.
Traditional EHRs were designed for the medical model; one provider, one patient, one record. That works fine in a hospital or primary care setting, where encounters are procedure-based and patient-specific. But in behavioral health? Especially in group therapy? That model collapses.
Think about it. In a single group session, you’re managing shared discussions, collective interventions, and individual outcomes and yet your EHR only wants you to document one patient at a time. The system’s data structure literally can’t comprehend multi-client relationships within a single encounter.
So, what happens? Clinicians are forced into a maze of manual workarounds just to make their documentation fit the system’s logic, not the other way around.
That’s how you end up with:
- Technical limitations that make it nearly impossible to link group notes and individual progress accurately.
- Privacy risks, since standard systems can’t easily separate shared session data from individualized notes raising red flags under HIPAA and 42 CFR Part 2.
- Workflow chaos, where billing and compliance are tied to one patient ID per note, even though six or eight clients attended the same session.
When your EHR is built around the wrong logic, it turns meaningful therapeutic work into fragmented data entry.
At its core, this isn’t a training issue or a workflow glitch. It’s a design flaw. Behavioral health needs systems that understand multi-client, relational care and until that happens, clinicians will continue working against their technology instead of with it.
Now that we’ve unpacked what’s fundamentally broken in traditional EHRs, let’s get more specific. What does this misalignment actually look like in day-to-day group sessions? Let’s break down the three biggest challenges every behavioral health provider faces when documenting group therapy.
The Three Hidden Challenges Behind Group Therapy Documentation Chaos
Let’s be clear, none of these challenges come from clinician error. They come from systems that weren’t designed to handle the real-world complexity of behavioral health. Here’s what that looks like when theory meets therapy.
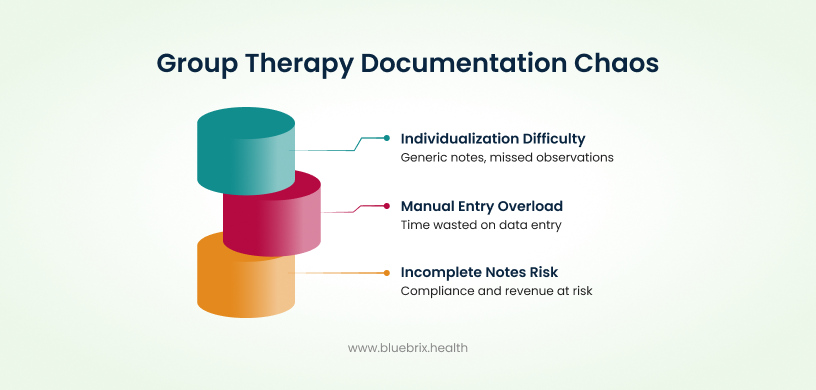
Challenge 1: Keeping Every Client’s Progress Note Individualized in a Shared Session
Imagine you’re Dr. Lopez, running a weekly trauma support group with eight participants. The session explores coping strategies, shared insights, and progress milestones. When it’s over, you open your EHR and that’s when the real work begins.
Now, you need to create individual progress notes for every participant. Each must reflect shared group activities while capturing each client’s unique journey, their reactions, emotional tone, and personal goals.
But here’s the issue: without group-specific templates or automated cloning tools, clinicians are left duplicating notes manually or risk oversimplifying.
The result?
- Notes that sound too generic.
- Missed individualized observations.
- Increased audit risk because payers demand distinct documentation for every billed service.
When EHRs can’t support individualized progress tracking, clinicians are forced to choose between speed and clinical quality; a trade-off no one should have to make.
Challenge 2: Manual Entry and Redundant Documentation That Drain Time and Morale
This one hits every behavioral health clinician hard. For each group session, you’re re-entering the same session details; date, time, interventions for every single participant. That’s six, eight, sometimes ten repetitions of the same data.
Generic EHRs don’t offer shared-session automation. So clinicians waste precious hours doing data entry instead of therapy.
Over time, this leads to what many call “EHR fatigue”; the mental exhaustion of documenting the same information again and again, day after day. The time you lose here isn’t just administrative; it’s time stolen from your patients, your team, and your well-being.
Challenge 3: Incomplete or Inconsistent Notes That Put Compliance and Revenue at Risk
When documentation is fragmented or incomplete, it’s not just inconvenient. Instead it’s dangerous from a compliance standpoint.
Every individual record must demonstrate medical necessity, session details, and client-specific outcomes. If a note is vague, inconsistent, or lacks required payer details, the claim is at risk.
This leads to:
- Denied or delayed reimbursements
- Audit vulnerabilities
- Compliance exposure under HIPAA and 42 CFR Part 2
And when you’re operating multiple sessions per week, across dozens of clients, one small inconsistency can cascade into serious revenue loss or regulatory headaches.
In short, traditional EHRs force clinicians to work against the system, resulting in lost time, burnout, and operational risk. The tools meant to simplify your work have, ironically, made it harder.
So, if standard EHRs are fundamentally flawed for group settings, what’s the alternative? The answer lies in technology that’s built for behavioral health from the ground up, not retrofitted for it. Let’s explore how a purpose-built behavioral health EHR turns documentation from an obstacle into an operational advantage.
How Purpose-Built Behavioral Health EHRs Fix Group Therapy Documentation for Good
The problem isn’t group therapy. It’s the outdated EHR architecture behind it. What you need isn’t a workaround, but it’s a workflow that understands the nature of behavioral health care.
A purpose-built behavioral health EHR does exactly that. It eliminates duplication, reduces cognitive load, and brings compliance and efficiency under one roof, so documentation finally supports, not sabotages, the therapeutic process.
Here’s how that transformation happens.
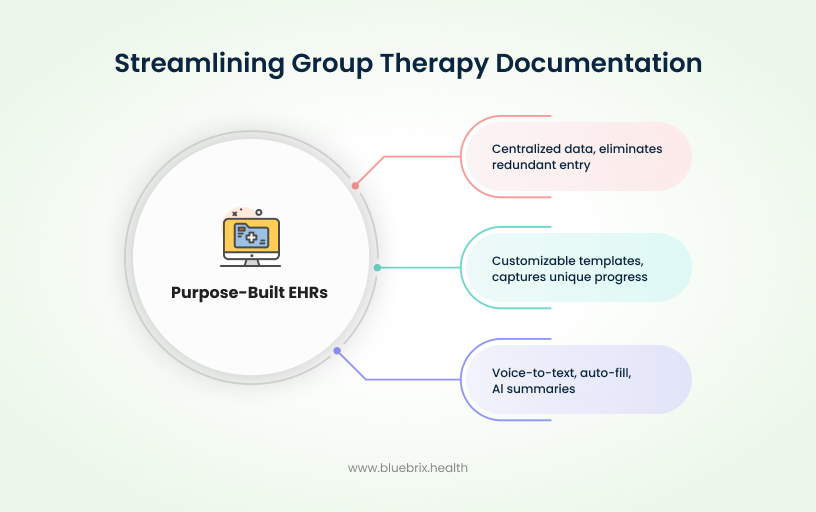
Solution 1: Unified Group Note Workflows – One Session, Seamless Documentation
Picture this: instead of documenting the same session details eight times, you create one master session note. From that single record, your EHR automatically populates the date, duration, session topic, and interventions across all participant charts.
That’s the foundation of a unified group note workflow.
- What it does: Centralizes all shared session data, the “who, what, and when” in one place.
- How it helps: Eliminates redundant data entry, minimizes manual errors, and ensures every participant’s chart stays synchronized.
- Compliance win: Each note is still linked to an individual record, preserving accountability and audit traceability.
Solution 2: Intelligent Individualization Within Shared Sessions
Now, here’s the real game-changer; intelligent individualization.
In traditional EHRs, the biggest compliance risk comes from generic notes that fail to show each client’s unique progress. Purpose-built behavioral health systems fix that through customizable note templates that prompt you to capture individual goals, responses, and outcomes, all within the same group session framework.
Think of it as “smart branching logic” for your documentation:
- The shared session note stays constant.
- The individualized sections evolve for each client.
Each record tells a complete, compliant story, the “Golden Thread” that ties treatment plans → progress notes → outcomes.
The result? No more oversimplified notes. No more payer pushback. Just accurate, individualized documentation that satisfies both clinical and billing requirements.
Solution 3: Automation and AI-Driven Efficiency Tools – Document Smarter, Not Harder
Once you’ve nailed structure and compliance, the next frontier is speed and ease. That’s where automation and AI-driven tools come in.
Modern behavioral health EHRs now integrate:
- Voice-to-text dictation so clinicians can document hands-free.
- Auto-fill dropdowns and attendance tracking that update records in real time.
- AI-generated summaries and smart note suggestions that learn from clinician input to refine documentation accuracy.
In other words, your EHR becomes a clinical assistant, not a clerical burden. These tools cut documentation time dramatically, reduce fatigue, and improve consistency across sessions.
When your system can think and move with you, documentation stops feeling like data entry and starts feeling like a natural part of your care delivery.
Now that we’ve covered how purpose-built EHRs solve the documentation dilemma, it’s time to look at the bigger picture, the why behind all of this. Why does intelligent documentation technology matter so much for behavioral health?
Why Intelligent Documentation Technology Matters in Behavioral Health
At its core, intelligent documentation technology isn’t just about saving click. Instead, it’s about protecting your clinicians, your revenue, and your mission. Let’s break down how the right technology turns documentation from a liability into a long-term asset.
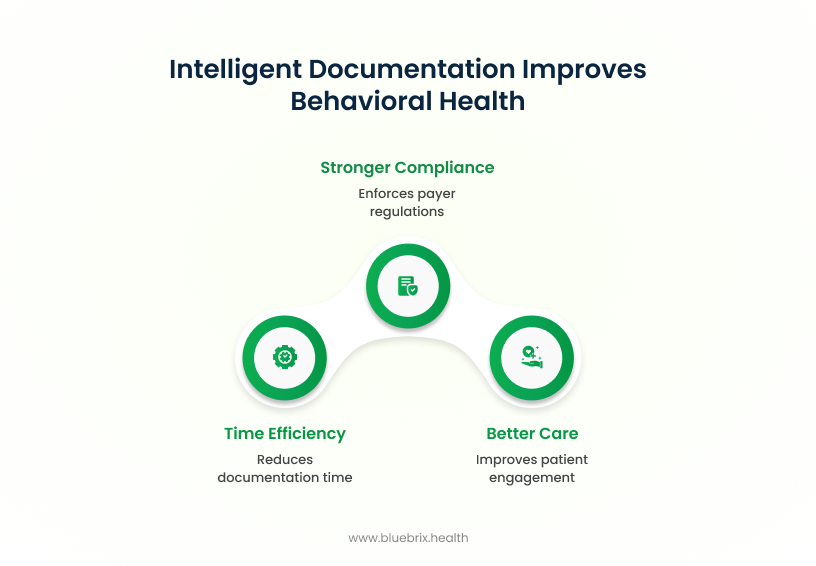
Benefit 1: Time and Cost Efficiency
Clinicians shouldn’t spend more time typing than treating.
With intelligent automation built into a behavioral health EHR, tasks like session metadata entry, attendance logging, and note cloning are handled automatically. Research shows that optimized EHR workflows can cut documentation time by over an hour per session, freeing clinicians to either see more clients or spend more time delivering actual care.
The result?
- Dramatically lower administrative overhead.
- Reduced overtime and burnout costs.
- More billable sessions without sacrificing quality.
When documentation takes half the time, practices see both operational and financial ROI within weeks.
Benefit 2: Stronger Compliance, Fewer Claim Denials
Behavioral health group therapy documentation must meet strict payer and privacy regulations, including 42 CFR Part 2 and HIPAA. Intelligent EHR workflows enforce compliance by design through standardized templates, automated prompts, and built-in data validation.
That means every group note consistently captures:
- Clinical justifications and medical necessity
- Required consent and attendance details
- Progress aligned to individualized treatment goals
With cleaner, standardized notes, practices experience:
- Fewer denials
- Faster reimbursements
- Lower audit exposure
Meaning, compliance becomes a natural outcome of your workflow. not a separate checklist to worry about.
Benefit 3: Better Care, Better Outcomes
When clinicians aren’t buried in paperwork, they reconnect with their purpose of helping and healing people.
Reduced documentation fatigue directly improves therapeutic presence and patient engagement. Meanwhile, more complete and accurate notes enhance clinical decision-making, continuity of care, and outcome tracking across group programs.
In short:
- Clinicians feel supported, not strained.
- Patients receive more attentive care.
- The entire organization operates with greater clarity and accountability.
That’s what happens when documentation stops being a burden and starts being an enabler of better care.
Now that we’ve seen why intelligent documentation matters strategically, let’s bring it home with a real-world look at how one platform like blueBriX, operationalizes these principles into a clinician-centered EHR ecosystem built for behavioral health.
It’s Time to Rethink Group Documentation — The blueBriX Advantage
At the end of the day, behavioral health providers shouldn’t have to fight their EHRs just to do their jobs. That’s exactly where we can discuss what blueBriX delivers. Built specifically for behavioral health, blueBriX turns the chaos of group documentation into a seamless, compliant, clinician-friendly experience.
Here’s how it makes that possible:
- Smart Group Documentation: With blueBriX, clinicians create a single master session note that automatically populates session metadata like date, time, and focus across all participant records.
- Compliance Built In: The system aligns with HIPAA and 42 CFR Part 2, guiding clinicians with intelligent templates, alerts, and secure data handling protocols and that results in consistent payer-ready documentation, reduced audit risk, and faster, cleaner reimbursements.
- Clinician-Centered Workflows: Every feature in blueBriX is designed to make clinicians’ lives easier. Voice-to-text dictation, automated attendance, and AI-powered note suggestions minimize administrative fatigue and keep documentation flowing naturally.
- A Fully Connected Behavioral Health Ecosystem: Documentation is just one piece of the blueBriX advantage. From integrated scheduling and billing to telehealth and multi-location coordination, blueBriX connects the entire continuum of behavioral health care.
The Takeaway
If your current system is draining clinician energy, slowing reimbursements, or triggering audit stress, it’s time to see what purpose-built behavioral health technology can really do.
blueBriX helps behavioral health teams document smarter, stay compliant, and focus on delivering care that changes lives.
Schedule a personalized demo of the blueBriX Behavioral Health EHR and discover how you can:
- Streamline group documentation
- Strengthen compliance
- Reclaim clinician time