No two people heal the same way. One person’s anxiety might calm with CBT and community support. Another might need trauma-informed therapy, regular follow-ups, and medication oversight. Yet, for years, behavioral health has treated them almost identically; same sessions, same timelines, same expectations.
That approach no longer works. Today’s patients expect care that understands their story. Clinicians want systems that evolve with real-life progress, not static templates. Behavioral health has outgrown the one-size-fits-all mindset, because no diagnosis tells the full story.
Every person brings their own mix of biology, environment, and living experience. When treatment ignores those factors, engagement drops, recovery slows, and relapse becomes a recurring cycle.
Of course, personalization sounds simple until you try to make it work in daily operations. It requires deep insight, constant monitoring, and the ability to make timely adjustments. Many practices struggle because the right infrastructure is missing.
That is where technology steps in. Modern EHRs are not just digital filing systems anymore. They have become intelligent ecosystems that bring every piece of patient data together, surface patterns, and help clinicians deliver care that is adaptive, evidence-based, and truly personal.
In this blog, we will look at why personalized treatment plans are no longer optional in behavioral health and how the right digital foundation can make them measurable, scalable, and real.
Why personalization is non-negotiable in behavioral health
Two patients might share the same diagnosis, but everything else about their lives can look completely different. One’s fighting social isolation. Another is trying to manage childhood trauma. A third juggling a job, family, and a cycle of panic attacks that never seem to end.

Give them all the same treatment plan, and what happens? They disengage. They relapse. They stop believing in therapy work.
That’s exactly why personalization has shifted from “a nice idea” to “the only way forward.”
Let’s unpack what makes it so powerful.
It turns patients into partners – Patients who help design their treatment plans don’t need reminders to engage. They already care because it’s their plan. They know why every step matters and what success looks like for them. That ownership changes the entire tone of therapy from being told what to do to being part of the process.
It sees the whole human, not the disorder – Behavioral health is never just psychological. It’s social. It’s environmental. It’s medical. Personalized planning connects those dots instead of treating symptoms in silos. When clinicians understand a patient’s relationships, culture, and physical health, care becomes relevant and respectful.
It moves at the speed of life – Mental health isn’t static. One week, a patient’s stable. The next, they’re struggling again. Personalized plans flex with those shifts. They give clinicians the freedom to update care in real time instead of waiting for a monthly check-in that’s already too late.
It builds trust that data alone can’t – Personalization is how trust grows. When patients feel understood and not just diagnosed, they open up. They’re honest. They stick with care because they finally believe someone is actually listening.
And here’s the kicker: research already proves it. Personalized behavioral health consistently outperforms standardized care in engagement, satisfaction, and long-term recovery. So, the question isn’t whether personalization works. It’s how we make it part of everyday care without overloading clinicians or systems. That’s where the next part of this story begins, what personalized care looks like when it’s done right.
The measurable impact: from engagement to long-term recovery
Evidence speaks louder than intent. Across behavioral health settings, one pattern keeps repeating. When care becomes personal, everything improves.
Here is what that looks like in real-world practice.
The following are fictional scenarios, inspired by real-world experiences in behavioral health practices. They illustrate how personalization can transform care outcomes.
Case 1: turning dropouts into progress
Dr. Kim runs a small outpatient practice that focuses on anxiety and panic disorders. For years, her team followed standard CBT modules. Some patients improved quickly, but many drifted away after a few sessions.
The turning point came when her team began analyzing engagement data such as attendance patterns, journaling activity, and feedback after each session. They noticed something interesting. Patients who skipped their journaling assignments were also the ones most likely to cancel appointments.
Dr. Kim shortened homework tasks, added quick mobile check-ins, and scheduled automated reminders. Within three months, patient adherence improved by up to 40 percent, and dropout rates fell to under 10 percent.
That is personalization in action. Small insights created through data translated into meaningful progress.
Case 2: managing complexity with precision
A regional behavioral health facility treating dual-diagnosis patients faced the classic data problem. Medication records, therapy notes, and social updates were all stored in separate systems. Coordinating care was nearly impossible.
After consolidating their data into one system, patterns started to appear. The team realized medication adherence often declined right after patients switched therapy groups. The clinicians responded by adding one-on-one follow-up sessions during those transitions.
The results will be immediate:
- The results were striking:
- Medication adherence improved by up to 30 percent
- Crisis interventions dropped by nearly half
- Patient satisfaction rose from “moderate” to “very satisfied” within a quarter
When teams can actually see their data, they can manage complexity instead of reacting to it.
Case 3: from reactive to proactive
An adolescent care program kept seeing the same frustrating trend. Teens with depression were stable most of the year, but relapse always spiked during exams. This time, the clinicians decided to stay ahead of the pattern.
They started monitoring mood and journaling data through patient self-reports. When activity levels dropped or stress markers rose, the team received alerts and adjusted treatment plans within days.
By the end of the semester, crisis visits may drop by as much as 60 percent, and overall mood scores showed consistent improvement across the program.
This is the essence of personalization. Care that moves as quickly as the patient’s life does.
Whether it is a solo practitioner or a large behavioral health network, the results tell the same story. When care becomes personal, engagement deepens, recovery stabilizes, and operations become more efficient. This is not theory anymore. It is measurable and repeatable.
The next step is to understand how to make personalization operational. Let’s look at what it actually takes to build this level of care into daily clinical workflows.
What personalized care looks like in practice
It is a mindset that reshapes how clinicians think, plan, and respond. When done right, it feels less like “a workflow” and more like a conversation that evolves with the patient.
Let’s look at how that plays out in real-world settings.
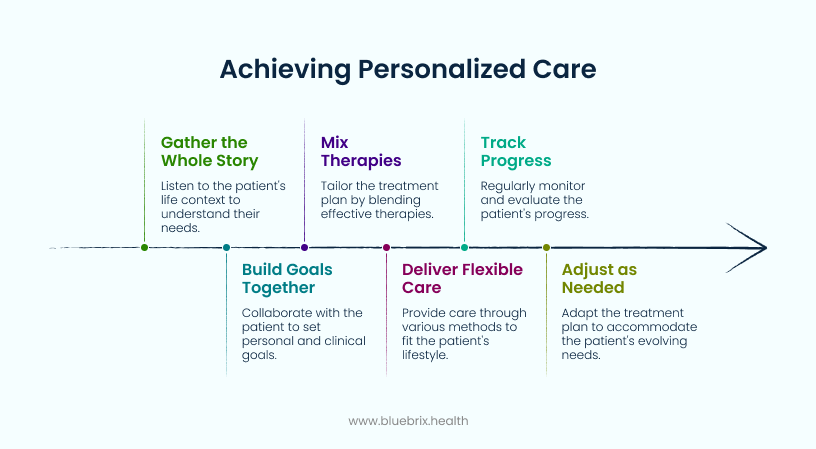
Personalized care starts with context; understanding the full story behind each patient’s journey, setting goals together, and adapting as life changes. It’s not about rigid protocols but about aligning clinical insight with real-world needs. When clinicians have the right tools to see progress, respond in real time, and adjust seamlessly, care feels less procedural and more human. That is exactly what drives lasting recovery. The real question is how to make this level of personalization possible at a scale across hundreds of clinicians and thousands of patients, without losing human touch.
That is where the right technology makes all the difference.
How blueBriX EHR makes it possible and scalable
Personalization sounds inspiring, but anyone in behavioral health knows how messy it can get behind the scenes. Different clinicians use different tools; patient data lives in disconnected systems, and real-time insights often come too late.
That is where blueBriX changes the story. Here is how we make personalized care repeatable, measurable, and scalable across teams, locations, and care models.

- Behavioral health care is multi-layered. A change in sleep patterns, a missed appointment, or a stressful event can all alter recovery. blueBriX brings every data point; clinical, behavioral, and social into one view. Clinicians can instantly see the connections, like how a patient’s mood shifts after medication adjustments or stressful life events. That clarity turns guesswork into precision and helps clinicians act before a setback happens.
- Small changes can reveal big risks. blueBriX helps clinicians track progress, symptom trends, and engagement in real time. If a patient misses a session, logs a negative mood entry, or shows a decline in activity, the system surfaces that insight immediately. Instead of reacting after a crisis, clinicians can intervene in early adjusting treatment or scheduling check-ins before the situation worsens.
- Personalized care works best when the entire care team moves as one. With blueBriX, psychiatrists, therapists, case managers, and primary care providers can collaborate through shared workflows. Progress notes, medication changes, and follow-ups are instantly visible to everyone involved. That eliminates duplication, prevents communication gaps, and ensures every clinician sees the same, complete story.
- blueBriX uses a robust clinical data repository (CDR) engine that automates how information flows across care workflows. It doesn’t replace clinical judgment, it simplifies it. The system automatically organizes data from multiple sources, surfaces what matters in real time, and keeps clinicians focused on care instead of coordination. That efficiency helps teams act faster, stay aligned, and maintain the human touch that defines quality care.
- Patients play a central role in their recovery when they can actually see their progress. Through the blueBriX patient portal, individuals can track goals, submit feedback, report symptoms, and stay connected with their care team. That visibility builds accountability and trust, turning patients into active partners instead of passive participants.
- No two behavioral health organizations operate the same way. blueBriX adapts to each one through configurable templates, automation, and integration support. Whether you are managing one clinic or multiple facilities, it scales with you supporting new care models, payment structures, and regulatory requirements without disruption.
Imagine a connected ecosystem where every patient journey fuels continuous learning. Where data informs decisions instantly. Where clinicians spend time on care, not coordination. That is what blueBriX was built to deliver. A behavioral health environment that is data-driven, adaptive, and deeply human at the same time.

