Most health systems are still trying to make palliative care work within frameworks built for hospitals. It’s a common but costly mistake.
Those frameworks were built to move patients through beds, not walk with them through the hardest chapters of their lives. They’re built for speed, not stability. For discharge, not dignity.
Palliative care is a different world entirely. It’s not episodic, it’s continuous. It’s not transactional, it’s relational. It’s where data meets emotion, and where coordination is less about logistics and more about human continuity.
Yet, we still measure success using metrics like “readmission rates” and “length of stay,” while ignoring what truly defines quality here; pain relief, peace of mind, and the emotional bandwidth of the family holding everything together.
The truth is, you can’t retrofit empathy into a hospital workflow. And you can’t expect EHR checkboxes to capture the reality of palliative care.
With an aging population, rising chronic illnesses, and expanding CMS value-based programs that reward continuity and quality of life, the need for a purpose-built palliative coordination model is now the next operational frontier, where compassion and efficiency finally converge.
The coordination crisis: why standard models fail palliative care
Let’s be real; the hospital model was built for throughput: stabilize, discharge, repeat. That logic works beautifully for acute cases but collapses when applied to long-term, emotionally complex palliative journeys.
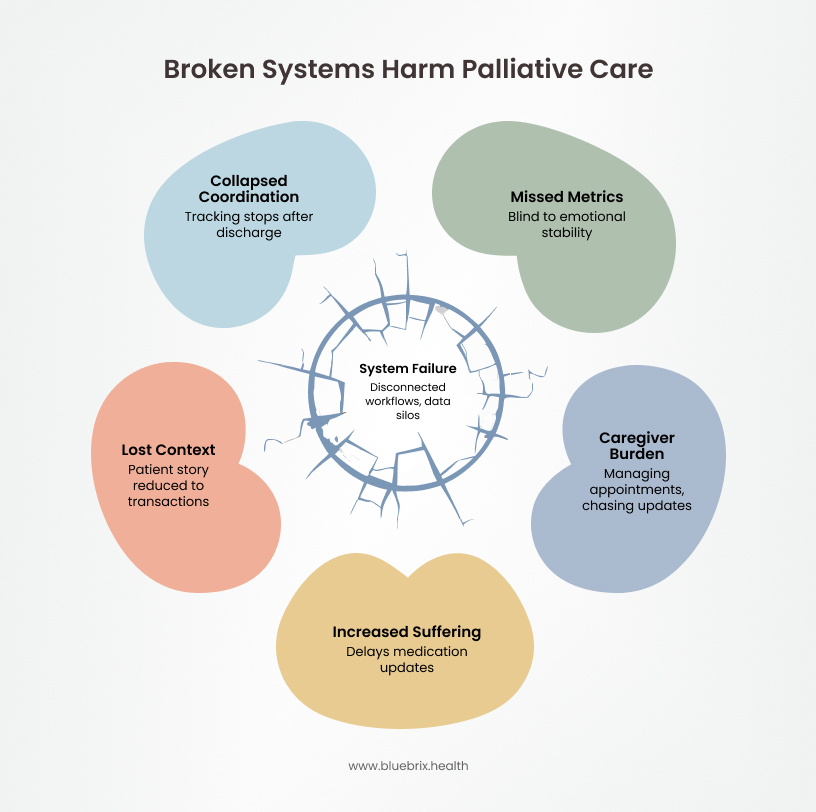
The myth of connected care in palliative settings
Every health system claims it’s integrated; shared EHRs, referral systems, multidisciplinary rounds. But peel back the layers, and you’ll find a hundred disconnected workflows pretending to be one system. The chart updates the data syncs, but the context gets lost. A patient’s story is reduced to a series of transactions. In palliative care, it’s devastating.
Why episodic thinking fails in continuous palliative journeys
Palliative care evolves; it fluctuates, lives between visits. When the system stops tracking after discharge, coordination collapses. The very logic that drives hospital efficiency becomes the reason for palliative care breaks.
What hospital metrics miss: The real measures of palliative success
You can measure length of stay or readmission risk but not fear. You can track vitals, but not peace of mind. And yet, those are the true metrics of palliative success; emotional stability, clarity, and trust. Hospital coordination models are blind to these dimensions because they weren’t designed for “total pain”; the physical, psychological, social, and spiritual layers of suffering that define palliative care.
When caregivers become the system’s backup plan
When systems can’t connect, caregivers take over. They become the de facto coordinators managing appointments, chasing updates, and bridging communication gaps that technology should have solved years ago. It’s not just exhausting; it’s unsustainable.
Data gaps and fragmented communication in palliative care
Existing EHRs and workflows emphasize utilization of metrics like length of stay and readmission rates, neglecting vital quality-of-life indicators such as symptom progression, caregiver burden, and spiritual well-being. Communication is siloed among hospice, home health, and palliative teams, often relying on non-digital methods like phone calls or faxes, which delays medication updates and care adjustments during critical phases.
The human cost of data silos in end-of-life care
When updates move slower than the patient’s decline, or when communication still happens by fax, the result isn’t just inefficiency, it’s suffering. That lag drives readmissions, missed interventions, and moral distress for clinicians who know better but can’t do better inside broken workflows.
Consider a 75-year-old patient with terminal cancer trying to ensure her end-of-life wishes are known and respected. Without advance directive discussions or guidance on hospice options, she ends up in aggressive treatments she never wanted, feeling stripped of control over her final days. This is not a failure of compassion; it’s a failure of coordination.
This isn’t a workflow problem. It’s a design flaw. Palliative care needs its own coordination backbone; one built for continuity, compassion, and human data. Because right now, the system doesn’t just waste resources; it wastes moments that matter.
What a purpose-built palliative coordination model can deliver
If hospital coordination is about managing beds, palliative coordination is about managing journeys. That shift from episodic to continuous, from throughput to trust changes everything.
A purpose-built care coordination model doesn’t just digitize communication; it redefines how teams, patients, and families move together through care. It replaces fragmented updates with shared understanding, and replaces paperwork with presence.
Here’s what that looks like in action.
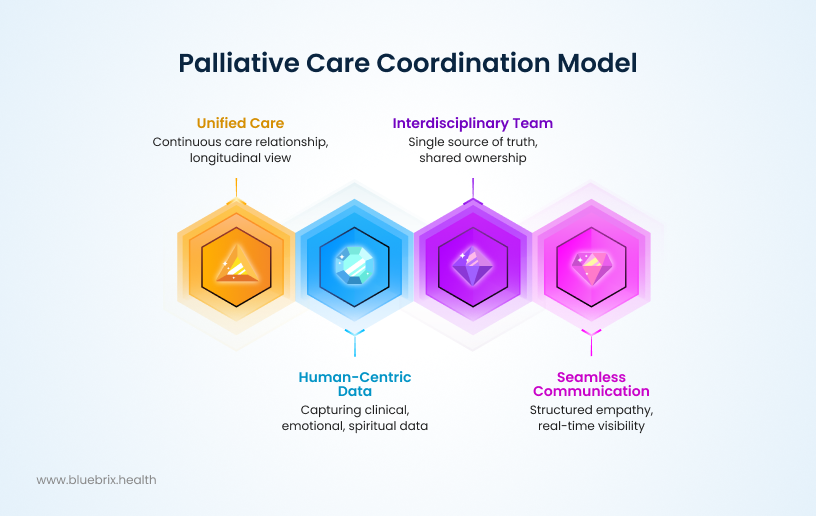
From encounters to continuity: redefining the palliative care journey
In palliative care, every touchpoint matters. A truly effective coordination model isn’t bound by admission or discharge, it follows the patient across every phase: primary, specialty, home health, hospice, and everything in between.
Instead of isolated records scattered across systems, there’s one unified care narrative that adapts as the patient’s goals evolve. It’s not about “episodes of care”; it’s about a continuous care relationship that survives every transition.
This kind of longitudinal visibility changes outcomes immediately. Teams stop reacting to crises and start anticipating needs because they can finally see the whole story, not just the latest note.
Capturing human-centric, multi-dimensional health data
The next big shift is what we choose to measure. Traditional systems focus on vitals and utilization. A purpose-built model captures the full human dataset:
- Clinical symptoms and pain scores
- Emotional distress and spiritual well-being
- Caregiver fatigue and support levels
Because in palliative care, data without humanity is noise. Predictive analytics can surface early signs of symptom escalation or caregiver strain, helping teams intervene before the next hospital visit or crisis call. It’s how compassion becomes proactive, not reactive.
Unifying the interdisciplinary team with a single source of truth
Palliative care doesn’t belong to one clinician. It belongs to an interdisciplinary team (IDT). That team consists of physicians, nurses, social workers, chaplains, caregivers who need a single coordination hub where roles are clear, updates are shared, and accountability is visible.
In a purpose-built care coordination model, every member works from the same real-time view. No “who’s updating the chart” confusion. No missed medication adjustments. Just shared ownership of the patient’s evolving care plan.
When communication is this seamless, the system itself starts to reflect what palliative care was always meant to be; collaborative compassion at scale.
Designing for seamless, compassionate communication
The heart of palliative care is communication between clinicians, families, and the patient themselves. A modern coordination model should embed this into the workflow, not bolt it on.
It’s about giving communication a structure that upholds empathy and dignity, ensuring patients are seen as people, not cases while enabling teams to anticipate needs before they escalate. When clinicians, families, and patients share the same real-time picture, compassion evolves from an individual act to a system-wide outcome.
This is what palliative coordination should look like: Continuous, data-smart, team-driven, and emotionally intelligent.
The systemic payoff: clinical, financial, and human impact
When coordination is designed for continuity, everything changes; outcomes, efficiency, and even morale. This isn’t about making palliative care “nicer.” It’s about making it smarter, sustainable, and measurable in ways hospital frameworks never could.
Clinical outcomes that prove the power of true coordination
When teams share a single source of truth, patients stop falling through the cracks. Real-time updates and predictive analytics mean symptom escalations are caught early, medication changes are made faster, and emergency visits drop.
Hospitals see fewer readmissions. Hospice and home health teams respond with agility instead of playing catch-up. And because the model emphasizes patient-reported outcomes like pain relief, functionality, peace of mind; the quality metrics finally match what matters most to patients and families.
How palliative coordination aligns with CMS and value-based care goals
This model doesn’t just feel right; it aligns perfectly with where the industry is headed. CMS programs like ACO REACH and VBID Hospice are explicitly rewarding what palliative care does best:
- reducing unnecessary hospitalizations,
- ensuring smoother transitions, and
- elevating patient satisfaction.
A longitudinal, patient-centered coordination model directly supports those goals. It creates the data visibility, quality documentation, and outcome tracking that value-based contracts demand.
That means better quality scores, stronger reimbursements, and competitive advantage for organizations ready to modernize.
The dual ROI of better coordination: financial gains and human value
When coordination works, preventable readmissions drop. Emergency visits decline. Resource utilization becomes predictable.
But the deeper return is the human ROI which is even more powerful. Caregivers feel supported instead of overwhelmed. Clinicians spend less time chasing information and more time practicing empathy. Families trust the process because it finally feels like everyone is on the same team.
These intangibles; satisfaction, trust, and emotional safety are eventually translated into tangible results like retention, referrals, reputation, and stronger public trust.
When palliative coordination reflects continuity and relational engagement, not fragmented episodes, the quality, satisfaction, and cost stop being competing priorities. They start reinforcing each other. The system becomes what it was always meant to be:
- clinically sound,
- financially responsible, and
- profoundly human.
That’s the real promise of purpose-built care coordination.
How blueBriX transforms palliative coordination with purpose-built technology
blueBriX is redefining palliative care coordination through a framework built specifically for the realities of continuous, multi-dimensional care. Its model delivers longitudinal visibility across home health, hospice, and specialty providers, creating one unified patient record that evolves with each stage of the journey.
- The platform integrates data beyond traditional EHR boundaries, bringing together clinical, behavioral, psychosocial, and caregiver insights into a single, human-centered view.
- Its AI-driven risk detection flags early signs of symptom escalation or caregiver strain, enabling proactive interventions instead of reactive calls.
- By automating workflows and clearly defining role ownership, blueBriX eliminates coordination ambiguity and ensures every clinician, nurse, and caregiver knows their responsibility in real time.
- Secure communication tools and family-facing portals maintain transparency and trust, while no-code flexibility allows instant adaptation across care sites and programs.
- Fully HIPAA-compliant and aligned with value-based care metrics, blueBriX transforms coordination from fragmented task management into a continuous, compassionate, and intelligent process.
Why modernizing palliative care coordination is an urgent priority for health systems
Palliative care serves people when the stakes are highest. It deserves systems built with the same urgency, empathy, and precision we demand from the clinicians who deliver it.
The U.S. population is aging rapidly, with 61.2 million adults aged 65+ in 2024 (18% of the population), a figure projected to reach 82 million by 2050. Over 76% of adults now live with at least one chronic condition, and cases among those over 50 are expected to nearly double by 2050. Meanwhile, demand for home-based and palliative care is accelerating, with the U.S. home healthcare market projected to grow from $310 billion in 2025 to $474 billion by 2030, and the global palliative care market more than doubling by 2034. Demand is clearly outpacing the capacity of systems still built on hospital-centric frameworks.
Those legacy systems were never designed for longitudinal journeys, and it shows. They can’t deliver the continuity, data transparency, or quality metrics required to compete under value-based reimbursement models like ACO REACH and VBID Hospice. Every delay in modernizing coordination workflows is a missed opportunity; both in revenue and in reputation.
Meanwhile, early adopters are already setting a new standard. Health systems investing in purpose-built coordination platforms are achieving lower readmission rates, better patient satisfaction scores, and higher value-based reimbursements; not because they added more tools, but because they finally built the right foundation.
Waiting isn’t neutral. It’s expensive. Each year of inaction compounds avoidable costs, clinician fatigue, and patient distress. And in an environment where quality, equity, and experience are the new currency, the cost of standing still is far higher than the cost of transformation.