Healthcare’s data backbone is under pressure. Over 70% of IT teams report C-CDA complexity slows application development, while interoperability gaps linked to legacy standards cost the industry nearly $30 billion annually. C-CDA’s XML packages may be comprehensive, but they’re bulky and inefficient when real-time insights are needed. FHIR flips the model—breaking data into modular, API-driven resources that developers can query instantly and leaders can scale across systems. The result? Faster builds, smoother integration, and measurable improvements in care coordination and performance.
In this blog, we’ll outline the best practices healthcare leaders need to navigate this conversion successfully while avoiding common pitfalls.
The push to FHIR: why healthcare is moving beyond C-CDA
When a patient arrives at your emergency department at 2 AM, you need their medical history now—not after navigating through complex document structures to find basic information like allergies or current medications. C-CDA documents, while comprehensive, weren’t designed for the speed and flexibility that modern healthcare demands. Your clinical teams need data that works as fast as they do, and C-CDA’s document-based approach often creates delays when time is critical. FHIR transforms how healthcare data moves through your organization, making the required patient information instantly accessible across departments, systems, and care teams when clinical decisions matter most.
Growing need for interoperability
Your healthcare organization likely runs on dozens of different systems—lab equipment, imaging devices, specialty apps, pharmacy systems. More than 80% of U.S. healthcare organizations are juggling this same complexity, processing thousands of data exchanges daily just to keep operations running.
The challenge isn’t having the data—it’s getting all these systems to actually talk to each other. That’s where FHIR comes in. Unlike the static C-CDA documents you’re probably familiar with, FHIR lets your hospitals, clinics, labs, and pharmacies communicate through standardized protocols that actually work together. The result? A connected ecosystem where your data flows seamlessly instead of getting stuck in silos.
Speed and real-time access
The transition to FHIR supports real-time data retrieval and updates across clinical systems. This means clinicians can instantly access the most current patient information—such as allergies, medications, or test results—precisely when they need it. In emergencies or during acute care, this immediate access enables time-critical decisions that could be life-saving, directly improving care quality, clinical responsiveness, and patient outcomes.
Enhanced patient engagement
FHIR’s web-friendly, API-based architecture provides patients with more accessible and secure methods to access their health records through applications and patient portals. For example, a patient’s wearable device can automatically update their care team about abnormal heart rhythms in real time, prompting the care team to respond quickly and proactively. This enhanced accessibility encourages active patient participation in care management and supports better health outcomes through improved patient engagement.
Regulatory and industry compliance
Government agencies and regulatory bodies, including the U.S. Office of the National Coordinator for Health IT (ONC) and mandates established through the 21st Century Cures Act, are requiring interoperability standards that promote data sharing and patient access rights. FHIR adoption has become increasingly essential for compliance with these regulations and industry certifications, making the conversion from C-CDA to FHIR a strategic necessity for healthcare organizations to meet current and future regulatory requirements.
Moving from C-CDA to FHIR: common pitfalls and how to avoid them
Converting C-CDA to FHIR can be tricky — with most teams stumbling over validation gaps, poorly structured extensions, weak error handling, outdated standards and much more. Here’s a quick breakdown of these pitfalls and how to stay ahead of them.
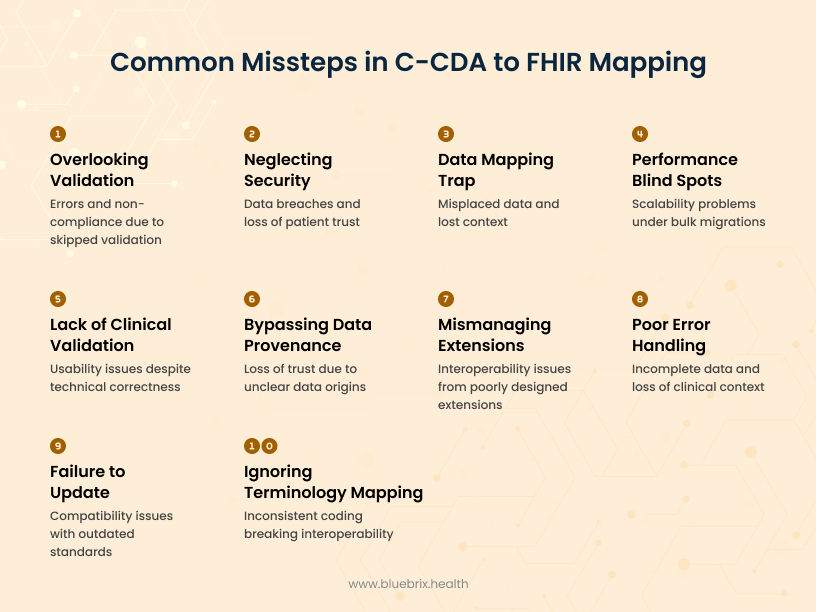
Overlooking validation
Skipping thorough validation of both the source C-CDA and the converted FHIR data can lead to errors, missing information, or non-compliant data that cause issues downstream in clinical systems.
How to avoid: Always use automated validation tools to check for structural correctness, required fields, and proper use of coding standards. Early and ongoing validation helps catch mistakes before they impact patient care or integration workflows.
Mismanaging custom extensions and legacy fields
Healthcare organizations often have unique data elements or legacy fields in their C-CDA documents that don’t fit neatly into standard FHIR elements and require extensions. Poorly designed or inconsistently used extensions can cause interoperability problems, confusion, and data loss.
How to avoid: Define custom extensions and tailored profiles carefully, following FHIR best practices. Document their use clearly and ensure that all systems involved understand and support these extensions to maintain interoperability without data loss. Avoid “ad hoc” extensions that aren’t maintained or standardized.
Poor error handling and data variability
Conversion processes encounter unexpected data issues, but the real challenge is C-CDA’s inconsistent real-world implementation. Different systems leave fields blank, use varying coding systems, or populate optional sections differently, creating missing or inconsistently structured data that can result in incomplete FHIR conversions and loss of clinical context.
How to avoid: Implement comprehensive error logging, validation feedback, and fallback defaults for missing data. Flag problematic entries for clinical review and have remediation processes ready to ensure patient safety and data reliability throughout conversion.
Failure to update with new FHIR/C-CDA versions
Both FHIR and C-CDA standards evolve regularly, adding new elements, modifying existing ones, and updating best practices. Sticking to outdated versions can cause compatibility issues and missed opportunities for improved interoperability and functionality.
How to avoid: Stay informed about the latest HL7 releases and update your conversion tools, mapping guides, and processes accordingly. Regularly review and test your workflows to ensure compliance with new versions and standards.
Ignoring terminology mapping & normalization
Even if the structure converts correctly, inconsistent coding (e.g., SNOMED vs ICD vs local codes) can break interoperability.
How to avoid: Use terminology services to normalize and cross-map codes so allergies, diagnoses, and labs can be consistently understood across systems.
Bypassing data provenance & auditability
After conversion, clinical teams may ask “Where did this data come from?” If provenance isn’t captured, trust in the migrated data suffers.
How to avoid: Always preserve metadata (e.g., source document ID, timestamps, authoring system) to provide a clear audit trail and build confidence in converted data.
Lack of clinical validation
Technical validation alone doesn’t guarantee usability. Data may be correct on paper but confusing or incomplete in a clinical workflow.
How to avoid: Involve clinicians in reviewing migrated records to confirm that the converted data is not just valid, but also meaningful and actionable at the point of care.
Performance & scalability blind spots
A process that works for a handful of records may break under bulk migrations or real-time conversions.
How to avoid: Conduct performance and load testing to ensure your conversion pipeline can scale reliably for large volumes and high transaction rates.
Falling into the data mapping trap
C-CDA’s document-heavy, deeply nested sections rarely align one-to-one with FHIR’s modular resources and fields. Without meticulous planning, it’s easy to misplace details like patient allergies or medication information, or to lose context within hierarchical data.
How to avoid: Break down both standards to understand exactly how data is structured and related. Use standardized mapping templates and test edge cases—especially for sections with many nested elements. Building reusable mapping logic and validating with clinical teams helps catch errors early and ensures the output preserves both meaning and clinical value.
Neglecting security and privacy
Failing to protect sensitive health data during conversion or any lapse in security such as unsecured storage, weak access controls, or unencrypted data transmission can result in serious breaches and loss of patient trust.
How to avoid: Always use encryption and robust access controls during storage and transmission. Limit data access to only authorized personnel or systems at every stage of conversion. Regularly audit processes to ensure compliance and detect potential vulnerabilities before they lead to data exposure.
Best practices for seamless C-CDA to FHIR migration
A smooth C-CDA to FHIR migration depends on the right approach: automate mappings, stick to HL7 standards, validate thoroughly, handle custom extensions properly, support both real-time and bulk conversions, enforce strong security, and continually test and refine. Here’s how to implement these best practices for a seamless shift.
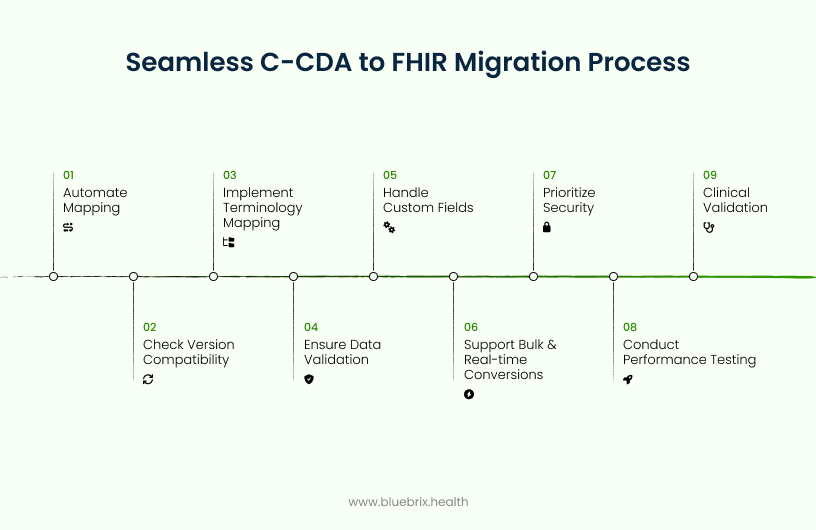
Automate the mapping
Your teams shouldn’t be manually retyping or rearranging patient data from one format to another. Use intelligent software tools or APIs that automatically translate information from legacy C-CDA formats to modern FHIR standards, eliminating manual data entry errors and saving valuable time.
Check for version compatibility
Both C-CDA and FHIR have multiple versions like different software editions—and each organizes data slightly differently. While C-CDA primarily uses Release 2.1 for current implementations, FHIR has evolved through versions like DSTU2, STU3, R4, and R5, each with distinct usage recommendations.
Understanding which versions to use and when is essential to ensure compatibility and smooth data exchange between systems. Below are practical guidelines for selecting appropriate FHIR versions based on interoperability needs:
DSTU2: Use only if you need to support very old, legacy healthcare systems—otherwise, avoid as it’s outdated.
STU3: Use only for connecting with a rare partner still on this version; it’s mostly obsolete for new products.
R4: The industry standard for all modern healthcare apps and integrations—use this for any new or current project.
R5: Consider only if you need cutting-edge FHIR features and all systems involved can support it; not yet mainstream.
Before migrating, identify exactly which versions your systems use and ensure your conversion process handles these differences—think of it as making sure you’re translating between the right editions without losing meaning.
Implement terminology mapping & normalization
Use HL7’s official mapping guides to accurately translate data elements (demographics, allergies, medications, etc.) from C-CDA to FHIR, utilizing coding systems like SNOMED CT, LOINC, RxNorm, CVX, and ICD-10. Since code usage can vary across vendors, integrate terminology services to normalize and cross-map codes, ensuring reliable and consistent data exchange across healthcare systems. Handling ICD-10 mappings may also be necessary to cover diagnoses and billing codes properly, further enhancing the robustness of the mapping process.
Ensure data validation and provenance
Implement comprehensive validation tools to verify both the source C-CDA and the converted FHIR documents for structural correctness, content accuracy, and regulatory compliance. These validators provide real-time feedback and error reporting throughout the migration process, ensuring data integrity. Additionally, capture provenance metadata that tracks the origin and any transformations of the migrated data. This provenance and audit trail enable downstream systems and providers to trace data back to its C-CDA source, maintaining trust, transparency, and accountability in clinical workflows.
Handle custom fields and extensions
Sometimes C-CDA files contain unique or non-standard data that doesn’t have a direct match in FHIR. Instead of throwing this information away, preserve it by using FHIR extensions (extra, well-defined fields you can safely add to a FHIR resource) or tailored FHIR profiles (customized versions of a standard FHIR resource for your specific use case). This way, important details stay intact and remain understandable to other systems. Always set up a process to log and flag any data that couldn’t be mapped directly, so clinical teams can review it and make sure nothing critical is lost during migration.
Support bulk and real-time conversions
C-CDA data is exchanged as large documents, making real-time queries slow and less efficient since the entire document must be processed before specific information can be accessed. To ensure timely and reliable access, implement solutions that pre-process and convert C-CDA documents into FHIR resources ahead of time. This enables seamless handling of both bulk batch migrations and instant real-time data access, supporting smooth workflows during system transitions and daily clinical use.
Prioritize security and compliance
Ensure all data conversions and transfers maintain HIPAA compliance, implementing secure encryption protocols for both data storage and transmission to protect sensitive health information. These security measures should be integrated throughout the entire conversion process, safeguarding patient data while meeting regulatory requirements that govern healthcare information exchange.
Performance testing & continuous monitoring
Conduct load and performance testing to ensure data migrations remain reliable and scalable under peak volumes, preventing system slowdowns or failures. Beyond initial testing, continuously monitor converted data in downstream systems for errors or data loss. Maintain and update conversion logic regularly as FHIR and C-CDA standards evolve. This ongoing testing and monitoring approach safeguards data accuracy and system stability, preventing issues that could disrupt clinical operations or patient care.
Clinical validation with end users
Don’t just check if the data is converted correctly—make sure it actually works for your clinical teams. You are the ones who’ll be using this information to make patient care decisions, so involve them in reviewing the migrated data. They can spot issues that technical validation might miss, like whether critical clinical context got lost in translation or if the data flows logically within your existing workflows. After all, perfectly structured data means nothing if it doesn’t help your clinicians provide better care.

