Understanding value-based care (VBC)
The healthcare landscape is evolving towards a model focused on value, not just volume. This shift is driven by Value-Based Care (VBC), a payment and delivery transformation strategy that incentivizes healthcare providers to deliver high-quality care at a lower cost.
VBC moves away from the traditional fee-for-service model where providers are reimbursed for each service they deliver. Instead, it focuses on outcomes and cost-effectiveness. Under VBC, the healthcare providers are rewarded for meeting specific quality metrics and keeping patients healthy, while penalties are imposed for poor quality care or high costs.
The two pillars of VBC
VBC success pivots on achieving a balance between two key components – Quality & Cost.
- Quality : refers to the effectiveness and appropriateness of the care provided. It involves measuring patient experience, adherence to evidence-based practices and clinical outcomes.
- Cost : focuses on the total cost of care throughout a patient’s journey, including prevention, treatment, and rehabilitation. The resources should be used optimally to reduce unwarranted healthcare costs. It also implies reducing complications, escalations and morbidity which usually contribute to increasing healthcare costs.
While the entire healthcare spectrum is trying to traverse the ever-evolving VBC landscape, VBC is stepping one level up with VBC 2.0.
VBC 2.0: The power of patient engagement
The current iteration, often referred to as VBC 2.0, recognizes the crucial role of patient engagement. Recent research and discussions within our team highlight that achieving patient satisfaction is a key element to VBC success. Patient satisfaction goes beyond simple politeness. It encompasses a sense of empowerment, partnership, and positive perception of the care experience. Empower patients with information and tools, fostering a collaborative partnership, and ensuring they have a positive perception of the entire care experience. Here’s how VBC 2.0 leverages technology and human touch points to cultivate patient engagement and move towards better patient satisfaction:
Technology:
- Patient portals: Empower patients to access medical records, schedule appointments, and communicate with their providers conveniently.
- Telehealth & video consulting: Enables remote consultations, improving access to care and reducing travel burdens.
- Healthcare apps: Offer personalized tools for self-care education, personalized communication, medication management, and symptom tracking.
- Wearable medical devices: Collects real-time information about the patient’s physical activity levels and vitals to be monitored by self and care-providers.
Human touch :
- Shared decision-making: Involves patients actively participating in discussions about their care plan, fostering trust and ownership.
- Empathy and communication: Caring and attentive interactions strengthen patient relationships and promote better adherence to treatment plans.
- Patient-centered care: Tailoring care plans to individual needs and preferences empowers patients and improves satisfaction.
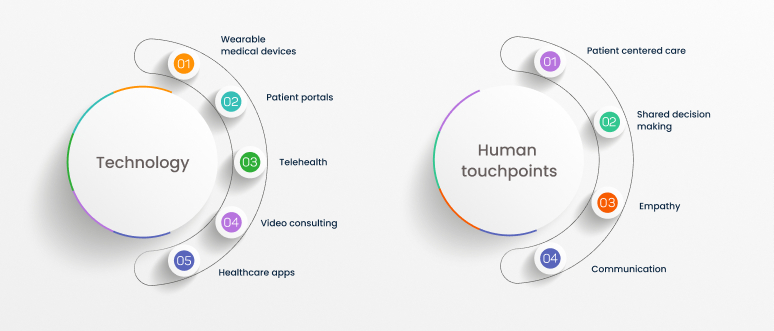
- By strategically combining technology with the human touch, VBC 2.0 creates a patient-centric environment that fosters engagement, improves outcomes, and ultimately leads to higher patient satisfaction. This translates to a positive feedback loop in the VBC model, where happy and engaged patients are more likely to adhere to treatment plans, leading to better health outcomes and lower long-term costs. As far as healthcare providers are concerned, this contributes significantly to retaining patients and acquiring referrals.
The importance of patient satisfaction
Let’s now delve deeper into what patient engagement entails and its impact on patient satisfaction.
Patient engagement: Above & beyond adherence
Patient engagement goes beyond simply showing up for appointments. It’s a collaborative process where patients actively participate in their healthcare journey and includes:
- Understanding their health conditions and treatment options.
- Making informed decisions about their care in partnership with their healthcare providers.
- Taking an active role in managing their health and well-being.
- Following treatment plans and preventive measures.
- Being a proactive part of their own health journey.
Since value-based care models are focused on patient outcomes, engaging regularly with patients to ensure the desired outcome becomes important for the provider. At the same time, the patients also must play their part actively to achieve their desired outcomes. To an extent, wearable medical devices and other technological innovations contribute to achieving this. Building a robust patient engagement framework is essential for succeeding in value-based care.
Framework for patient engagement
Building a framework for patient engagement involves creating a supportive environment that educates, empowers and enables patients. Here are some key elements:
- Communication: Open and transparent communication with clear explanations and two-way dialogue is essential. This, taking care of privacy and federal regulations is key.
- Education: Providing patients with accessible, reliable information about their conditions and treatment options. Equipping patients with an efficient knowledge management system and personalized information sharing helps improve engagement.
- Shared decision-making: Encouraging patients to participate in discussions about their care plan fosters ownership and trust. The provider should understand the patient’s living conditions, health history, occupational, financial and other aspects that could influence their treatment decisions and devise a treatment plan accommodating their preferences. Providing them with ample information about their health conditions, available treatment plans and encouraging them to explore them will help improve their trust. Shared decisions ensure better adherence which eventually results in better outcomes.
- Accessibility: Ensuring patients have easy access to their healthcare providers and resources, both virtually and in-person. Telehealth, video conferencing and remote monitoring contribute to this aspect.
- Respect and empathy: Treating patients with respect, compassion, and understanding is paramount. This is where the human touch points come into play. Until Gen AI or some other technology cracks this aspect, human intervention can take care of empathy.

Tools for patient engagement
Healthcare providers can utilize a variety of tools to promote patient engagement, catering to different needs and preferences. Before we explore the tools, we must understand the patient psyche to gauge if the patient has low or high engagement levels. Based on this, a different strategy and set of tools are chosen by the providers to engage the patients optimally.
Patient engagement levels & their impact on VBC
Patient engagement level can vary significantly from individual to individual. Here’s a breakdown of different levels of engagement and how they translate within the VBC model:
Low engagement: These patients may be passive participants in their care. They might rely heavily on their healthcare providers to make decisions and may not actively seek out information.
VBC impact : Low engagement can lead to poor adherence to treatment plans, potentially resulting in higher costs and poorer health outcomes.
High engagement: These patients are actively involved in their health journey. They take initiative, ask questions, and participate in shared decision-making.
VBC impact : High engagement patients are more likely to adhere to treatment plans, leading to better outcomes and lower costs, positively impacting VBC performance.
Tools for patient engagement
Healthcare providers can utilize a variety of tools to promote patient engagement, catering to different needs and preferences. Before we explore the tools, we must understand the patient psyche to gauge if the patient has low or high engagement levels. Based on this, a different strategy and set of tools are chosen by the providers to engage the patients optimally.
Patient engagement levels & their impact on VBC
Patient engagement level can vary significantly from individual to individual. Here’s a breakdown of different levels of engagement and how they translate within the VBC model:
Low engagement: These patients may be passive participants in their care. They might rely heavily on their healthcare providers to make decisions and may not actively seek out information.
VBC impact : Low engagement can lead to poor adherence to treatment plans, potentially resulting in higher costs and poorer health outcomes.
High engagement: These patients are actively involved in their health journey. They take initiative, ask questions, and participate in shared decision-making.
VBC impact : High engagement patients are more likely to adhere to treatment plans, leading to better outcomes and lower costs, positively impacting VBC performance.

Measuring patient engagement levels
There’s no single “one size fits all” method to categorize patient engagement levels. However, healthcare providers can utilize a combination of tools and observations:
Self-reported measures: Surveys and questionnaires can gauge patients’ level of involvement, understanding, and comfort in managing their health.
Reviewing medical records: Analyzing appointment attendance, medication adherence data, and communication patterns can offer insights into a patient’s engagement level.
Direct observation: Observing interactions during appointments can reveal how actively patients participate in discussions and ask questions.
Patient-reported experience measures (PREMs): Standardized questionnaires assess patients’ perceptions of their care and involvement in decision-making.
Considerations for choosing patient engagement tools
The most appropriate method for measuring engagement depends on your specific needs and resources. Consider factors like:
Patient population: Tailor your assessment approach to the specific demographics and health literacy levels of your patients.
Time constraints: Balance the information you need with the time available for data collection.
Accessibility: Choose methods that are easy for patients to understand and complete.
By understanding patient engagement levels and utilizing appropriate assessment tools, healthcare providers can identify patients who might benefit from additional support. This allows them to tailor their approach and implement strategies to promote higher levels of patient engagement, ultimately contributing to better outcomes and VBC success.
Low engagement tools :
- Patient portals: Offer an easy way for patients to access medical records, view test results, and schedule appointments.
- Text message reminders: Provide convenient nudges for appointments, medication refills, and preventative care measures.
- Automated prescription refills: Streamline medication access and reduce the risk of missed doses.
- Automated appointment reminders: Text messages, emails, or phone calls can nudge patients to schedule or attend appointments.
- Automated medication adherence trackers: Monitor medication refills and refill reminders can be helpful for some patients who need extra support.
- Personalized health summaries: Provide patients with concise summaries of their medical history, medications, and upcoming appointments.
- Educational videos and resources: Offer patients access to reliable health information at their own pace.
- Limited interaction webinars or live chats: Offer opportunities for patients to learn passively from healthcare professionals without requiring active participation.
- Interactive voice response (IVR) systems: Automated phone systems can answer basic questions and schedule appointments but lack personal interaction.
High engagement tools:
- Personalized health apps: Offer features like medication reminders, symptom trackers, and educational content tailored to a patient’s specific needs.
- Online patient communities: Connect patients with others managing similar conditions, fostering peer-to-peer learning and support.
- Wearable devices and health trackers: Allow patients to monitor their health data (e.g., blood pressure, activity levels) and share it with their providers for personalized feedback.
- Gamification elements: Incorporate game-like features like points, badges, and leaderboards into self-management apps to promote healthy behaviors and enhance motivation.
- Real-time health data dashboards: Provide patients with easy-to-understand visualizations of their health data, empowering them to track progress and make informed decisions with their providers.
- Personalized coaching programs: Offer remote or in-person coaching sessions with healthcare professionals or health coaches focused on behavior change and self-management.
- Patient-provider co-creation of care plans: Actively involve patients in developing their treatment plans, fostering a sense of ownership and accountability.
- Telehealth consultations: Facilitate remote appointments, improving access for patients with busy schedules or mobility limitations.
- Video consultations with specialists: Facilitate access to specialized care remotely, reducing travel burdens and increasing engagement with expert opinions.
- Patient support lines: Quick two-way access for one-to-one communication will help ensure adherence, engagement and satisfaction scores which leads to preventive healthcare and better outcomes.
The tools we explored highlight some of the diverse strategies available to promote patient engagement. By offering a spectrum of low- and high-engagement options, healthcare providers can cater to individual needs and preferences. As patients become more comfortable with technology and actively participate in their care, transitioning them from basic tools towards personalized apps, secure messaging, and co-creation of care plans can further enhance engagement.
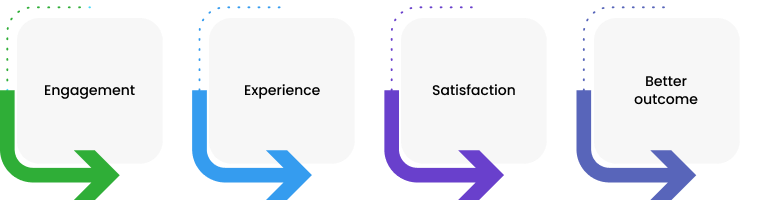
As patient engagement levels increase, patient satisfaction, and patient experience, also increase. That’s how a well-designed engagement strategy can positively impact all three aspects within the VBC framework. Before we move on, let’s understand how closely related, and yet different patient engagement, satisfaction and experience are.
Patient satisfaction vs. patient engagement vs. patient experience
Though these three are closely connected, it’s important to distinguish the core meanings in the healthcare ecosystem:
Patient satisfaction: This refers to a patient’s overall feeling about their care experience. It encompasses factors like courtesy of staff, clarity of communication, and confidence in their provider. High patient engagement can lead to increased satisfaction.
Patient engagement: As discussed above, engagement signifies a more active partnership between patients and providers in managing health. Higher engagement levels result in better outcomes.
Patient experience: This encompasses the totality of a patient’s interactions with the healthcare system, including appointments, communication, and billing. Patient engagement can contribute to a positive patient experience, which in-turn helps retain them and earn the provider more recommendations.
While these terms are distinct, they are interconnected. Fostering patient engagement creates a positive feedback loop. Engaged patients are more likely to be satisfied with their care and have a positive overall experience. This, in turn, leads to better health outcomes and reduced healthcare costs, contributing to VBC success.
Unveiling patient satisfaction: Metrics, payer Influence, and the satisfaction conundrum
Understanding patient satisfaction goes beyond a simple smile or a “thank you.” It’s about quantifying patient experiences to identify areas for improvement and ultimately deliver better care within the VBC framework. Let’s consider the metrics and scores that translate patient experiences into actionable data:
Traditional powerhouses: Standardized surveys
- CAHPS (Consumer Assessment of Healthcare Providers and Systems): Developed by the AHRQ, CAHPS surveys provide a standardized way to assess patient experiences across various healthcare settings. These comprehensive surveys cover areas like:
- Access to care: Ease of scheduling appointments, wait times, and availability of after-hours care.
- Communication with doctors and nurses: Clarity of explanation, ability to ask questions, and feeling listened to.
- Overall care processes: Coordination between providers, information sharing, and discharge instructions.
- Patient experience: Courtesy of staff, cleanliness of facilities, and overall satisfaction with the care received.
- HCAHPS (Hospital CAHPS): This survey focuses specifically on a patient’s hospital stay, measuring factors like:
- Communication with doctors and nurses: Timeliness of communication, clarity of information provided, and responsiveness to patient needs.
- Pain management: Effectiveness of pain medication and attention to patient comfort.
- Hospital environment: Cleanliness of rooms, noise levels, and overall satisfaction with the physical space.
- Discharge planning: Clarity of discharge instructions, follow-up care arrangements, and overall preparedness for transitioning home.
Beyond the averages: Additional metrics and considerations
While CAHPS and HCAHPS provide valuable insights, a multi-pronged approach can offer a more comprehensive picture of patient satisfaction. Here are some additional metrics to consider:
- Net promoter score (NPS): NPS measures patient loyalty by asking how likely they are to recommend the healthcare provider to others on a scale of 0 to 10. Scores are categorized as promoters (9-10), passives (7-8), and detractors (0-6). A high NPS score indicates a strong likelihood of patient recommendation, reflecting overall satisfaction.
- Patient-reported experience measures (PREMs): These standardized questionnaires assess patients’ perceptions of their health and care experience. PREMs can cover a wide range of topics, from symptom severity to treatment effectiveness, offering a more specific look at patients’ perspectives on their health journey.
- Social media sentiment analysis: While not a formal metric, tracking online reviews and social media mentions can provide valuable insights into patient perceptions. Analyzing the sentiment of these discussions can reveal areas of praise and dissatisfaction with your healthcare services.
Beyond the numbers: The human touch
It’s important to remember that patient satisfaction isn’t simply a collection of numbers. While metrics and scores offer valuable insights, it’s crucial to consider qualitative data and anecdotal feedback as well. Tools like open-ended survey questions and focus groups can provide deeper understanding of what truly matters to patients beyond the measured metrics.
By combining quantitative and qualitative data, healthcare providers can identify recurring themes and areas for improvement, ultimately fostering a more patient-centered approach to care delivery within the VBC framework.
Payer and patient satisfaction in VBC: A tangled web
Payers are increasingly integrating patient satisfaction into their VBC payment models. Here’s how it plays out:
- Pay-for-Performance Models: Providers have the chance to earn bonus payments based on exceeding patient satisfaction benchmarks alongside achieving quality and cost-efficiency goals.
- Risk Adjustment: Payers consider a patient’s health status and risk profile when determining reimbursement rates. High patient satisfaction can potentially impact risk adjustment models, as it’s often associated with better health outcomes and lower costs in the long run.
The payer vs. patient conundrum
While patient satisfaction is a vital component, there’s a potential disconnect between payer and patient priorities. The linked article highlights this conundrum:
- Payer focus: Payers might prioritize metrics that demonstrate cost savings when considering patient satisfaction. This could incentivize providers to focus on aspects of care that reduce costs, even if they don’t directly improve the patient’s experience (e.g., shorter appointment times).
- Provider focus: Providers and payers have different perspectives of value. For a provider, the patient’s clinical outcomes and declining readmission rate could be more important than their personal conveniences or work conditions that could be attributed to the outcome.
- Patient priorities: Patients may value factors like having enough time with their doctor or feeling genuinely heard, which might not directly translate to cost reduction. They also expect the provider to consider their preferences in terms of treatment options, timelines and lifestyle changes. Patients would want the providers to help them with their outcomes with minimal lifestyle changes and easier accessibility.
Patient’s values and provider’s priorities tend to be different in a typical healthcare ecosystem. But in value-based care, the payer, provider, and patient priorities must be balanced to assess the desired and actual outcomes to determine the value provided, which in turn determines the provider incentive. This is important for both payers and providers because patient satisfaction and retention will be highly impacted by any imbalance in priorities.
Navigating the maze: A balanced approach
Understanding both payer and patient perspectives is crucial. VBC programs can strive for a more holistic approach by incorporating a variety of patient satisfaction metrics alongside clinical outcomes and cost data. Here are some additional considerations:
- Tailored Surveys: Different patient populations might value specific aspects of care. Developing targeted surveys and assessments can offer more nuanced insights into patient satisfaction.
- Identifying Areas for Improvement: Patient satisfaction data can be a goldmine for identifying areas for improvement in the patient’s experience. Addressing these issues leads to better overall care delivery, ultimately benefiting both patients and the healthcare system.
By effectively utilizing these tools, addressing the payer vs. patient satisfaction conundrum, and implementing a balanced approach, VBC programs can create a system that prioritizes both high-quality, cost-effective care and a positive patient experience, driving better health outcomes for all stakeholders.
History of digital health solutions for care delivery
The landscape of healthcare is undergoing a dramatic transformation fueled by digital technologies. This evolution has fundamentally reshaped patient experience, moving from a passive, record-centric approach to one that prioritizes patient engagement and satisfaction.
Early days: Limited focus on engagement
The history of digital health solutions is relatively young. The term “e-health” emerged in 1998, marking the beginning of a new era. Initial efforts primarily focused on Electronic Health Records (EHRs), offering limited patient engagement beyond basic patient portals.
The ACA ushers in change
The Affordable Care Act (ACA) played a pivotal role in shifting the focus towards patient engagement. By incentivizing preventive care and value-based care models, the ACA emphasized the importance of patient participation in managing their health.
The rise of patient engagement
The widespread adoption of smartphones and wearable devices like Fitbit further fueled the patient engagement movement. These technologies empowered individuals to actively track their health data, fostering a sense of ownership and control.
The value-based care imperative
The current shift towards value-based care models has further underscored the need for patient engagement. Since payments are now tied to outcomes and satisfaction, healthcare providers must prioritize patient involvement to achieve success.