If there is one thing every healthcare team agrees on, it is that authorizations can make or break a smooth patient journey. A single missed approval can delay a procedure, upset a patient, and slow down the entire revenue cycle. But when authorizations run well, everything feels lighter. Patients get the care they need on time, and organizations get paid without unnecessary back and forth.
Think about a typical patient visit. Someone comes in with knee pain, gets recommended an MRI, and assumes things will move quickly. Behind the scenes, the RCM team has already checked the insurance plan, confirmed whether prior approval is needed, and gathered the right clinical notes. By the time the patient shows up for the scan, everything is cleared. No surprises. No last minute cancellations. No stress. That is the power of strong pre authorization.
But healthcare is unpredictable. Emergencies happen. Patients show up needing urgent care without time to wait for payer approval. This is where post authorization steps in. It gives providers a window to secure payer approval after the service has been delivered. It is not the preferred route, but it often prevents revenue from slipping through the cracks and ensures patients are not penalized simply because their care could not wait.
Together, pre and post authorization shape how care flows and how revenue is protected. They help avoid denials, keep organizations compliant with constantly changing payer rules, and make the patient experience more reliable.
Now that we have set the stage, let us walk into the world of pre authorization and understand why it is often considered the first line of defense in revenue cycle management.
Understanding pre-authorization
Pre authorization often gets framed as a routine administrative formality, but anyone in revenue cycle knows it is much more than that. It is the first gatekeeper that determines whether a claim will fly through adjudication or quietly turn into a denial that resurfaces weeks later. For many organizations, this step is the difference between steady cash flow and chronic leakage.
At a functional level, pre authorization verifies two core questions:
- Is this service medically necessary based on payer criteria?
- Will the plan cover it under the patient’s current benefits?
Simple questions, but the complexity lies in the fact that payer rules change frequently, medical necessity criteria can vary by specialty, and coverage depends on precise documentation and coding. Even small errors create significant friction later in the cycle.
A practical view of how it works behind the scenes
When a provider recommends a service like a lumbar MRI or a specialty infusion, the RCM team quickly evaluates three things:
- The patient’s eligibility and benefit limitations
- Whether the CPT code triggers pre authorization under the payer
- What clinical documentation the payer requires (which often changes without warning)
If the service requires approval, the RCM team essentially builds a case file. They align diagnosis codes, gather clinical notes that justify medical necessity, and submit everything through the payer’s preferred channel. A well prepared submission can cut turnaround time significantly, especially for high volume specialties like radiology or behavioral health.
This is why strong pre authorization teams function almost like compliance specialists. They know payer patterns, common denial triggers, and how to structure requests that move quickly through review.
Why pre authorization matters so much
Getting pre authorization right is more than just compliance. It prevents headaches for everyone involved.
Better payer alignment: Payers frequently adjust their rules and criteria. Pre authorization ensures the provider’s request matches the payer’s expectations from the start. When that alignment is missing, denials follow.
Fewer delays and fewer denials: Most denied claims have something in common. The service either had no prior authorization or had incomplete documentation. By handling this step early, RCM teams avoid unnecessary rework and speed up reimbursement.
Clearer financial expectations for patients: When patients know upfront that their insurance covers the service, they feel more secure. Nobody wants a surprise call saying their procedure is postponed because the approval did not go through.
An Example: Consider a psychiatry clinic requesting approval for a complex medication regimen. Payers often require documentation showing the patient has tried other treatments first. If the submission is missing even one progress note, the request stalls. That delay does not just push back reimbursement. It affects the patient’s ability to start treatment on time, and it increases the administrative work needed to resubmit, appeal, or correct the request. A proactive RCM team, however, knows what each payer typically asks for, prepares the full documentation packet upfront, and often secures approval in the first attempt. This improves both clinical continuity and revenue reliability.
Now that the role of pre authorization is clear, the next step is understanding where it happens most often. Different specialties face different authorization rules, documentation needs, and CPT level requirements.
Specialties that commonly require pre authorization
Not all services trigger the same level of payer scrutiny. Some specialties carry higher clinical risk, higher cost, or a history of inconsistent utilization. These are the areas where payers tighten their rules, making pre authorization a standard expectation.
Understanding why these specialties are targeted helps RCM teams prepare stronger, cleaner submissions and avoid predictable denials.
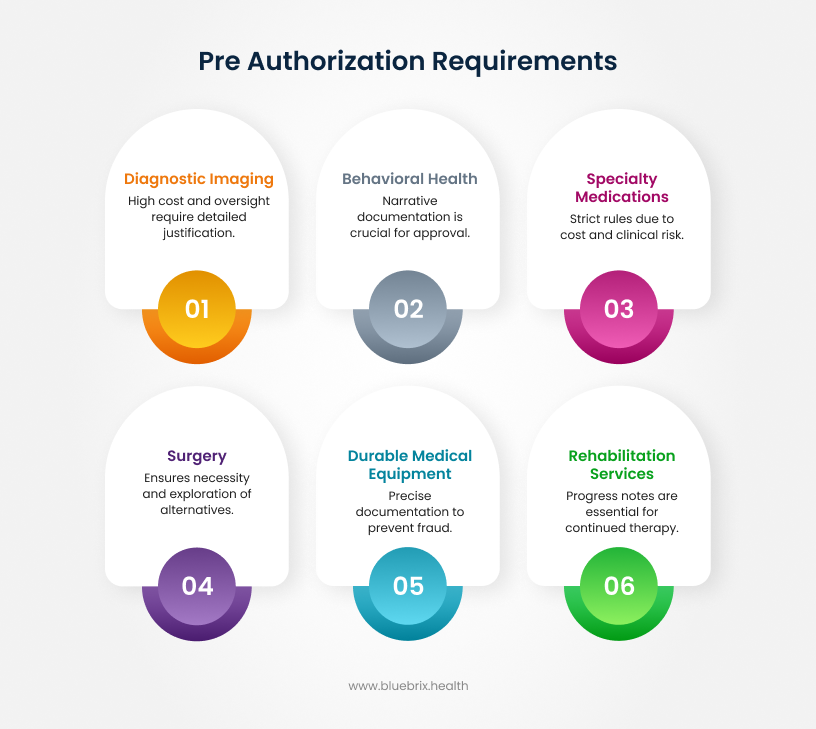
1. Diagnostic imaging: high cost, high oversight
MRIs, CT scans, PET scans, and nuclear medicine studies are some of the most frequently reviewed services. Payers watch these closely because:
- They involve significant cost
- Overutilization is common without strict guidelines
- Many plans require proof that conservative treatment failed before approving the scan
For RCM teams, this means securing detailed clinical notes, previous treatment attempts, and any prior imaging reports to justify medical necessity.
Example: For an MRI of the lumbar spine, many payers expect documentation of at least six weeks of conservative therapy unless red flag symptoms are present.
2. Behavioral health: documentation depth matters
Behavioral health has expanded rapidly, and so has payer scrutiny. In this space, pre authorization may be required for:
- Inpatient psychiatric admissions
- Partial hospitalization programs
- Intensive outpatient programs
- Continued therapy sessions beyond initial limits
- Certain psychiatric medications
Payers want to verify diagnosis accuracy, medical necessity, and ongoing progress. Incomplete treatment plans or missing progress notes are common reasons for delays.
Why this matters: Behavioral health documentation is narrative heavy, so missing details can easily lead to stalled authorizations.
3. Specialty medications and infusions
Biologics, injectables, and specialty pharmacy medications are among the costliest services in healthcare. Payers expect:
- Proof of diagnosis
- Lab results
- Evidence of previous therapies
- Step therapy compliance
This area often has the strictest authorization rules due to cost and clinical risk.
Example: For autoimmune biologics, payers may require documentation showing failure of two or more first line treatments.
4. Surgery: from elective to complex procedures
Most elective surgeries and some medically necessary ones need pre authorization, including:
- Orthopedic surgeries
- Cardiac interventions
- Gastrointestinal or bariatric procedures
- ENT and neurosurgical operations
Payers want to ensure that surgery is indicated and that all conservative options were explored first.
Operational insight: Missing pre authorization for surgery does not just cause delays. It disrupts OR scheduling, frustrates patients, and creates major financial risk for the provider.
5. Durable medical equipment (DME)
Devices like wheelchairs, CPAP machines, oxygen supplies, and infusion pumps often require prior approval. Payers typically look for:
- Proof of functional limitations
- Test results (for example, sleep studies for CPAP)
- Long term treatment plans
Because DME claims have historically faced fraud concerns, documentation must be precise.
6. Rehabilitation and therapy services
Physical therapy, occupational therapy, and speech therapy often require authorization after a certain number of sessions. Payers evaluate:
- Baseline functional assessments
- Progress toward goals
- Medical necessity for continued therapy
Missing progress notes is one of the top denial triggers in this category.
These specialties highlight how varied and detailed heavy authorization requirements can be. The real challenge is not just knowing what needs approval, but understanding how the authorization process actually moves from start to finish. Every step, from reviewing the chart to tracking the payer’s response, plays a role in preventing delays and securing clean claims.
The next section walks through the actual workflow inside a pre authorization process and the checkpoints where RCM teams make the biggest impact.
Inside the pre authorization workflow
A strong pre authorization workflow is not just a checklist. It is a coordinated sequence of steps that determines whether care moves forward without interruption or gets stuck in back and forth with the payer.
A well built workflow reduces delays, prevents denials, and helps clinical and administrative teams stay aligned. Here is how it typically works behind the scenes.

Step 1. Reviewing the patient chart: finding the story behind the request
The process starts with understanding why the service is being ordered. The RCM team reviews:
- The diagnosis
- Clinical notes
- Prior treatments or test results
- Any red flag symptoms or clinical justification
This step is important because payers do not just approve services. They approve medical necessity, and that narrative must be clear and consistent.
Key insight: Even a strong clinical case can be delayed if documentation does not clearly support the request.
Step 2. Eligibility and benefits verification: confirming what the plan allows
Next, the team checks the patient’s insurance details. This step confirms:
- Whether the patient is currently covered
- What benefits apply
- Whether pre authorization is required
- Any limits, exclusions, or step therapy rules
A missed detail here can cause cancellations or surprise out of pocket costs for patients.
Step 3. Determining requirements based on cpt codes and payer rules
This is where precision matters. A single CPT code can determine:
- Whether pre authorization is needed
- What documents must be attached
- Which payer policies apply
Since rules vary by payer and often change, this step requires timely information and sometimes payer portal checks.
Operational reality: Wrong or outdated CPT codes are a leading cause of preventable delays.
Step 4. Submitting the request: packaging the case for approval
Once everything is validated, the request is submitted along with clinical documentation. Depending on the payer, RCM teams may use:
- Online portals
- Integrated ePA tools
- Fax submissions
- Phone based approvals
Strong submissions anticipate payer questions before they arise. This reduces back and forth and cuts turnaround times.
Step 5. Tracking, following up, and resolving requests
This is where many organizations lose time and revenue. A good tracking process ensures:
- Every request is monitored
- Status updates are not missed
- Additional information is provided quickly
- Denials are caught early
Without active monitoring, even approved authorizations can be delayed simply because responses were overlooked.
When these steps work together, the entire organization benefits:
- Clinics avoid last minute cancellations
- Physicians get faster confirmation
- Billing teams submit cleaner claims
- Patients receive care without delays
- Revenue moves without unnecessary obstacles
But even with a strong workflow, pre authorization still comes with challenges. In the next section, we will look at the most common challenges organizations face in pre authorization and why these bottlenecks continue to drain time and resources.
Common challenges in pre authorization
Even the best workflows can be tested by the realities of pre authorization. The process touches multiple teams, involves multiple systems, and depends heavily on payer clarity, which is often inconsistent. This combination creates friction that RCM teams deal with daily.
Here are the challenges that appear the most and why they continue to complicate the process.
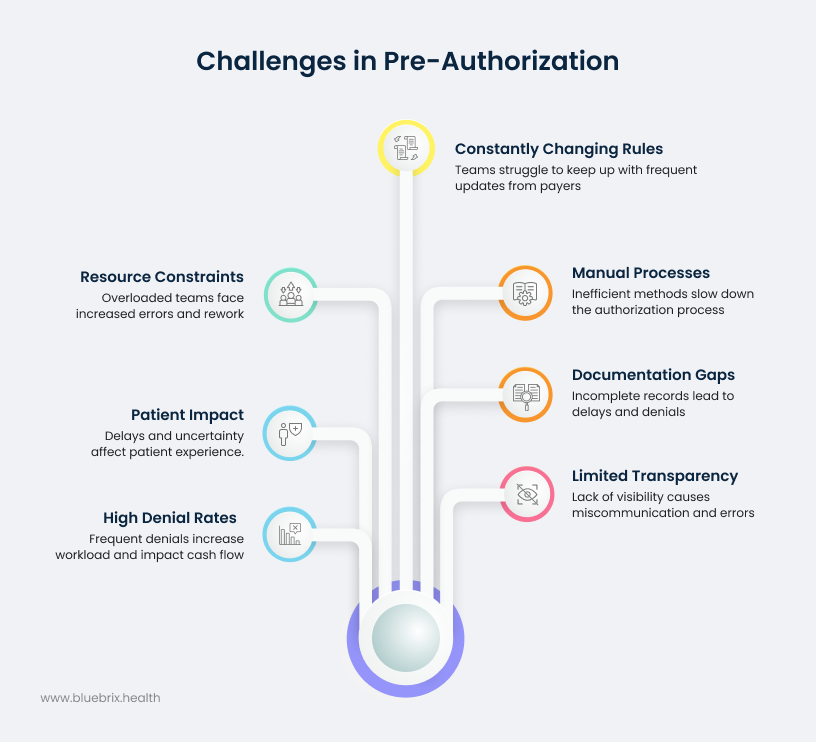
1. Constantly changing payer rules
Payers update their medical necessity criteria, documentation requirements, and approval protocols with little notice. For RCM teams, this means:
- Yesterday’s correct submission can become today’s denial
- Staff must track multiple rule sets across multiple payers
- Policies change by plan, not just payer
This variability forces teams to stay in constant learning mode.
2. Manual processes that slow everything down
Fax based submissions, long hold times, and portal hopping drain staff productivity. The result:
- Extended wait times for decisions
- Higher risk of missing information
- Delays that spill into the clinical schedule
Manual work also increases the chance of errors that could easily be avoided.
3. Documentation gaps that trigger delays
Many denials do not happen because the service was inappropriate. They happen because:
- Notes were incomplete
- CPT and diagnosis codes did not align
- Prior treatments were not documented
- Required attachments were missing
These small gaps create big roadblocks.
4. Limited transparency across the workflow
Clinicians, front desk teams, and RCM staff often do not have a unified view of authorization status. This causes:
- Duplicate efforts
- Miscommunication
- Scheduling issues
- Surprise denials
Without clear visibility, responding quickly becomes almost impossible.
5. High denial rates and time consuming appeals
When an authorization is denied, the rework begins. Appeals require:
- Updated documentation
- Medical necessity explanations
- Phone or portal follow up
- Resubmissions
Each denial can cost significant time and directly impact cash flow.
6. Patient impact that cannot be ignored
Patients often experience the effects directly. Missed authorizations lead to:
- Rescheduled procedures
- Delayed treatments
- Uncertainty about costs
- Frustration and lost trust
From a patient experience standpoint, authorization delays can feel like the system is working against them.
7. Resource constraints across RCM teams
High request volumes combined with staff shortages create pressure to move quickly, which increases the risk of:
- Errors
- Missed follow ups
- Incomplete submissions
This leads to a cycle where overloaded teams face even more rework.
These pain points do not exist in isolation. Together, they slow approvals, deepen administrative burden, and increase denial risk. They also impact the organization’s ability to deliver timely care, maintain cash flow, and keep patient confidence high.
But some authorizations cannot be obtained beforehand. Emergencies, urgent care needs, and unpredictable scenarios make pre authorization impossible. In the next section, we look at what happens when this step is missed and how post authorization supports both patient care and revenue recovery.
When pre authorization is missed: the role of post authorization
Even with strong workflows, well trained teams, and automated tools, healthcare is unpredictable. Patients arrive with urgent needs, physicians make time sensitive decisions, and some situations simply cannot wait for payer approval. When this happens, organizations depend on post authorization to protect both the patient and the provider.
Post authorization, also called retroactive authorization, allows RCM teams to request approval after the service is already provided. It is not the preferred route, but it is an essential safety net.
Why post authorization exists
Post authorization acknowledges a basic truth in healthcare. Sometimes care must come first, paperwork second. Typical situations include:
- Emergency room visits
- Urgent surgical interventions
- Sudden behavioral health crises
- Hospital admissions where delay could worsen the patient’s condition
In these scenarios, stopping to obtain pre authorization is not clinically responsible or even possible. Post authorization provides a structured way to justify the care that was delivered and secure reimbursement afterward.
How the process works
While it mirrors pre authorization in concept, post authorization has a more compressed and high stakes workflow. RCM teams must:
- Collect all clinical documentation related to the emergency or urgent need
- Explain why pre authorization could not be obtained
- Submit justification that clearly demonstrates medical necessity
- Follow payer specific timelines, which are often extremely short
- Respond quickly to any additional documentation requests
The key difference is that payers scrutinize retroactive requests more closely because the service has already occurred.
Why it is more challenging than pre authorization
Post authorization is harder for several reasons:
- Approval is less predictable
- The burden of proof is higher
- Timelines are tighter
- Missing documentation carries more risk
- Some payers only allow retroactive requests in specific clinical situations
If the justification is weak or submitted late, denial is likely. This is why organizations treat post authorization as a corrective measure, not a routine workflow.
The impact on patient access and provider revenue
When handled well, post authorization:
- Prevents unnecessary write offs
- Ensures emergency care is reimbursed
- Supports continuity of treatment
- Protects patients from unexpected financial responsibility
But if mismanaged, it can:
- Trigger denials that lead to revenue loss
- Complicate patient billing conversations
- Expand administrative workload
- Create gaps in the patient’s ongoing care plan
RCM teams that respond quickly, submit strong clinical narratives, and track payer timelines closely have the highest success rates.
Now that we understand when and why post authorization comes into play, the next step is to explore how payers decide whether to grant retroactive approvals and what rules govern this process. That clarity helps teams act fast and improve approval outcomes when pre authorization cannot be secured in advance.
When and why retroactive approvals are permitted
Retroactive approvals sound generous at first glance, but payers do not allow them freely. They are permitted only in specific scenarios where the provider can prove that care could not wait, documentation supports medical necessity, and the absence of pre authorization was unavoidable rather than operational oversight.
Understanding these conditions helps RCM teams move quickly and build stronger cases when post authorization becomes necessary.
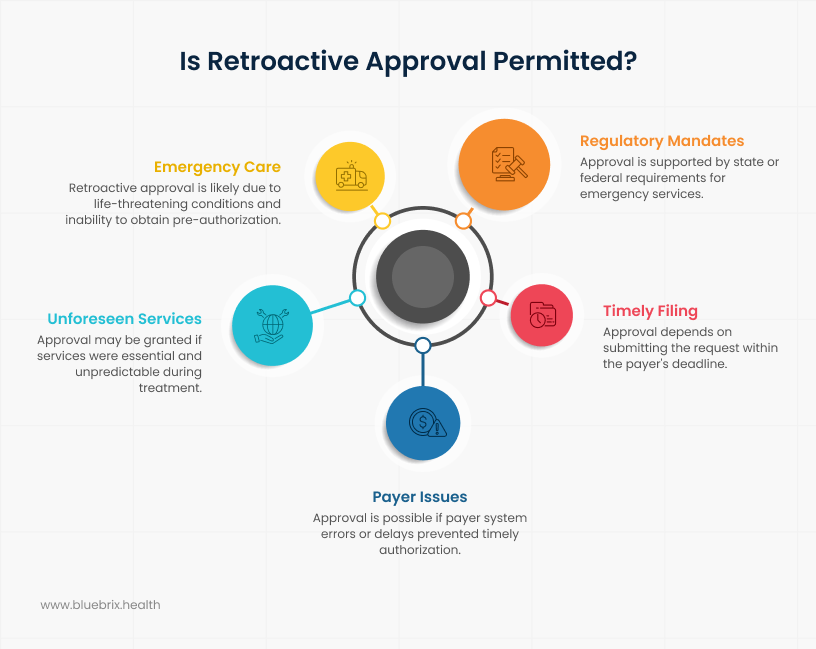
1. Emergencies where delaying care was not an option
This is the most common and most universally accepted scenario. Payers allow retroactive approvals when:
- A patient’s condition was life threatening
- Delaying intervention would have caused harm
- There was no reasonable possibility of obtaining pre authorization
Examples include chest pain requiring immediate imaging, traumatic injuries, acute psychiatric crises, or complications during an ongoing procedure.
What payers expect: Documentation must clearly show why the situation qualified as urgent or emergent and why waiting for approval was not clinically safe.
2. Unplanned or unforeseen services during treatment
Sometimes care evolves during a procedure or hospital stay, leading clinicians to perform additional services that were not originally anticipated.
Retroactive approval may be permitted if:
- The need emerged during surgery or ongoing treatment
- The additional service was essential to prevent complications
- The change in care plan could not have been predicted
Example: A surgeon discovers an unexpected complication during a procedure and must extend or modify the surgery.
3. Gaps caused by late coverage updates or payer system issues
Though less frequent, retroactive approvals also happen when the payer’s own systems or delays prevented a timely pre authorization. This includes situations like:
- Delayed eligibility updates
- Incorrect payer information provided by the member
- System outages that prevented timely submission
When approved: Only if the provider can demonstrate that the attempt to obtain pre authorization was made but blocked due to payer side issues.
4. Timely filing allowances within strict windows
Most payers allow retroactive authorization only if the provider submits the request within a narrow timeframe. Common windows include:
- 24 hours
- 48 hours
- 72 hours
- For some Medicaid plans, up to 7 to 14 days
Requests submitted beyond the payer’s window are almost always denied unless the case involves extreme medical necessity.
5. State or federal requirements that mandate exceptions
Certain state regulations or CMS guidelines require emergency services to be covered even when pre authorization was not possible. Payers still request documentation, but the regulatory framework gives providers additional support in securing retroactive approval.
Knowing when retroactive requests are legitimate helps teams:
- Avoid wasted effort on cases that will not qualify
- Prioritize cases where approvals are more likely
- Ensure documentation is collected at the right time
- Submit requests within the payer’s deadline
- Reduce the number of preventable denials
The key is speed and precision. The sooner the request is submitted and the clearer the justification, the higher the chances of approval.
The next section looks at how organizations strengthen their overall authorization structure. We explore the standards, documentation practices, and payer specific tracking methods that help teams maintain control across both pre and post authorization.
Building a seamless and scalable authorization workflow
A smooth authorization workflow does not happen by accident. It is created through intentional alignment of teams, documentation, technology, and payer requirements. When every element works together, authorizations stop being a bottleneck and become a predictable part of patient care and revenue protection.
Below are the core elements that create a reliable, scalable, and efficient authorization system.
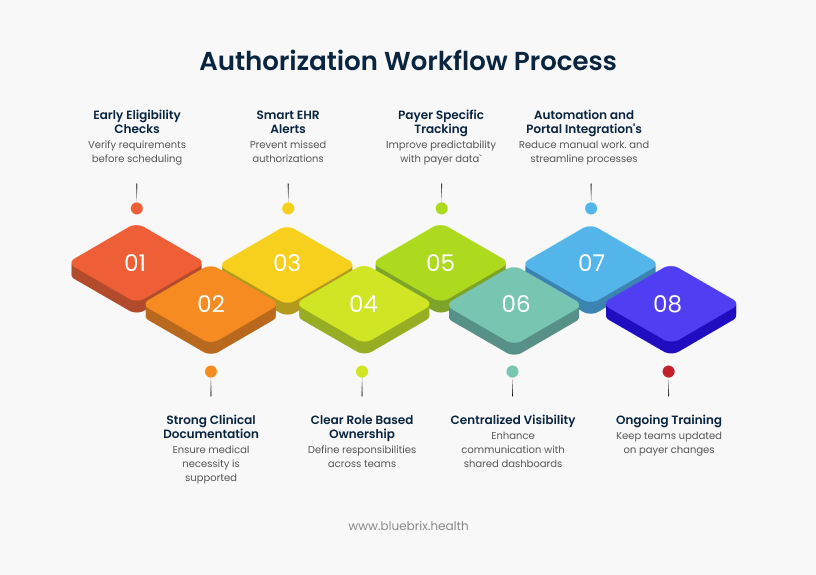
1. Early eligibility checks that detect requirements before scheduling
The workflow begins at intake or scheduling. Early eligibility and benefits verification helps teams immediately identify:
- Whether prior authorization is required
- What documents or clinical details the payer expects
- Any plan specific limits, step therapy rules, or exclusions
This prevents last minute cancellations, reduces patient disruptions, and gives teams enough time to prepare a complete, compliant request.
2. Strong clinical documentation that supports medical necessity
Approvals rely heavily on how well the patient story is captured. Strong documentation standards ensure:
- Clinical notes clearly support medical necessity
- Prior treatments and outcomes are documented
- CPT and diagnosis codes match the clinical scenario
- Diagnostic reports or required attachments are included
- Progress notes support continued care requests
This upfront alignment improves first pass approvals and shortens turnaround time.
3. Smart EHR alerts that prevent missed authorizations
Many delays occur because teams simply do not realize authorization is required. Helpful EHR alerts include:
- Prompts for high cost imaging
- Flags for DME items requiring payer validation
- Notifications when therapy visits approach plan limits
Timely reminders help clinicians and staff act before a case becomes urgent.
4. Clear role based ownership across teams
Authorization involves multiple departments, so role clarity is critical. A seamless workflow defines responsibilities such as:
- Front desk teams verifying insurance
- Clinical teams completing documentation
- RCM teams submitting and following up
- Managers handling high risk or high cost cases
Clear accountability prevents delays, duplication, or missed steps.
5. Payer specific tracking for better predictability
Since every payer operates differently, tracking their rules and behavior improves accuracy and planning. Effective tracking includes:
- Average processing times
- Common denial reasons
- Required documentation sets
- Retroactive approval windows
- Turnaround times and follow up intervals
This allows teams to anticipate challenges, reduce variability, and refine workflows based on real data.
6. Centralized visibility across the workflow
Authorization spans intake, clinical teams, and RCM. Shared dashboards or integrated tracking allow teams to see:
- Which requests are pending
- Which cases need additional documentation
- Which are nearing deadlines or at risk
- Which approvals are complete
Unified visibility eliminates miscommunication and prevents interruptions in patient care.
7. Automation and portal integrations that hold the process together
Technology supports the workflow by reducing manual work and creating real time visibility. Automation helps teams:
- Auto populate payer forms
- Validate codes and clinical details
- Submit requests directly to payer portals
- Track status updates in real time
- Flag cases that need staff attention
Portal integrations further reduce administrative burden and keep the process moving without delays.
8. Ongoing training that keeps teams ahead of payer changes
Since payer rules and medical necessity criteria evolve frequently, ongoing training ensures staff can adapt quickly. High performing teams stay updated on:
- New payer policies
- Revised documentation expectations
- Updated regulatory requirements
This prevents errors and strengthens compliance across the workflow.
The outcome: a controlled, predictable, and patient friendly process
When eligibility checks, documentation standards, role clarity, payer tracking, and automation work in harmony, organizations see:
- Faster approvals
- Fewer denials
- Cleaner claims
- Timely care delivery
- More stable cash flow
Instead of scrambling to fix issues later, teams prevent problems before they disrupt schedules or revenue. What once felt like a reactive burden becomes a controlled, dependable system that supports both care quality and financial integrity.
In the next section, we will look at how technology and the right automation tools help reduce these recurring pain points and create a more predictable, scalable authorization process.
How technology and automation improve accuracy, efficiency, and turnaround time
Even with strong workflows and skilled staff, traditional authorization processes remain vulnerable to errors, delays, and heavy administrative load. Technology fills these gaps by eliminating repetitive work, improving documentation quality, and creating fast, reliable communication loops between providers and payers. Instead of replacing teams, it strengthens them, helping organizations shift from reactive firefighting to predictable, high speed authorization cycles.
A structured workflow paired with the right automation tools ensures every step happens consistently: eligibility checks occur before scheduling, documentation is reviewed before submission, and follow ups happen on time. This consistency builds accuracy, reduces denials, and prevents the cycle of rework.
Below is how technology transforms the process end to end.
1. Reducing manual errors through smart automation
A large portion of authorization work involves handling data across multiple systems. Automation improves accuracy by:
- Pulling demographics and insurance details directly from the EHR
- Auto populating payer specific forms
- Validating CPT and ICD codes
- Checking for missing or mismatched documentation
- Ensuring required attachments are included
These checks eliminate common errors like incorrect codes, incomplete notes, or missing clinical details, which are among the top drivers of preventable denials.
2. Faster submission with electronic prior authorization (ePA)
Electronic prior authorization tools speed up submission by replacing phone calls, faxes, and manual portal navigation. ePA systems can:
- Send requests instantly
- Route submissions through API connections where available
- Flag missing information in real time
- Accelerate payer review
What previously took days often gets completed in minutes for straightforward cases.
3. Real time status tracking to prevent missed follow ups
One of the biggest sources of delays is simply losing track of requests. Modern platforms eliminate guesswork with:
- Real time updates from payer portals
- Alerts when payers request additional documentation
- Notifications for deadlines and expiring authorizations
- Dashboards that display all cases at a glance
Teams stay proactive, preventing avoidable delays and last minute surprises.
4. Strengthening documentation and coding accuracy
AI assisted document checks give teams an extra layer of quality control by identifying:
- Missing medical necessity details
- Coding inconsistencies
- Documentation gaps
- Conflicts between clinical notes and requested services
By prompting corrections before submission, teams can send cleaner, more complete requests that stand a better chance of quick approval.
5. Robotic process automation (RPA) for high volume tasks
RPA takes over the repetitive, time consuming steps that burden staff, such as:
- Checking payer portals for updates
- Uploading attachments
- Copying data into forms
- Logging status changes
This frees staff to focus on complex cases and patient communication instead of spending hours on routine administrative work.
6. Actionable insights for continuous improvement
Technology platforms generate valuable analytics that highlight:
- Payers with the longest response times
- CPT codes with high denial risks
- Recurring documentation issues
- Turnaround time trends by specialty
Leaders can use these insights to refine workflows, adjust staffing, train teams, and collaborate with providers to improve documentation standards.
7. Better experiences for patients and providers
When processes run smoothly:
- Patients experience fewer delays and cancellations
- Providers get faster authorization decisions
- Staff spend less time on manual tasks and more time supporting care
This creates a dependable environment that improves satisfaction across the board.
Why technology makes such a big difference
Technology brings speed, accuracy, and visibility to a process that otherwise depends heavily on manual effort. When automation supports the workflow:
- Approvals move faster
- Denials decrease
- Staff workload drops
- Patients experience fewer delays
- The revenue cycle becomes more predictable
It transforms authorization from a time consuming administrative task into a controlled, efficient component of care delivery.
With technology enhancing accuracy and speed, it becomes easier for RCM teams to manage authorization across the entire care journey.
In short, technology and automation turn authorization from an unpredictable, error prone process into a controlled, efficient system that protects revenue, accelerates care, and strengthens the entire RCM operation.


