In the world of behavioral health, care is deeply human—but the systems meant to support it often fall painfully short.
Ask any behavioral health provider, and they’ll tell you: the technology they’re handed wasn’t built for what they do. Generic EHRs treat therapy sessions like checkups, group therapy like a billing anomaly, and trauma-informed care like an afterthought.
For a field rooted in empathy, context, and complexity, this kind of tech mismatch isn’t just frustrating—it’s harmful.
Let’s talk about why that actually happens—and how some providers, like Laurel Life, are breaking that cycle with behavioral-health-first solutions like blueBriX.
The Behavioral Health Gap: Where Traditional Systems Fail
Most EHRs and care platforms are built for general medicine. They’re designed around labs, prescriptions, and procedures, not long conversations, emotional safety, or social context.
But behavioral health is different. It’s dynamic, decentralized, and deeply relational.
Here’s what that looks like day to day:
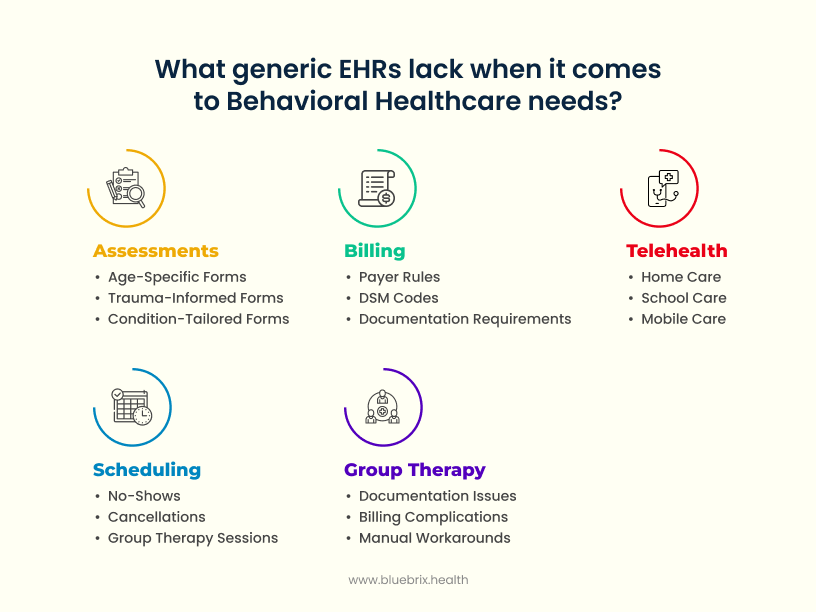
Assessments Aren’t One-Size-Fits-All
Clinicians need age-specific, trauma-informed, condition-tailored forms. Generic templates force them to “make do,” which leads to duplicated work and inaccurate records.
Scheduling Is a Constant Juggling Act
From no-shows and cancellations to back-to-back group therapy sessions, scheduling in behavioral health is anything but simple. Systems that can’t adapt create chaos and idle time.
Group Therapy Is a Billing and Workflow Nightmare
Most EHRs weren’t designed to handle multiple patients in a single session. This breaks documentation, complicates billing, and forces manual workarounds.
Telehealth Needs to Be Seamless, Not Siloed
Behavioral care often happens at home, in schools, or on the move. Switching between apps for telehealth disrupts care continuity—and hurts outcomes.
Billing Is Complex and Constantly Changing
Payer rules, DSM codes, and documentation requirements evolve fast. If your system doesn’t adapt with them, denials go up and revenue goes down.
The Human Cost of All This
The consequences of using generic or outdated systems in behavioral health aren’t just operational—they’re human.
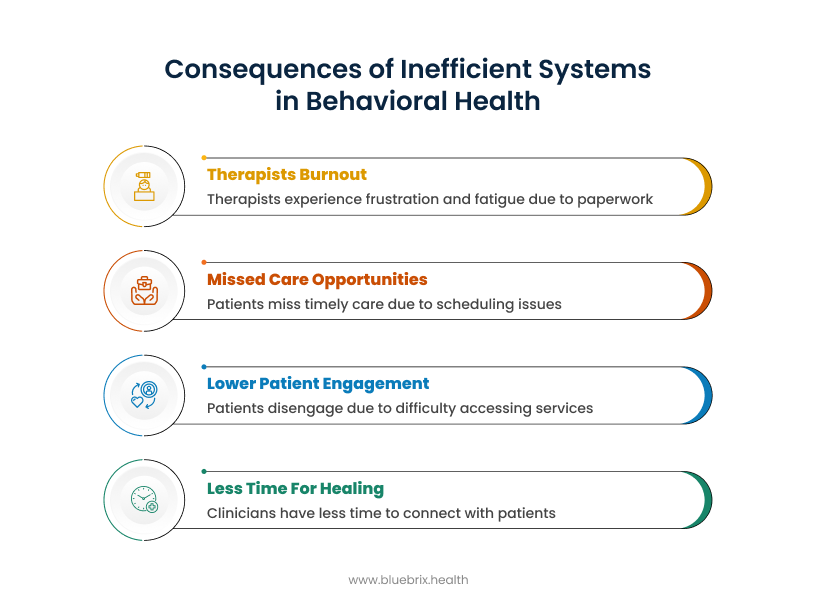
- Therapists burned out from paperwork.
When clinicians spend hours navigating clunky interfaces, retyping notes, or reconciling billing codes manually, it chips away at their ability to focus on what really matters: their clients. Over time, the emotional toll of balancing caregiving and clerical work leads to frustration, fatigue, and even turnover. - Missed care opportunities.
Every inefficient intake form, every double-booked calendar, every session that gets lost in the scheduling shuffle represents a person not receiving timely care. In behavioral health, delays don’t just inconvenience—they can worsen outcomes. - Lower patient engagement.
When patients can’t easily schedule appointments, access their care plans, or communicate with providers, they start to disengage. They miss sessions. They drop off the radar. And the continuity of care—the foundation of healing—is broken. - And less time spent actually helping people heal.
Perhaps the most tragic cost of all: clinicians lose valuable time they could spend connecting with patients. Time spent clicking, correcting, and chasing paperwork becomes time stolen from care.
At blueBriX, we don’t see these as isolated glitches—they’re systemic symptoms of tools that were never designed for behavioral health. And we’re here to change that.
The Way Forward: <i>Purpose-built For Behavioral Health </i>
That’s where blueBriX comes in—a platform designed from the ground up to reflect how behavioral health truly works in the real world.
We’re not just another digital solution trying to retrofit behavioral health into a medical template. We built blueBriX with behavioral health leaders, clinicians, and community programs in mind, deeply understanding the nuances of trauma-informed care, multi-modality services, complex billing, and the emotional dynamics of the work itself.
This isn’t about replacing paper with pixels. It’s about removing friction from every workflow, connecting clinical logic with operational efficiency, and giving providers more time to do what they do best: care.
With blueBriX, behavioral health organizations get:
- Technology that adapts to their programs—not the other way around
- Workflows designed for group therapy, community outreach, school-based care, and telehealth
- Patient experiences that feel personal, proactive, and empowering
- A platform that scales, secures, and strengthens operations behind the scenes
Because behavioral health deserves more than accommodation. It deserves technology that’s aligned, intentional, and built to elevate care.
The blueBriX Solution: How Laurel Life Reimagined Behavioral Health with the Right Technology
Laurel Life, a leading behavioral health organization in Pennsylvania and a division of the non-profit Folium, Inc., is deeply committed to providing high-quality, trauma-informed care across diverse communities. Their mission is rooted in a powerful belief: that transformation is possible for everyone. Through outpatient therapy, school-based programs, community-based services, and crisis intervention, Laurel Life helps individuals build resilience, foster healthy relationships, and navigate life’s challenges.
With operations spanning nine locations across Pennsylvania, Laurel Life has built a strong presence in both rural and urban communities—underscoring their focus on accessible, evidence-based care.
When Laurel Life set out to streamline care, reduce administrative complexity, and scale across multiple communities, they didn’t just want an EHR—they needed a behavioral health-first ecosystem. As a non-profit, their impact hinges not just on clinical excellence, but on operational efficiency. That’s why they continuously seek systems that align with their philosophy, adapt to their workflows, and maximize their ability to serve.
The Roadblocks to Growth and Resilience
Despite their clarity of mission, Laurel Life—like many behavioral health providers—faced growing pains rooted in everyday operational realities:
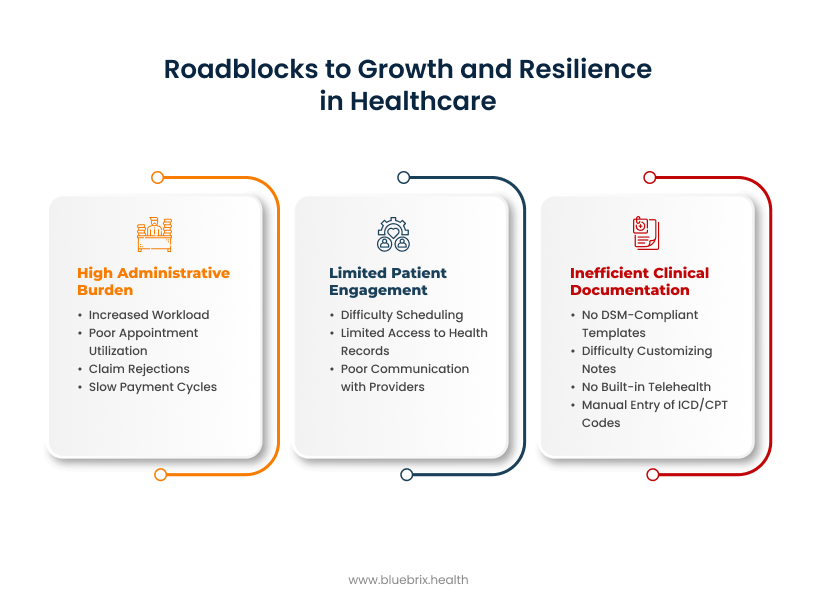
1. High Administrative Burden
Fragmented systems meant that scheduling, billing, and clinical documentation operated in silos. This led to:
- Increased workload on staff
- Poor appointment utilization
- Manual errors and rising operational costs
- A high number of claim rejections due to coding issues and missing information
- Slow payment cycles and inconsistent cash flow
2. Inefficient Clinical Documentation
Their existing tools failed to support trauma-informed, behavioral health-specific documentation:
- No DSM-compliant templates
- Difficulty customizing notes for different age groups and conditions
- No built-in telehealth, requiring clinicians to juggle multiple apps
- Manual entry of ICD/CPT codes, leading to billing errors and delays
3. Limited Patient Engagement
Patients struggled to:
- Schedule or reschedule appointments
- Access their health records
- Communicate with providers easily
This reduced satisfaction, increased no-shows, and created bottlenecks for the admin team.These weren’t isolated problems—they were part of a compounding system of inefficiencies. Disconnected documentation led to billing issues. Lack of engagement tools increased administrative calls. Admin overload reduced time for patient care. Every gap created ripple effects across care quality, revenue, and staff morale.
Laurel Life recognized that piecemeal solutions wouldn’t cut it. They needed a fully integrated platform—purpose-built for behavioral health—to break the cycle and better serve their mission. They chose blueBriX. And in doing so, they transformed the way their organization delivered care.
How blueBriX Empowered Laurel Life’s Mission
Laurel Life needed more than just an upgrade—they needed a behavioral health solution that truly understood their work. That’s where blueBriX came in. Purpose-built for behavioral health, blueBriX helped Laurel Life streamline operations, improve care delivery, and refocus their time and energy on what matters most: transforming lives.
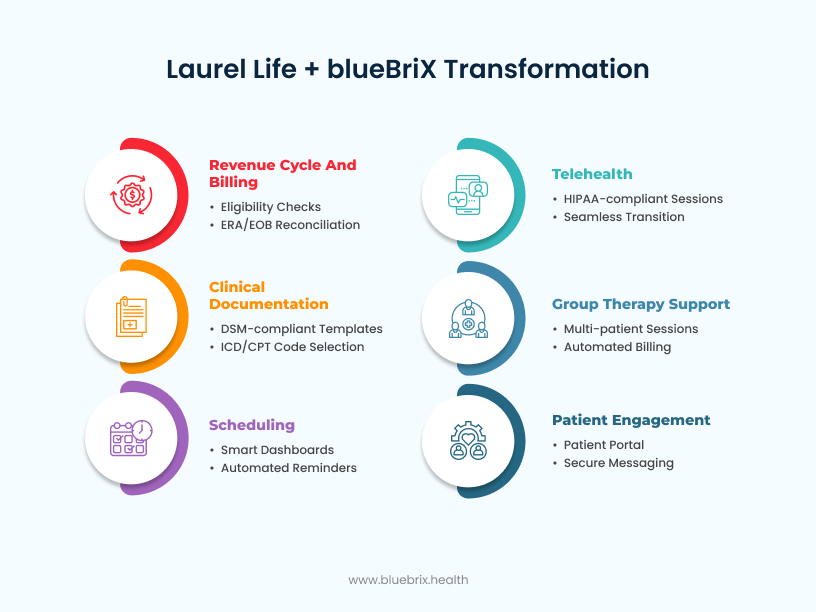 Here’s how that change unfolded:
Here’s how that change unfolded:
1. Clinical Documentation That Mirrors the Reality of Behavioral Health
Before blueBriX: Laurel Life’s therapists were spending too much time reworking generic templates and managing fragmented notes—slowing them down and risking claim denials.
With blueBriX:
- Clinicians now use DSM-compliant templates tailored to trauma-informed therapy.
- Documentation adjusts dynamically based on age and condition, helping Laurel Life’s team support youth, adults, and families with precision.
- Required Medicare and payer fields are flagged and enforced, reducing errors and missing data.
- ICD and CPT codes are embedded in note-taking—so providers no longer re-enter billing data post-session.
What changed:
Laurel Life reduced documentation time, increased clinical accuracy, and ensured that records not only told the full story of care—but also passed every audit.
2. Purpose-Built Support for Group Therapy
Before blueBriX: Group sessions required separate notes for each patient, duplicating effort and complicating billing—especially across school and community-based programs.
With blueBriX:
- Laurel Life implemented group therapy workflows that allowed one session to be shared across participants while enabling individualized tracking and outcomes.
- Billing was simplified, with automated linkage between attendance, session notes, and insurance claims.
- Everything—from scheduling to follow-ups—was managed in one place.
What changed:
Laurel Life now delivers more structured, scalable group sessions, with less admin overhead and more focus on impact.
3. Scheduling That Actually Works for Behavioral Health
Before blueBriX: Missed appointments, last-minute changes, and manual coordination were making it hard to optimize provider availability and meet demand.
With blueBriX:
- Laurel Life adopted smart scheduling dashboards to book, reschedule, and track appointments across providers and locations.
- An integrated intake form automatically matched patients to programs based on condition, location, and availability.
- Automated reminders via SMS/email significantly reduced no-shows.
What changed:
Appointment utilization improved by 20%, and staff gained back valuable time previously lost to coordination chaos.
4. Telehealth That Feels Seamless, Not Siloed
Before blueBriX: Laurel Life relied on third-party apps for telehealth, creating disjointed experiences and added complexity for providers and patients alike.
With blueBriX:
- Telehealth was natively integrated, with HIPAA compliance built in.
- Providers launched sessions directly from their dashboard, and patients accessed them via the portal—no switching apps or sending Zoom links.
- Secure chat and in-session documentation supported smooth, continuous care.
What changed:
Laurel Life could expand access to care across geographies, reduce IT complexity, and improve follow-through for virtual visits.
5. Billing and Revenue Integrity That Drives Growth
Before blueBriX: Laurel Life was facing high claim rejection rates, delayed payments, and manual processes that left revenue on the table.
With blueBriX:
- Real-time eligibility verification helped prevent issues before services were rendered.
- Claim scrubbing flagged errors pre-submission.
- ERA/EOB reconciliation automated follow-ups.
- Payer contract logic ensured every service was reimbursed accurately.
What changed:
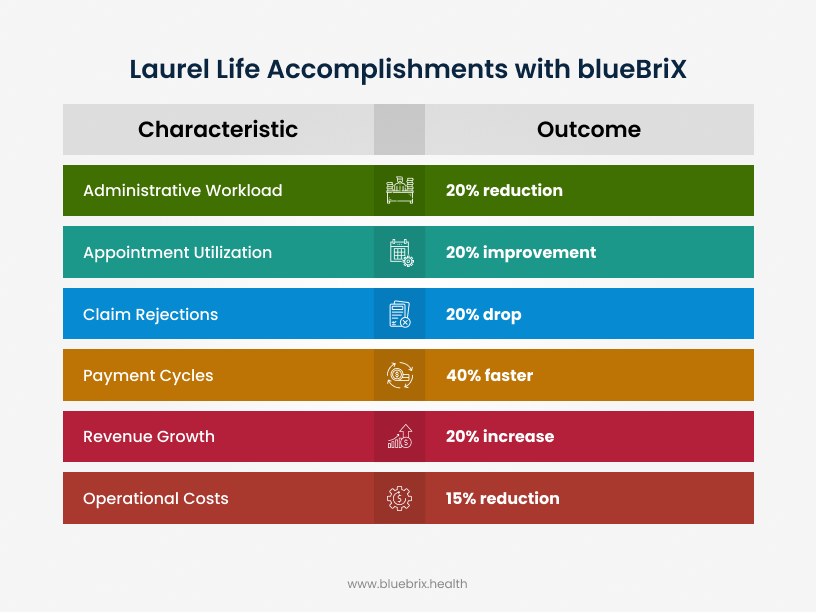
- 20% decrease in claim rejections
- 40% faster payment cycles
- 20% revenue growth driven by clean, accurate billing
Laurel Life turned billing from a bottleneck into a growth engine.
6. Engaging Patients with Simplicity and Transparency
Before blueBriX: Patients often missed appointments, struggled to engage between sessions, and had limited visibility into their own care journey.
With blueBriX:
- A 24/7 patient portal now offers access to records, care plans, and secure messaging.
- Online appointment scheduling and cancellation gave patients control and reduced admin calls.
- Automated SMS/email reminders improved attendance.
- Future plans include a custom patient engagement app for even deeper community connection.
What changed:
Patient participation and satisfaction increased, while Laurel Life’s team spent less time chasing confirmations and more time delivering care.
Outcomes That Speak for Themselves
At Laurel Life, the implementation of blueBriX led to remarkable, quantifiable improvements across key operational areas. We saw a 20% reduction in administrative workload, a 20% improvement in appointment utilization, and a 20% drop in claim rejections. Furthermore, payment cycles accelerated by 40%, contributing to a 20% increase in revenue growth and a 15% reduction in operational costs. Beyond these impressive metrics, blueBriX empowered Laurel Life’s team to refocus on their core mission: delivering compassionate, evidence-based care that genuinely transforms lives.