
Spravato (esketamine) therapy has been a breakthrough for patients living with treatment-resistant depression (TRD); but for behavioral health practices, it’s also become a billing and compliance minefield.
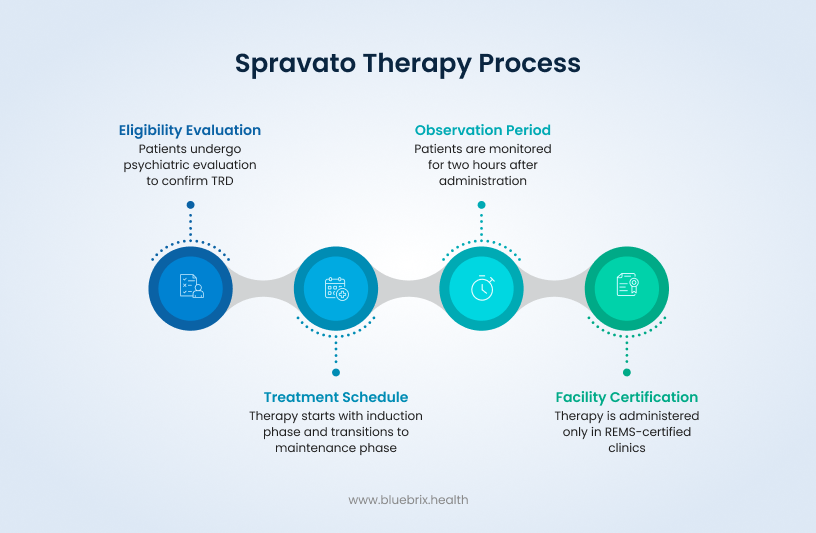
If you’ve ever tried to process a Spravato claim, you already know it’s nothing like billing for a standard antidepressant. Every dose must be administered under medical supervision in a REMS-certified clinic, tracked in real time, and billed with precision across medical and pharmacy benefit lines that rarely play nice together.
And here’s the kicker: even a minor coding misstep or missing documentation can lead to denials, payment delays, and serious revenue leakage.
That’s why Spravato isn’t just another medication. It’s a clinical and operational ecosystem that requires a new kind of behavioral health RCM precision.
In this blog, we’ll unpack how Spravato’s unique clinical and billing model works, where most workflows break down, and how behavioral health organizations can future-proof reimbursement using compliant, audit-ready processes.
Whether you’re a psychiatrist running an independent clinic or an RCM director managing multiple behavioral health locations, this guide will show you how to ensure your Spravato billing and coding get paid right the first time. A better option to consider would be to partner with blueBriX for outsourced RCM services to ensure accuracy, compliance, and faster reimbursements without adding to your administrative burden.
Before we dig into billing mechanics, let’s quickly cover what makes Spravato clinically unique, because that’s what creates the billing complexity we’re about to solve.
What Makes Spravato (Esketamine) Therapy Different and Why Billing It Is Complex
Spravato is an FDA-approved nasal spray used specifically for adults with treatment-resistant depression (TRD) and is administered in a REMS-certified facility under direct clinical supervision. That one distinction changes everything; clinically, operationally, and financially.
This means your RCM process has to track every moving part; procurement, coding, pre-authorization, and payer coordination with zero room for error.
And that’s exactly where most billing teams start to feel the pressure. Because once you move past administration, the next big challenge is understanding how Spravato gets paid for and who’s paying for what.
Understanding those clinical constraints clarifies why two procurement models exist, and why your reimbursement approach must adapt accordingly.
Spravato Procurement and Payment Models: How Each Impacts Reimbursement
When it comes to Spravato reimbursement, there are only two ways to play it and both require airtight workflows:
- Buy-and-Bill Model: Your clinic buys Spravato directly from a distributor, administers it onsite, and bills the payer for both the drug and clinical services (administration + observation).
- Assignment of Benefits Model: A specialty pharmacy supplies the medication, while your clinic bills only for administration and observation.
Either way, you’re responsible for documenting the who, what, when, and how of every single session and aligning it with payer-specific rules that often differ by plan or phase of treatment.
This is where operational discipline meets coding precision. Because once you’ve figured out your payment model, the next barrier to clean claims isn’t about process, it’s about code accuracy.
Understanding Spravato’s Dual-Benefit Dilemma
Some payers classify Spravato under the medical benefit. Others treat it as a pharmacy benefit. A few do both, which is every billing manager’s nightmare. When the therapy straddles two benefit types, your RCM workflow has to split and synchronize claims across systems that were never meant to talk to each other.
Picture this: Dr. Patel’s behavioral health clinic just completed a flawless Spravato session. The documentation is perfect, the patient responded well and then comes the question no one wants to ask: Which benefit do we bill under?
That’s the dual-benefit dilemma.
If Spravato falls under the medical benefit, your clinic is responsible for pre-authorization, benefit verification, and one of two procurement paths; buy-and-bill (where you purchase and bill for the drug) or assignment of benefits (where a specialty pharmacy supplies it).
If it’s covered under the pharmacy benefit, a specialty pharmacy handles the drug billing, while your team must submit a separate medical claim for administration and observation services.
The problem? Those two workflows almost never align. Data gets siloed, claim submission timing goes off, and payment reconciliation turns into a guessing game. The result: denials, underpayments, and revenue leakage that can easily be avoided with tighter integration.
Why Traditional Billing Systems Fail with Spravato Claims
Here’s the truth: most billing systems simply weren’t built for hybrid therapies like Spravato. They’re designed for speed and volume, not for complex, dual-benefit workflows that demand meticulous synchronization.
Traditional systems fail because of five main weaknesses:

- Limited System Design – Pharmacy billing software assumes self-administered drugs, while medical billing tools assume the encounter ends when the visit does. Spravato doesn’t fit either model.
- Documentation Gaps – The therapy requires detailed pre-authorization records, dosage tracking, and two-hour observation logs that standard drug workflows never capture.
- Lack of Integration – Pharmacy and medical billing systems don’t communicate, leading to fragmented claims and mismatched data.
- Coding Complexity – Spravato requires multiple CPT and HCPCS codes combined into one coherent claim. Many workflows can’t handle that.
- Procurement Conflicts – Some payers demand buy-and-bill while others require specialty pharmacy procurement. The lack of standardization creates workflow chaos.
Essentially, the old RCM playbook doesn’t work here. Spravato’s clinical and financial intersections require a next-generation billing framework; one that can handle nuance and compliance without sacrificing speed.
Common Spravato Billing Challenges and How to Avoid Claim Denials
Let’s start with the internal roadblocks that drag down Spravato reimbursement.
Complex Prior Authorizations: Every payer wants something different — diagnosis proof, treatment history, dosing schedules, letters of medical necessity, and REMS logs. Miss one piece, and your authorization request is either delayed or denied.
Coding Accuracy Problems: Spravato claims fail when the codes don’t line up. The most common culprits?
- Wrong HCPCS code (S0013, G2082, G2083).
- Missing prolonged service codes for observation.
- Failing to link all codes under the same diagnosis.
Dosing Frequency Errors: Payers are strict about FDA-approved schedules — twice weekly during induction, less frequent during maintenance. Bill for an off-schedule visit, and the claim gets hit with “not medically necessary.”
Documentation Gaps: A missing progress note, incomplete REMS log, or absent LMN (Letter of Medical Necessity) is enough to trigger denials or even post-payment clawbacks.
Split Billing Confusion: When one patient’s medication is covered under pharmacy benefits and administration under medical benefits, clinics often submit fragmented or duplicate claims. This is one of the top drivers of Spravato-related denials.
Inefficient Denial Management: Even when claims are recoverable, many clinics lack structured follow-up workflows. That means denials sit unresolved for weeks, or worse — they’re written off as bad debt.
If this list feels familiar, you’re not alone. These pain points plague behavioral health organizations across the country, but they’re also completely fixable with the right RCM infrastructure.
Common Reasons for Spravato Claim Denials
Here’s what payers flag most often and how to read between the lines:
- No Prior Authorization — Automatic denial. Period.
- Incorrect or Missing Codes — Usually tied to prolonged observation codes or mismatched CPT/ICD pairings.
- Insufficient Medical Necessity Documentation — Missing evidence of two failed antidepressants or incomplete LMN.
- Non-Adherence to Dosing Schedule — Billing outside the FDA-approved induction or maintenance plan.
- Eligibility or Coverage Gaps — Patient plan doesn’t cover the full course or has expired authorization.
- Administrative Errors — Missing NPI, incorrect date of service, or mismatched payer ID — the small mistakes that cost big.
The harsh reality? Most Spravato denials are self-inflicted. They stem from process breakdowns that can be prevented with automation, integration, and real-time verification.
The Hidden Operational Costs of Outdated Billing Workflows
When your billing systems can’t keep up, the fallout hits fast and hard. Behavioral health clinics face operational slowdowns, compliance risk, and serious cash flow issues.
Here’s what that looks like on the ground:
- Teams juggling multi-channel claim coordination between pharmacy, medical, and payer systems.
- Authorization overload, with every session requiring detailed documentation and REMS proof.
- Drug access delays, caused by confusion over whether to use medical or pharmacy benefits.
- Prolonged reimbursement cycles, with payments stuck in limbo due to mismatched data.
- Higher denial rates, especially when codes or payer rules aren’t aligned.
The cumulative impact? Staff burnout, slower scheduling, and financial unpredictability all of which drain operational efficiency.
How to Optimize Revenue Integrity and Improve First-Pass Claim Success
Let’s break down the three high-impact strategies driving that success:
1. Build Strong Charge Capture and Verification Workflows
Every Spravato session has multiple billable components: the drug, the administration, the E/M visit, and the prolonged observation. Miss even one, and your clinic leaves money on the table.
That’s why charge capture is your first line of defense in protecting revenue.
High-performing behavioral health clinics use multi-layer verification where clinical, coding, and billing teams each confirm accuracy before submission.
Here’s how that works in practice:
- Clinical staff verify the dosage, administration times, and patient observation duration.
- The billing team validates codes and payer-specific coverage rules.
- The RCM system cross-references the documentation to ensure every element from drug units to modifiers is accounted for.
When your workflows are structured this way, nothing slips through. You capture every charge, verify every detail, and submit claims that payers can’t easily reject.
That’s how you move from chasing payments to maintaining predictable, stable cash flow.
2. Automate Eligibility, Benefit Verification, and Prior Authorization Tracking
If manual verification feels like a full-time job, that’s because it is the automation can do faster and more accurately.
Spravato billing is a moving target. Different payers treat it differently; authorization timelines vary; and benefit renewals expire mid-treatment if no one’s watching. That’s where automation flips the script.
Leading RCM service providers will help you integrate real-time eligibility checks, payer-specific rule mapping, and automated prior authorization tracking directly into the billing workflow.
What does that mean for your clinic?
- You know instantly whether a patient’s coverage falls under medical or pharmacy benefits.
- Prior authorization requests go out electronically, with all required attachments pre-populated.
- The system flags expiring approvals and sends renewal reminders before treatment interruptions occur.
It’s how modern RCM teams stay proactive, not reactive.
3. Leverage Real-Time Denial Analytics
You can’t fix what you can’t see and that’s why denial analytics has become the backbone of high-performing RCM teams.
Spravato billing denials aren’t random. They follow patterns: mismatched codes, documentation gaps, and missing authorizations. When you track and categorize them at scale, those patterns reveal your weakest links.
Forward-thinking clinics use real-time denial dashboards to monitor these trends; identifying root causes and closing workflow gaps before they repeat.
Think of it as feedback intelligence. Every denial is a data point that, if analyzed, improves the system.
Here’s how the best clinics use it:
- They review top denial reasons weekly (authorization, documentation, coding).
- They run root cause analyses to identify which process failed.
- They update templates, training, and automation rules based on findings.
Over time, that loop drives measurable improvement. The result? Fewer resubmissions, faster payments, and a first-pass rate that steadily climbs toward perfection.
And that’s exactly where blueBriX stands out as a behavioral health RCM service provider; giving clinics real-time insights into denial drivers, payer trends, and staff performance.
Spravato Coding Guide: Getting Drug, Administration, and Observation Codes Right
Coding Spravato is half the battle. Every treatment session combines three distinct billable elements: the drug, the administration, and the extended observation. Miss one, misalign them, or use the wrong code, and your claim is dead on arrival.
Let’s break it down in plain terms and see how a little precision on the front end can save weeks of reimbursement delays on the back end.
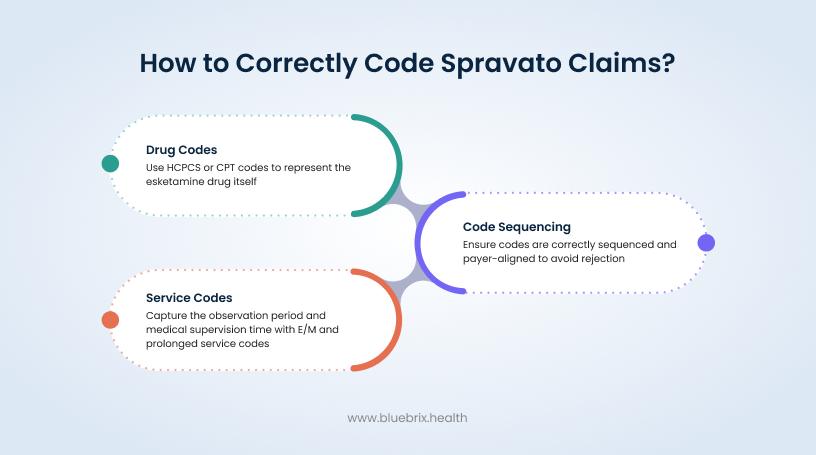
Drug Coding (HCPCS): Getting the Foundation Right
Spravato’s coding starts with the HCPCS drug codes. Unlike standard antidepressants, this isn’t a one-size-fits-all scenario. You need to report the exact milligrams administered, tied to the correct payer code.
Here’s the lineup:
- S0013 — Esketamine nasal spray, 1 mg. Commonly used by commercial payers. Your billed units must match the exact dose. For instance, a 56 mg dose equals 56 units of S0013.
- G2082 — Used for the 56 mg dose under Medicare or certain commercial payers.
- G2083 — Used for the 84 mg dose under Medicare or similar plans.
- J3490 — Unclassified drugs. This is the fallback when payers haven’t yet adopted specific codes. But be warned, you’ll need clear documentation of the drug, dosage, and purpose to justify its use.
In some payer setups, G2082 and G2083 include both the drug and administration service, especially under buy-and-bill arrangements. Always confirm your payer’s setup before billing, that single step can mean the difference between clean payment and back-and-forth appeals.
Administration and Observation Codes (CPT/HCPCS): Capturing the Full Service
Spravato isn’t something you hand to a patient and bill once. Each treatment involves active administration followed by mandatory clinical observation. That’s two separate categories of CPT coding that must work together.
Let’s start with administration:
- You’ll typically use Evaluation & Management (E/M) codes 99202–99215 for office or outpatient services. The exact level depends on either the complexity of decision-making or the total encounter time.
For the prolonged observation phase, which is what really separates Spravato from routine care, use:
- 99415, 99416, or 99417 — for extended clinical supervision or patient contact that exceeds normal E/M limits.
- G2212 — the Medicare equivalent of 99417, billed in 15-minute increments once you surpass the highest E/M threshold.
The rule is simple: if the patient sits in your clinic for two hours post-administration, you need to capture every minute that qualifies as prolonged service time backed by exact start and stop times in your documentation.
Here’s a quick example:
Example: Dr. Nguyen administers an 84 mg dose of Spravato, then monitors the patient for two hours. Her coder bills G2083 for the drug, an E/M code for the encounter, and multiple units of 99417 for the prolonged observation period. The documentation includes start and end times, vitals, and monitoring notes — resulting in a clean, fully justified claim.
That’s how you prevent denials before they even reach the payer queue.
Modifiers and Units: Fine-Tuning for Accuracy
Here’s where many clinics stumble — the details. Spravato billing is a precision game, and units and modifiers are your calibration tools.
- Units: The units you bill must directly match the dosage administered. For instance, 56 mg equals 56 units of S0013.
- Modifiers: If you perform distinct procedures or repeat services on the same day, you’ll likely need modifiers such as -59 (distinct procedural service) or –76 (repeat procedure by the same provider).
- Time Documentation: Every session should include start and end times for both administration and observation. This validates the level of service and justifies prolonged time-based codes.
Why Coding Precision Matters for Spravato Billing Compliance and Reimbursement
A single code mismatch can trigger an audit, delay cash flow, or lead to underpayment that goes unnoticed for months.
Precision matters because payers expect complete synchronization between three things:
- The drug codes (HCPCS).
- The service and observation codes (CPT/HCPCS).
- The supporting documentation — dosing logs, time records, and REMS notes.
A clean claim tells a coherent story: the patient qualified for treatment, received it under REMS conditions, was monitored per FDA requirements, and every step was properly documented.
Payers don’t reject Spravato claims because they dislike the therapy. They reject them because the paperwork doesn’t connect the dots.
That’s why leading behavioral health RCM service providers like blueBriX use a combination of expert oversight and intelligent automation to validate time, dosage, and payer-specific coding rules before a claim ever leaves the queue.
Documentation That Drives Reimbursement: How to Build an Audit-Proof Record
Every payer, every auditor, every post-payment review starts with the same question: Can you prove medical necessity? And here’s the truth — Spravato reimbursement lives or dies by your documentation discipline.
It’s not just about filling in forms or ticking boxes. It’s about showing, step by step, that your patient needed the therapy, that it was administered exactly per FDA standards, and that every minute of observation and care was medically justified.
Think of documentation as your clinic’s financial safety net. The tighter you weave it, the safer your revenue cycle becomes.
1. Medical Necessity Documentation for Authorization and Claims
To get paid and stay paid you must document medical necessity like a litigator preparing evidence.
Every Spravato claim should prove three things:
- The patient met the FDA and payer criteria for treatment-resistant depression (TRD).
- The provider and facility were qualified and REMS-certified.
- The treatment was clinically justified and safely administered.
That means your records need to include:
- Confirmed Diagnosis: The patient’s chart should clearly state TRD or Major Depressive Disorder with acute suicidal ideation, backed by standardized scales like PHQ-9 or MADRS.
- Treatment History: Detailed notes on failed antidepressants — names, doses, treatment durations, and clinical outcomes. Two failed trials minimum, per payer policy.
- Provider and Facility Credentials: Proof that both are REMS-certified and authorized to administer Spravato.
- Treatment Plan: Exact dosing schedules for induction and maintenance phases.
- Observation Records: Vitals, reactions, and supervision notes logged during the two-hour post-dose window.
- Letter of Medical Necessity (LMN): A formal narrative summarizing diagnosis, failed treatments, rationale for Spravato, and clinical goals — ideally signed by the supervising psychiatrist.
2. Charting Protocols: Administration, Observation, and Adverse Events
Spravato charting isn’t just a clinical formality, it’s an FDA requirement and a financial safeguard rolled into one.
Every session should have real-time charting that captures exactly what happened, when, and how it was managed.
Here’s what that looks like in practice:
- Administration Notes: Record when the drug was administered, the dosage (in milligrams), the method (nasal spray), and whether the patient self-administered or required staff support.
- Observation Timeline: Log precise start and stop times for the two-hour monitoring period, including vitals and behavioral assessments at regular intervals.
- Adverse Event Tracking: If dissociation, sedation, or blood pressure spikes occur, document the onset, severity, interventions, and patient outcome.
- Follow-Up Summary: Include clinician observations and patient-reported feedback post-session.
This level of granularity does three things:
- Keeps your clinic REMS-compliant.
- Protects your team during payer audits.
- Validates every billed minute of E/M and prolonged service codes.
Let’s put it in context:
Example: Dr. Alvarez’s clinic noticed denials for prolonged service codes. After reviewing documentation, they realized nurses were charting observation start times but not end times. By correcting that, adding vitals at 30-minute intervals, and syncing logs with the billing team, denial rates dropped by 40% in one quarter.
That’s how documentation turns from an afterthought into a measurable revenue driver.
3. Linking ICD-10 Diagnoses to CPT/HCPCS Codes for Seamless Claims
Clean documentation alone isn’t enough. Your codes must tell the same story your chart does.
Every Spravato claim needs precise alignment between ICD-10 diagnosis codes (what was treated) and CPT/HCPCS procedure codes (what was done).
Here’s what that alignment looks like:
- Use the Right ICD-10 Codes:
- F32.2 — Major depressive disorder, single episode, severe
- F33.2 — Major depressive disorder, recurrent, severe
- F32.3 or F33.3 — If psychotic features are present
- Link Consistently: The same diagnosis should appear on every claim line — for the drug (HCPCS), administration (CPT), and observation (prolonged service codes).
- Follow Payer Rules: Some payers limit which ICD-10 codes qualify for Spravato coverage. Verify this before submission.
- Sequence Correctly: Always list the primary diagnosis first, matching the date of service and CPT/HCPCS details.
- Align Documentation: Each diagnosis must be supported by clinical notes, validated assessment scores, and prior treatment history.
When coding and documentation speak the same language, payers can’t argue medical necessity and that’s how you achieve true first-pass claim success.
As behavioral health RCM service providers like blueBriX have shown, integrating automation and expert oversight to link diagnoses, CPT codes, and REMS records removes guesswork entirely — ensuring every claim goes out clean and audit-proof.
In short, documentation is your financial armor. It justifies the treatment, proves compliance, and backs every code you submit.
Even when the clinical side of Spravato® (esketamine) therapy runs like clockwork, many behavioral health clinics still watch their reimbursements crumble under the weight of RCM errors.
Why? Because Spravato doesn’t play by the usual billing rules.
Why a Specialized RCM Service Provider Is Essential for Spravato Billing
When a therapy blurs the lines between pharmacy and medical benefits, only a specialized behavioral health RCM model can keep revenue flowing smoothly.
The most successful clinics are already moving toward smarter systems. Those are the ones that
- Run real-time benefit verification to detect which channel applies.
- Automate cross-claim coordination between pharmacy and medical workflows.
- Handle pre-authorization management without manual back-and-forth.
- Maintain audit-ready documentation that passes payer scrutiny on the first submission.
That’s the kind of automation-driven accuracy provided by RCM service providers like blueBriX, connecting compliance, coding, and cash flow in one synchronized ecosystem.
Because when your RCM backbone is built for hybrid models like Spravato, billing won’t be a battle. It becomes a predictable, scalable process freeing your clinical team to focus on care, not claim reconciliation.
Strategies to Protect Financial Health in Spravato Billing and Reimbursement
You can’t eliminate payer complexity, but you can outsmart it. The most financially stable behavioral health clinics have something in common, that is proactive RCM workflows that close gaps before they open.
Here’s how they do it:
Standardize Documentation: Build a Spravato-specific checklist for every patient: diagnosis confirmation, treatment history, dosing schedule, LMN, and REMS logs. No treatment proceeds until it’s complete.
Train and Audit Coders: Continuous education is non-negotiable. Your billing team should understand Spravato’s unique coding hierarchy and your internal audits should catch inconsistencies before payers do.
Automate Administrative Workflows: Use technology to handle the tedious stuff: prior authorization tracking, benefit verification, and payer rule updates. Automation eliminates the “human lag” that causes preventable denials.
Create a Denial Recovery System: Don’t just track denials categorize, analyze, and act on them. Use dashboards to identify recurring issues and implement fixes immediately.
Strengthen Payer and Pharmacy Collaboration: Keep open communication channels between your RCM team, payers, and specialty pharmacies. Shared visibility prevents duplicate or misaligned billing.
This is where blueBriX changes the game. As an RCM service provider, they bring together payer rule mapping, automated pre-authorization workflows, and denial analytics in one unified system giving clinics the ability to resolve, prevent, and even predict denials before they impact revenue.
When it comes to Spravato, “good enough” won’t cut it. Each claim represents hundreds of dollars in drug costs and hours of clinical care — and one small mistake can flip that from profit to loss in seconds.
That’s why the most successful behavioral health clinics treat revenue integrity as a strategic discipline, not a back-office function. Their goal? Check it out in what comes next.
Key Takeaways: Building a Resilient Spravato Billing and Coding Workflow
If your workflows can handle Spravato billing with accuracy and speed, they can handle anything.
The clinics that are winning in this space have stopped viewing Spravato billing as a “problem to solve” and started seeing it as a blueprint for financial resilience.
Here’s what that looks like in practice.
Each session can bring in $1,300 to $1,600 in reimbursement, with roughly $875 of that tied to the drug alone. But that revenue potential disappears the moment your claim gets denied or underpaid.
Getting it right the first time means:
- Maximized Revenue Capture — Every drug dose, observation period, and E/M service is billed and reimbursed correctly.
- Accelerated Cash Flow — Clean claims clear faster, boosting cash stability and reducing AR aging.
- Reduced Audit Exposure — Meticulous documentation and accurate coding minimize payer scrutiny.
When your clinic runs on a first-pass success model, your bottom line reflects it.
Why Partnering with an RCM Service Provider Future-Proofs Your Spravato Operations
Spravato has exposed a simple truth about behavioral health billing: traditional systems can’t keep up. Between dual-benefit workflows, payer variability, and REMS documentation, the process demands specialized expertise and intelligent automation.
That’s where forward-looking clinics are finding their edge through strategic RCM partnerships.
Partnering with a specialized RCM service provider like blueBriX gives behavioral health organizations a significant operational advantage:
- Smarter RCM Automation: Seamless integration across EHRs, payers, and pharmacies.
- Compliance Assurance: Continuous alignment with FDA REMS and evolving payer requirements.
- End-to-End Visibility: From patient eligibility to payment posting — every detail tracked, validated, and auditable.
And if you’re ready to stop reacting and start scaling, then partner with the right technology. blueBriX helps behavioral health organizations master the art of first-pass success through unified RCM automation that bridges clinical care, compliance, and cash flow. Book a DEMO now!