In healthcare, knowing a patient’s risk is paramount. But what if that crucial information is always a step behind, painting yesterday’s picture when today’s intervention is desperately needed? This first part of our series dives deep into the hidden costs of delayed detection, exploring why static risk scores are failing our patients and hindering true preventive care. Discover how blueBriX is changing the game with real-time, dynamic insights, transforming how risks are identified and setting the stage for truly proactive patient management.
We’ve all seen it! Mrs. Davies, a vibrant 72-year-old, was discharged after a successful hip replacement. Her initial “risk score” for readmission, generated upon discharge, was reassuringly low. But over the next 48 hours, subtle shifts began to occur: a slight increase in her temperature, a new, almost unnoticeable tremor in her hand, a brief mention of feeling “a bit more tired than usual” during a routine follow-up call. Individually, these might seem minor. Collectively, they paint a different picture. Yet, her official risk score, tied to a system that updates only once every 24 hours, still flags her as low-to-moderate. The new, critical pieces of her evolving health puzzle haven’t yet been processed into an updated score. By the time the system catches up, valuable hours, even a full day, have been lost, and her condition has escalated from a minor concern to a potential crisis. This is the treacherous reality of clinical and operational delays stemming from lagging or static risk data.
The problem isn’t a lack of data; it’s a critical deficit in timely, integrated data. In healthcare, every second counts, and outdated information isn’t just inefficient—it’s dangerous. Traditional risk assessments often rely on batch processing, where vital patient information is collected, compiled, and analyzed at set, often infrequent, intervals – daily, weekly, or even monthly. Imagine a doctor trying to make a life-saving diagnosis based solely on a patient’s lab results from yesterday morning, while new, critical symptoms developed just an hour ago haven’t even been noted in the chart.
Healthcare professionals find themselves in precisely this dilemma, striving to predict dynamic patient prognosis with static snapshots from the past. They’re forced to make critical, often life-altering decisions based on yesterday’s news, not today’s rapidly evolving reality. This inherent lag creates invisible, yet deeply dangerous, cracks in the system, through which patients like Mrs. Davies can, and often do, fall. This systemic inability to adapt to real-time changes severely hinders any meaningful efforts at preventive care and undermines the very foundation of value-based care models, where proactive, timely interventions are paramount.
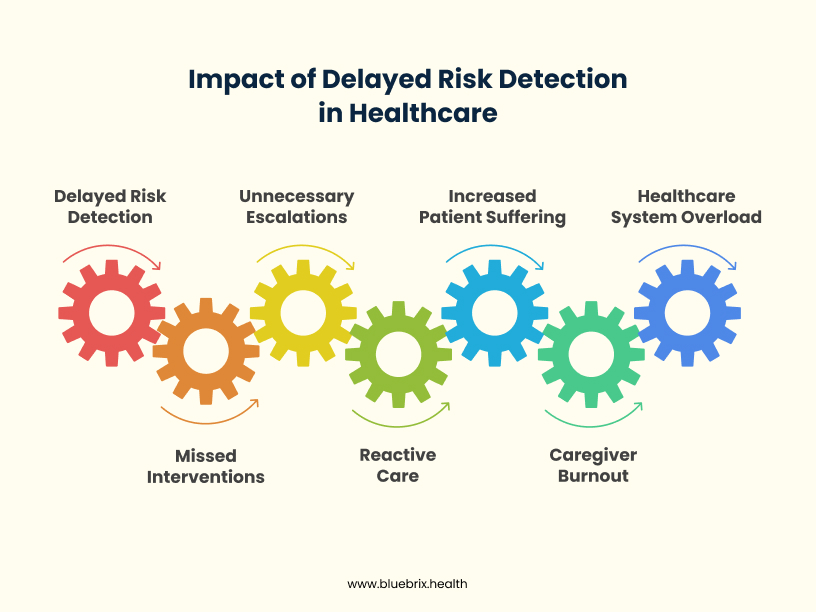
When risk scores come too late, the ripples are felt throughout the entire care continuum, creating a cascading effect of inefficiency and compromised care. We see missed interventions, like Mrs. Davies’s early signs of a post-operative complication being overlooked until it’s a full-blown crisis requiring re-hospitalization. This leads directly to unnecessary escalations, forcing patients into higher levels of care, extending hospital stays, and driving up costs that could have been avoided. This directly sabotages efforts for reduced readmissions. Clinicians, already under immense pressure, are trapped in a cycle of reactive care, constantly responding to emergencies rather than proactively preventing them. They feel the frustration of knowing, intuitively, that something is wrong, but lacking the real-time, data-driven support to justify immediate action. The hidden cost isn’t just financial, measured in inflated bills and wasted resources; it’s profoundly human, measured in increased patient suffering, caregiver burnout, and a healthcare system always playing catch-up, always a step behind.
But then, the turning point. We introduce how blueBriX flips this script by delivering real-time risk scoring. Imagine a system where every piece of new information – a nurse’s observation logged at the bedside, a lab result uploaded seconds after processing, a patient’s self-reported symptom captured via a mobile app, even subtle shifts in historical data points – is instantly fed into an intelligent engine. At the core of this dynamic data capture is our intuitive custom form builder. With blueBriX’s low-code no-code platform, providers can effortlessly design and deploy highly adaptive forms to gather rich, granular data – everything from social determinants of health to detailed lifestyle assessments, directly from patients or during clinical encounters. These forms aren’t static surveys; they intelligently adapt based on previous responses, ensuring the right information is captured efficiently and comprehensively, without a single line of code.
Our powerful rule engines aren’t just running calculations once a day; they’re constantly listening, evaluating, correlating, and learning from this incoming stream of data, including what’s captured through our dynamic forms. They’re like a vigilant sentinel, connecting the dots as they appear. If Mrs. Davies’s temperature ticks up by a single degree, if she reports new pain via a custom form on her tablet, or if her activity level decreases, the system instantly processes these inputs, updating her risk profile in milliseconds. It’s like upgrading from that day-old map to a live GPS system, constantly updating with traffic conditions, road closures, and even unexpected hazards, providing a dynamic, evolving picture of the road ahead. This dynamic risk scoring profoundly supports preventive care by identifying individuals at risk before they fully manifest acute conditions or require readmission, thus aligning perfectly with value-based care goals. The underlying configurable EHR makes it simple to integrate these real-time risk assessments into any existing clinical workflow, adapting to unique organizational needs without complex IT projects.
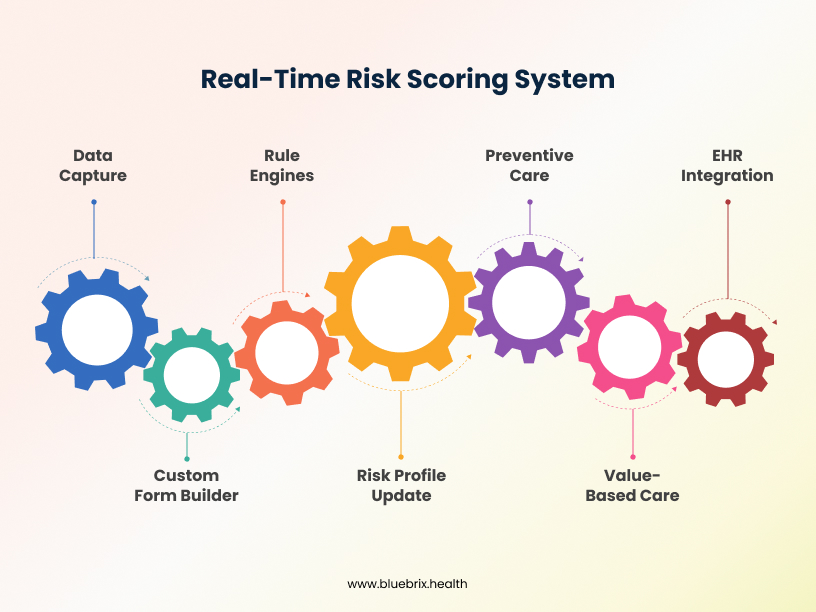
This means user input and assessments, powered by our flexible Form Builder, aren’t just static data points for later review; they dynamically update patient profiles, ensuring that every risk score is as fresh as today’s news – in fact, as fresh as this very moment. This isn’t just a number on a chart; it’s a living, breathing indicator that empowers proactive care and drives towards reduced readmissions. We’ll show how blueBriX identifies subtle shifts, not just obvious crises, allowing care teams to intervene earlier, often before a patient’s condition significantly worsens. Imagine a nurse receiving an alert about Mrs. Davies’s elevated temperature as it happens, prompting an immediate check-in, averting a readmission. This transition from retrospective analysis to predictive foresight fundamentally changes the rhythm of care delivery.
We’ve now seen how blueBriX transforms static data into a living, evolving understanding of patient risk, enabling truly proactive care. But identifying risk is only half the battle; the real challenge begins when that critical information demands immediate, intelligent action – a challenge we’ll tackle in the next part: Triage.
Next Steps: Ready to See Risk in Real-Time?
The journey to proactive care begins with truly understanding risk. Stay tuned for Part 2 of our series, where we’ll delve into “The Triage Trap” and how intelligent automation ensures timely action.
Want to explore how real-time risk insights can specifically transform your organization’s value-based care initiatives and help achieve remarkable reductions in readmissions? Connect with blueBriX today for a personalized discussion.