
You’ve identified a high-risk patient – now what? Our previous discussion highlighted the power of real-time risk identification. But in this second part of our series, we confront “The Triage Trap,” where the critical handoff from risk identification to action often becomes a chaotic bottleneck. We’ll explore how manual prioritization leads to staff burnout, inconsistent care, and preventable hospitalizations. Learn how blueBriX’s intelligent, automated triage, powered by actionable dashboards, transforms this challenge, ensuring timely and precise care coordination for every patient.
When we have accurate, real-time risk scores, how do we ensure the right people get the right care, right now? This is where many organizations fall into “The Triage Trap.” The moment a high-risk patient is identified, a new kind of chaos often ensues, transforming a moment of clarity into a quagmire of manual effort.
Imagine a care coordinator overwhelmed by a flood of alerts, trying to manually route a high-risk patient like Mr. Rodriguez, whose complex diabetes needs immediate follow-up. This often involves sifting through sprawling spreadsheets, jammed inboxes, and relying on intuition to determine which team has the capacity and expertise. This messy, fragmented approach makes preventive care coordination nearly impossible.
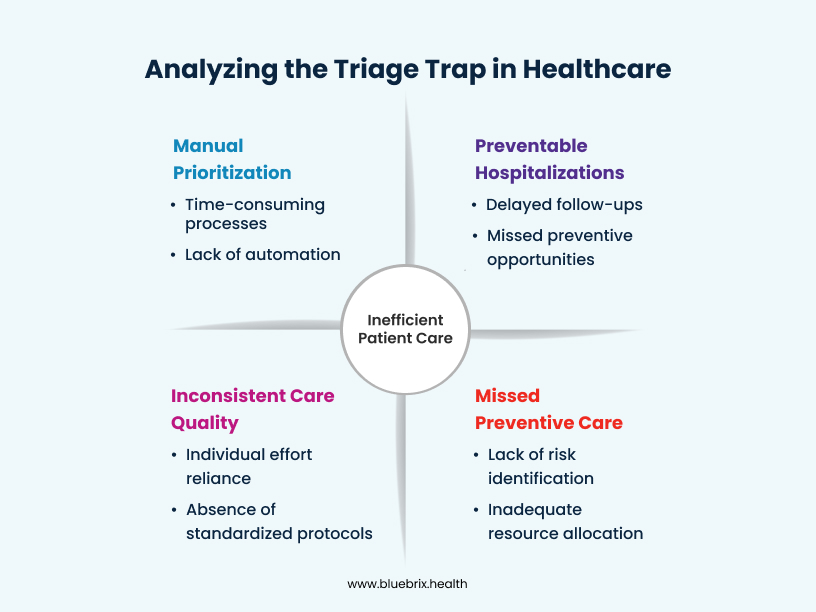
The consequences are severe. Care teams experience severe burnout from the constant pressure of manual prioritization and the agonizing fear of missing a critical patient. This leads to inconsistent care quality, as patient routing depends on individual effort rather than standardized processes, directly impacting value-based care. Most tragically, this often results in preventable hospitalizations and missed opportunities for preventive care. Mr. Rodriguez might fall through the cracks, his vital follow-up delayed, leading to a preventable emergency room visit that costs both the system and the patient dearly. It’s a system struggling under its own weight, desperately needing a smarter, more reliable way to connect identified risks with decisive action and achieve reduced readmissions.
Let’s look at how smart, automated triage via actionable dashboards closes this critical loop, transforming chaos into clarity. Imagine that same busy care coordinator, Ms. Chen, but now her blueBriX dashboard isn’t just a list; it’s a dynamic, intuitive command center. These Actionable dashboards are more than just displays; they are interactive workspaces designed for immediate decision-making and seamless workflow management. They instantly highlight the highest-risk patients, thanks to the real-time data from Part 1, presented with clear visual cues, urgent flags, and a prioritized queue. These dashboards are highly configurable using our low-code no-code platform, allowing organizations to tailor views to specific roles, departments, and workflows. Every provider sees only what they need, when they need it, simplifying even the most complex care coordination processes.
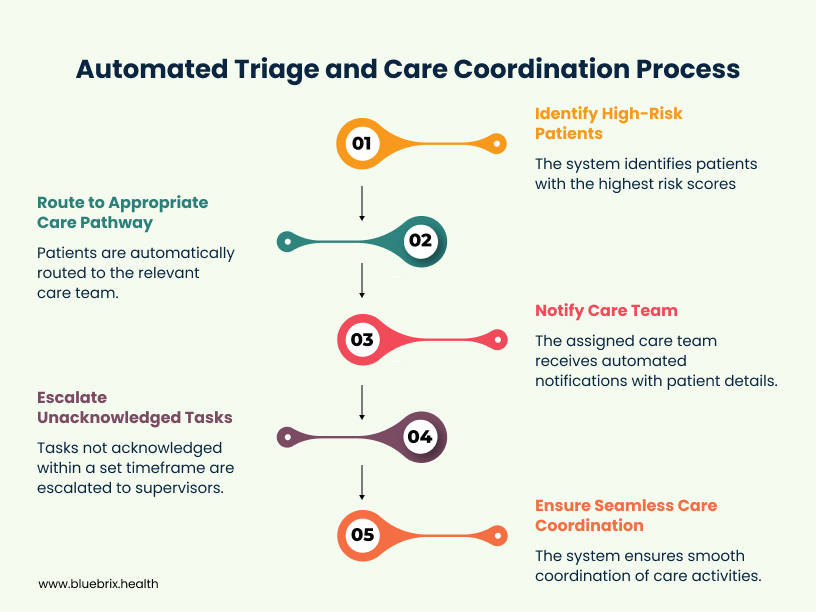
Based on pre-defined, intelligent rules easily configured within our EHR, the system automatically routes the patient to the appropriate care pathway or team. If it’s a patient with complex diabetes and a rising risk score, the system instantly directs them to the specialized chronic care management team’s queue, complete with all relevant medical history. This isn’t just about acute care; this is crucial for preventive interventions. The system can identify patients at risk for chronic disease development and automatically route them to health coaching programs, nutrition counseling, or educational resources, demonstrating a profound commitment to value-based care. This automated routing eliminates guesswork, ensures consistency, and dramatically reduces the time between risk identification and active engagement, directly contributing to reduced readmissions.
Crucially, blueBriX’s integration-agnostic EHR seamlessly connects with existing scheduling systems (or facilitates its own flexible scheduling capabilities), making the critical step of booking follow-up appointments, specialist visits, or program enrolments remarkably easier and faster. Our configurable EHR makes it simple for non-technical users to set up these complex triage rules, adapting to new care models and clinical guidelines without extensive coding or IT support.
Furthermore, blueBriX ensures seamless care coordination, truly closing the loop. The system doesn’t just route; it facilitates. Automated notifications are sent to the assigned care team, complete with all necessary patient details and a clear next step. Escalation protocols are built-in, so if an assigned task isn’t acknowledged or completed within a set timeframe, it’s automatically escalated to a supervisor, ensuring no patient is ever forgotten. This ensures accountability and follow-through, preventing patients from getting lost in the shuffle.
You just saw how blueBriX takes the guesswork and stress out of prioritization, ensuring that every patient receives the precise attention they need, when they need it most, driving both preventive care and reduced readmissions. And as we’ll show, this streamlined process doesn’t just provide better care—it also generates the crucial insights needed to strategically manage entire patient populations through risk stratification and cohort management, which is what we’ll explore in our final chapter.
Next Steps: Ready to Transform Triage into Strategic Action?
We’ve seen how blueBriX transforms individual patient management. Stay tuned for Part 3 of our series, where we’ll explore “Risk Stratification and Cohort Management” and how to impact population health.
Curious about how intelligent triage can specifically enhance your value-based care models and drive down readmission rates? Connect with blueBriX today for a personalized demonstration.