Open-Source Solutions: Empowering Customization and Collaboration
Open-Source Software (OSS) is characterized by its publicly accessible source code, allowing users to view, modify, and distribute the software freely, often under specific open-source licenses. This fundamental principle fosters a collaborative environment where a global community of developers can contribute to the software’s improvement, identify and fix bugs, and adapt it to diverse needs.
Key Advantages of Open Source for Behavioral Health
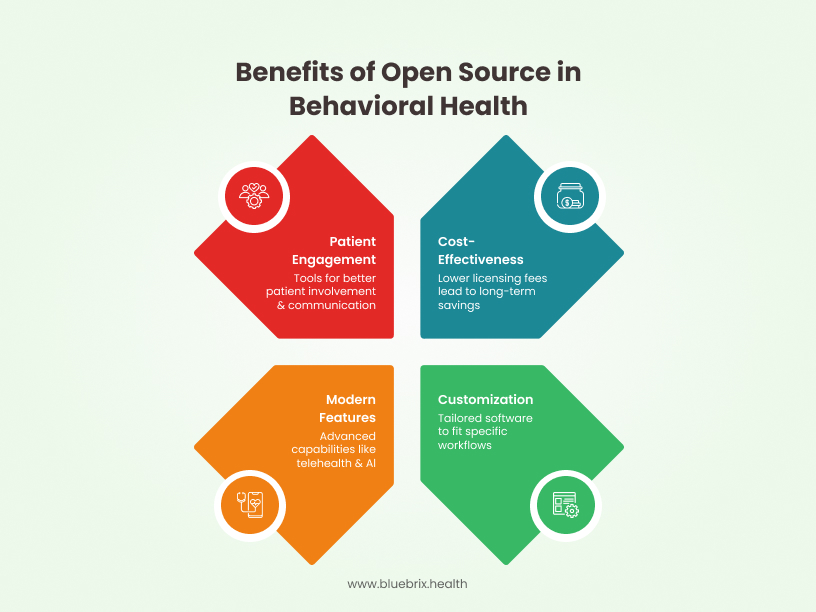
Behavioral health clinics that are budget-conscious, require workflow customization, prioritize data control, have some technical capability, or need strong interoperability should strongly consider open source EHR solutions. These platforms offer flexibility, affordability, and transparency that can be especially valuable in behavioral health settings.
Cost-Effectiveness and Reduced Licensing Fees
One of the most significant attractions of OSS is the typically lower upfront and ongoing costs associated with licensing. While there might be expenses related to implementation, customization, and support, the absence of per-user or per-feature licensing fees can lead to substantial long-term savings, especially for growing clinics or those with a large number of users.
Customization and Flexibility to Fit Specific Workflows
The availability of the source code provides unparalleled flexibility for customization. With OSS, clinics with the necessary technical expertise or access to developers can tailor the software precisely to their operational needs, rather than being constrained by the features offered in off-the-shelf proprietary solutions. This level of customization can lead to increased efficiency, improved data accuracy, and a better fit for the specific nuances of behavioral health practice.
Modern Features and Interoperability
Today’s open-source EHR systems are equipped with cutting-edge features like integrated telehealth modules, AI-powered decision support, and FHIR-based interoperability. These advanced capabilities allow behavioral health clinics to provide virtual care, automate routine workflows, and seamlessly exchange data with labs, pharmacies, and health information exchanges, ensuring comprehensive, real-time patient insights.
Enhanced Patient Engagement
Open-source EHRs also offer patient engagement tools, including secure patient portals. These portals empower patients to access their treatment plans, educational resources, and appointment schedules, while also enabling secure communication with providers. This level of access promotes better patient involvement and adherence to care plans, which is particularly critical in behavioral health settings.
Potential Challenges of Open Source
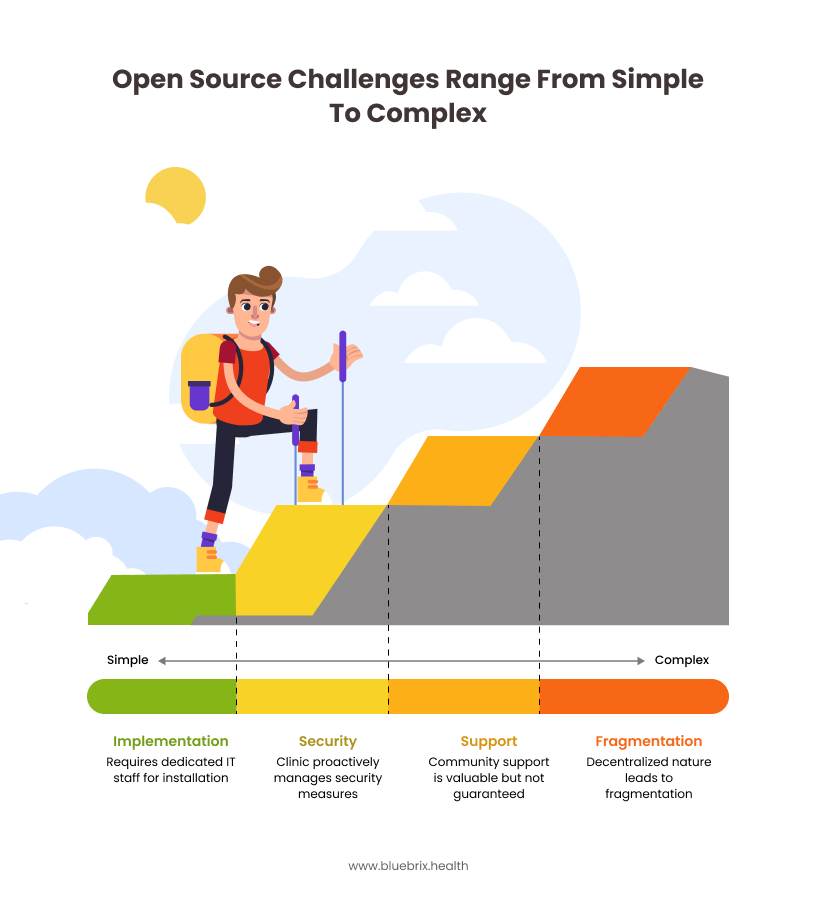
While open source EHRs offer many benefits, clinics should also be aware of potential challenges, such as the need for technical expertise, limited out-of-the-box support, and the responsibility for system maintenance and security.
Technical Expertise Required for Implementation and Maintenance
Implementing and maintaining OSS often requires a higher level of technical expertise compared to user-friendly proprietary solutions. Clinics may need to hire dedicated IT staff or contract with external consultants for installation, configuration, customization, and ongoing maintenance. This can offset some of the initial cost savings if the required technical expertise is significant.
Responsibility for Security and Updates
While the open nature of the code can enhance security through community review, the ultimate responsibility for implementing security measures, applying updates, and ensuring compliance rests with the clinic. Unlike proprietary vendors who typically provide regular security patches and updates, OSS users need to proactively manage these aspects, which can be challenging without dedicated IT resources.
Limited Dedicated Support
While community support can be valuable, it may not always be as readily available or as guaranteed as the dedicated support offered by proprietary software vendors. Response times can vary, and there may not be Service Level Agreements (SLAs) in place. For critical issues requiring immediate attention, this lack of guaranteed support can be a significant drawback for busy behavioral health clinics.
Potential for Fragmentation and Lack of Standardization
The decentralized nature of some open-source projects can lead to fragmentation, with multiple forks or variations of the software emerging. This can make it challenging to choose the most stable and well-supported version. Additionally, OSS solutions may not always adhere to the same level of standardization as proprietary EHR systems, potentially impacting interoperability with other healthcare systems.
Clinics That Benefit Most from Open Source EHRs
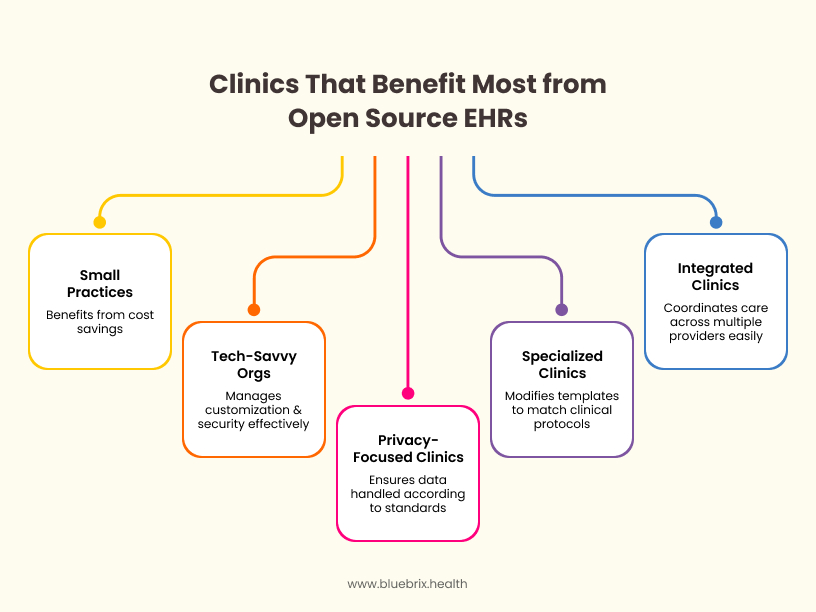
Behavioral health clinics that should consider open source EHR software typically fall into several categories based on their size, budget, workflow needs, and technical capabilities.
Small and Mid-Sized Practices with Limited Budgets
Open source EHRs are free or significantly less expensive than proprietary alternatives, making them ideal for clinics with restricted financial resources. Cost savings are particularly important for solo practitioners, community mental health centers, and organizations serving underserved populations.
Organizations with Unconventional or Highly Specialized Workflows
Behavioral health clinics often require unique documentation, assessment, and treatment planning tools. Open source EHRs allow for deep customization. Clinics can modify templates, forms, and workflows to match their specific clinical protocols, such as substance abuse assessments or trauma evaluations. This flexibility is especially valuable for practices with specialized services or non-standard processes.
Clinics Prioritizing Data Control and Transparency
Open source EHRs provide full transparency and control over patient data, which is a significant advantage for organizations concerned about privacy, compliance, or vendor lock-in. Clinics that want to ensure data is handled according to their own standards, or those wary of third-party data access, benefit from this model.
Tech-Savvy Organizations or Those with dedicated IT Support
Successful implementation and ongoing management of open source EHRs are easier for clinics with staff who are comfortable with technology or have 24X7 access to dedicated IT professionals. These organizations can handle customization, updates, and security more effectively.
Clinics Seeking Interoperability and Integration
Open source EHRs often adhere to industry standards like FHIR and HL7, making it easier to integrate with labs, pharmacies, telehealth platforms, and health information exchanges. This is important for behavioral health clinics that need to coordinate care across multiple providers or settings.
Behavioral Health Clinics That Should Not Consider Open Source EHRs
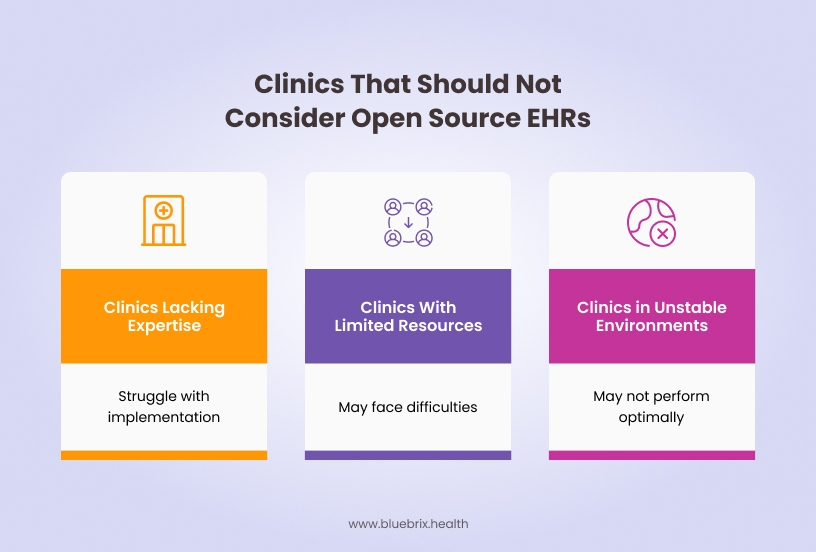
Certain types of behavioral health clinics may find open source EHRs unsuitable due to their unique operational, regulatory, or technical requirements. Key scenarios include:
Clinics Lacking Technical Expertise or IT Support
Open source EHRs often require in-house technical skills for installation, customization, maintenance, and troubleshooting. Clinics without dedicated IT staff or clinicians comfortable with open source software may struggle with implementation and ongoing support, as open source solutions typically lack 24/7 vendor support.
Clinics With Limited Resources for Training and Change Management
Successful adoption of any EHR requires adequate training and change management. Clinics with limited capacity to train staff, manage user resistance, or support ongoing education may face greater difficulties with open source systems, which often lack structured onboarding and user support compared to proprietary vendors.
Clinics in Low-Resource or Unstable Technical Environments
In settings with unreliable power, internet connectivity, or insufficient hardware, open source EHRs may not perform optimally, especially if the system is not designed for offline use or low-resource environments.
Proprietary Software: Streamlined Solutions and Dedicated Support
Proprietary software, in contrast to open source, has its source code exclusively owned and controlled by the developing organization. Users typically purchase a license to use the software under specific terms and conditions, but they do not have the right to access or modify the underlying code. This model is prevalent in the healthcare software industry, with numerous vendors offering EHR, practice management, and other solutions tailored to various medical specialties, including behavioral health.
Key Advantages of Proprietary Software for Behavioral Health
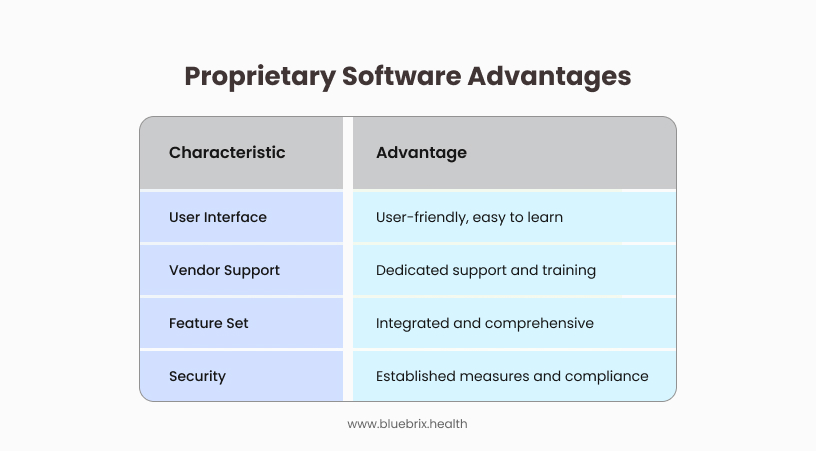
Proprietary behavioral health EHR software delivers significant advantages through tailored workflows, enhanced security, integrated decision support, seamless interoperability, operational efficiency, and specialized vendor support.
User-Friendly Interfaces and Ease of Us
Proprietary software vendors often invest heavily in user interface and user experience design to create intuitive and easy-to-use applications. This can significantly reduce the learning curve for clinicians and administrative staff, leading to faster adoption and increased efficiency. The focus on usability is often a key selling point for proprietary solutions.
Dedicated Vendor Support and Training
A significant advantage of proprietary software is the availability of dedicated support from the vendor. This typically includes comprehensive documentation, training programs, technical assistance via phone, email, or online portals, and often Service Level Agreements (SLAs) that guarantee response times for critical issues. This dedicated support can be invaluable for behavioral health clinics that may lack extensive in-house IT expertise.
Integrated Features and Comprehensive Solutions
Many proprietary vendors offer integrated suites of software that combine EHR functionalities, practice management tools (scheduling, billing, etc.), telehealth capabilities, and other features relevant to behavioral health. This all-in-one approach can streamline workflows, improve data consistency, and reduce the need for integrating disparate systems.
Established Security Measures and Compliance Efforts
They invest significantly in security infrastructure, implement robust security measures, and provide regular security updates to protect sensitive patient data. This can provide clinics with a greater sense of security and reduce the burden of independently managing complex compliance requirements.
Potential Challenges of Proprietary Software
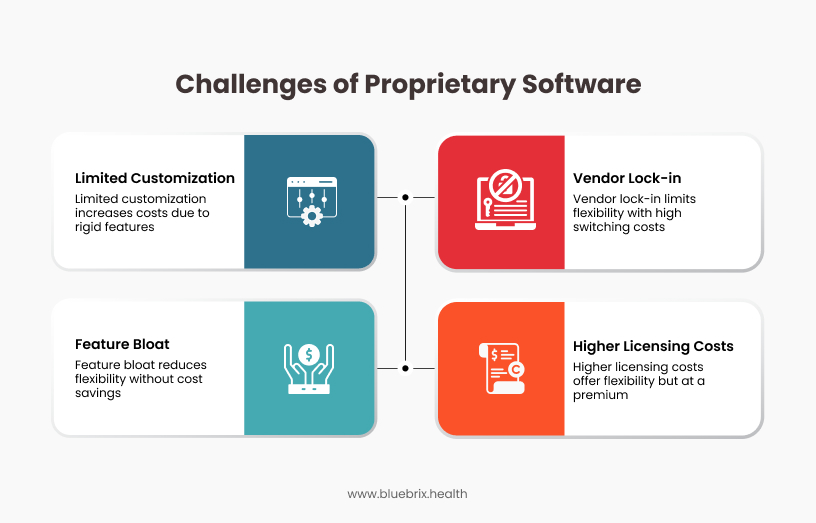
While proprietary behavioral health EHRs offer specialized features, they also present significant challenges like the one listed below.
Higher Licensing Costs and Subscription Fees
Proprietary software typically involves higher upfront licensing costs or ongoing subscription fees compared to open-source alternatives. These costs can be a significant factor, especially for smaller or budget-constrained behavioral health clinics. The total cost of ownership over time can be substantial, particularly if per-user or per-feature fees apply.
Limited Customization Options
The closed nature of proprietary software means that customization options are generally limited to the features and configurations provided by the vendor. Clinics may need to adapt their workflows to fit the software’s capabilities, rather than the other way around. This lack of flexibility can be a significant drawback for clinics with unique or highly specialized needs.
Vendor Lock-in and Dependence
Once a behavioral health clinic invests in a proprietary software solution and integrates it into its operations, switching to a different vendor can be a complex and costly undertaking. This vendor lock-in can limit the clinic’s future flexibility and potentially make them susceptible to price increases or changes in the vendor’s offerings.
Potential for Feature Bloat
In an effort to appeal to a broad range of users, proprietary software can sometimes become bloated with features that are not relevant to the specific needs of a behavioral health clinic. This can lead to a cluttered interface, increased complexity, and potentially higher costs for features that are never utilized.
Types of Behavioral Health Clinics That Benefit Most from Proprietary Software EHR
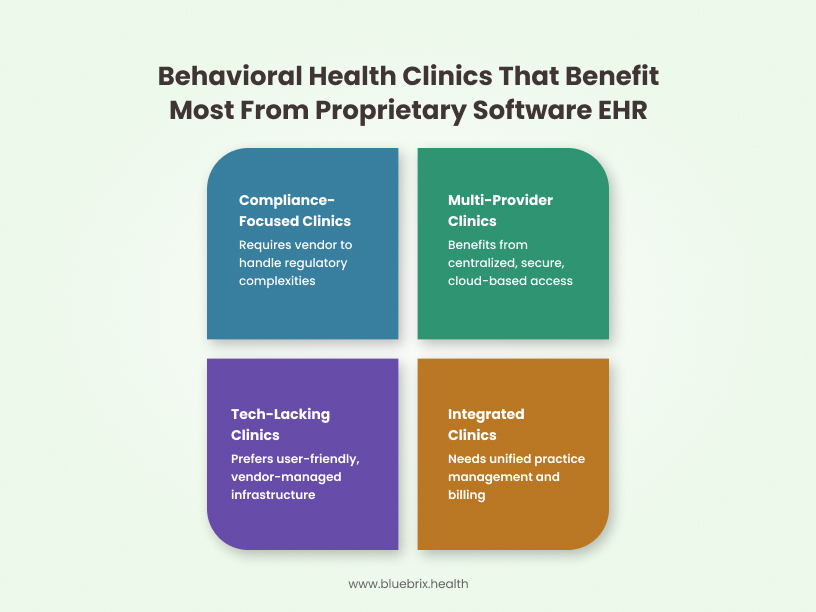
Proprietary software EHRs are particularly beneficial for behavioral health clinics that require tailored solutions, integrated practice management, and secure, efficient workflows-regardless of size or specialty.
Clinics with Limited Technical Expertise
Implementing and maintaining an open-source EHR can require a certain level of technical proficiency or the willingness to invest in IT support. Clinics that lack this expertise may find the user-friendly interfaces and vendor-managed infrastructure of proprietary systems more suitable.
Clinics Focused on Specific Compliance Requirements
While both open-source and proprietary EHRs can be HIPAA compliant, proprietary vendors often handle the complexities of regulatory updates and compliance measures, providing assurance to clinics that may not have the resources to manage this independently.
Clinics Favoring Integrated Practice Management and Billing
Proprietary EHRs often come tightly integrated with practice management and billing modules. This can streamline administrative tasks, improve billing accuracy, and simplify revenue cycle management for clinics that prefer a unified system.
Multi-Location or Multi-Provider Clinics
Clinics with multiple locations or providers benefit from the centralized data management and secure, cloud-based access offered by proprietary EHRs. These features ensure all team members have up-to-date patient information, supporting coordinated care and reducing errors.
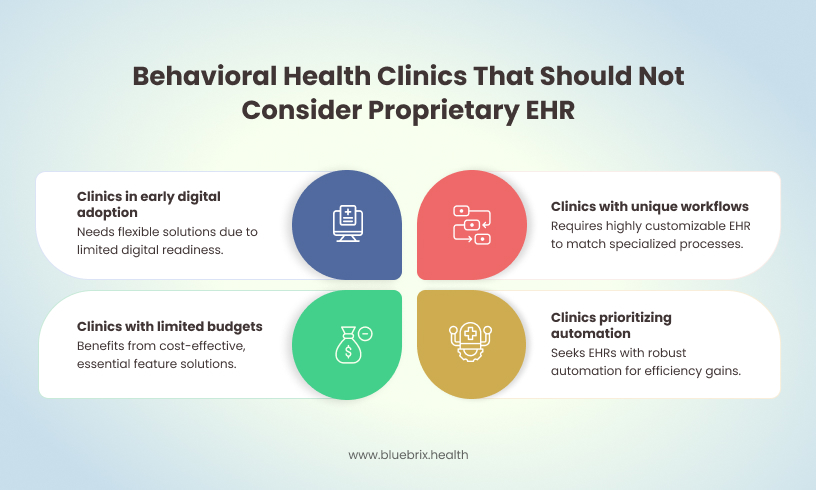
Behavioral Health Clinics That Should Not Consider Proprietary EHR
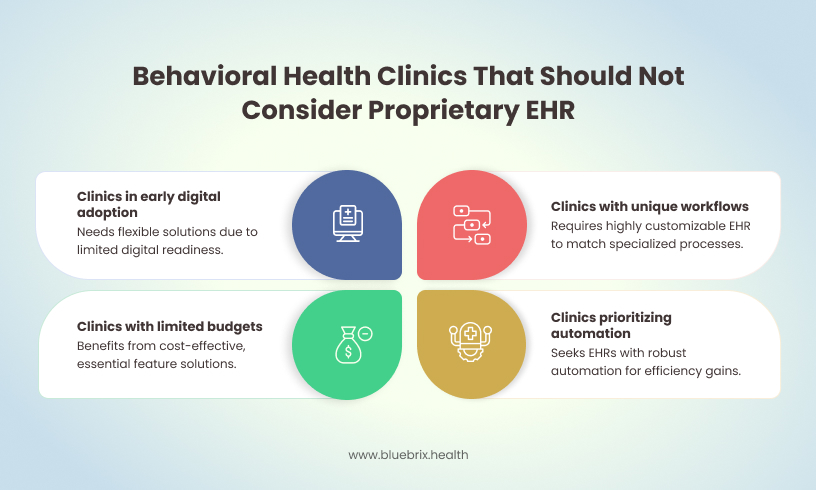
Behavioral health clinics that require robust physical health integration, high interoperability, extensive customization, automation, or have limited budgets and IT resources should be cautious about adopting proprietary EHRs. Instead, they should seek solutions that align with their specific clinical, operational, and financial needs
Clinics with Unique or Highly Customized Workflows
If a clinic’s workflows are highly specialized and the proprietary EHR cannot be sufficiently customized to match these needs, staff may be forced to change their established processes, leading to inefficiency and frustration. Clinics should avoid systems that cannot adapt to their workflow rather than forcing clinicians to adapt to the software.
Clinics with Limited Budgets or Small Scale
Smaller clinics or those with tight budgets may find the cost of proprietary EHRs-including licensing, customization, and ongoing maintenance-prohibitive. These clinics might benefit more from open-source or lower-cost cloud-based solutions that offer essential features without high upfront or recurring expenses.
Clinics in Early Stages of Digital Adoption
Organizations still reliant on paper-based systems or with minimal IT infrastructure may struggle with the complexity and resource demands of implementing a proprietary EHR. These clinics may benefit from phased or more flexible digital solutions as they build readiness for comprehensive EHR adoption.
Clinics Prioritizing Automation and Efficiency
If a proprietary EHR offers limited automation for routine tasks (like order sets, billing, or documentation), clinics seeking to streamline operations and reduce manual work may find such systems inadequate. Automation is increasingly a baseline expectation, and systems lacking these features can create unnecessary administrative burdens.
Platform Solutions: Leveraging Ecosystems and Scalability
Platform solutions represent a more recent evolution in healthcare software. These are typically comprehensive EHR or practice management systems that offer a core set of functionalities but also provide an ecosystem or marketplace where third-party applications can be integrated. This approach aims to combine the benefits of a robust, integrated system with the flexibility and specialized capabilities of external applications.
Key Advantages of Platform Solutions for Behavioral Health
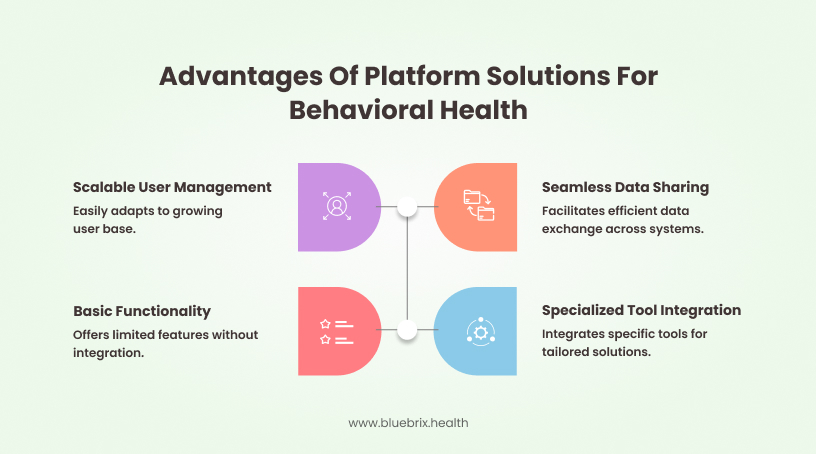
Platform solutions for behavioral health are transforming care delivery by making it more accessible, efficient, patient-centered, and secure, while supporting both providers and patients in achieving better outcomes
Extensibility and Integration with Third-Party Applications
The key advantage of platform solutions is their ability to integrate with a wide range of specialized third-party applications. For behavioral health clinics, this can mean access to specialized tools for outcome measurement, telehealth, patient engagement, billing for specific treatment modalities, and more. This allows clinics to tailor their software ecosystem to their precise needs without being limited to the features offered by a single vendor.
Scalability to Accommodate Growth
Platform solutions are often designed with scalability in mind, allowing clinics to easily add users, expand functionalities through integrations, and adapt to increasing patient volumes and evolving needs. This scalability can be particularly attractive for growing behavioral health organizations.
Potential for Specialized Behavioral Health Integrations
As the demand for specialized behavioral health technology grows, platform providers are increasingly focusing on integrating with applications that cater specifically to this field. This can provide clinics with access to cutting-edge tools and technologies tailored to their unique requirements.
Streamlined Data Sharing and Interoperability
Platform solutions often prioritize data sharing and interoperability, both within the platform’s ecosystem and with external healthcare systems. This can facilitate seamless communication and coordination of care, which is crucial in the complex healthcare landscape.
Potential Challenges of Platform Solutions
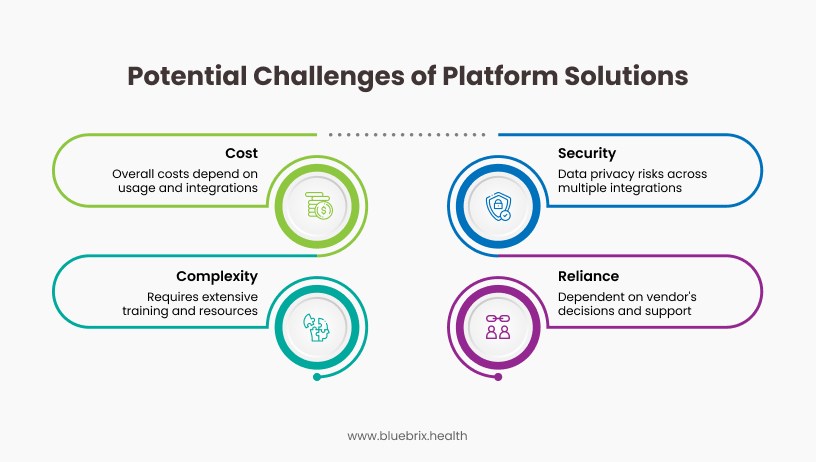
Platform solutions have become essential for modern behavioral health practices, offering integrated care management, patient engagement, and data analytics. However, despite their many advantages, these systems come with unique challenges, ranging from data security and integration complexities to customization limitations and regulatory hurdles.
Complexity and Learning Curve
The extensive functionality and integration capabilities of platform solutions can lead to increased complexity and a steeper learning curve for users. Clinics may need to invest more time and resources in training staff to effectively utilize the platform and its integrated applications.
Potential for Higher Overall Costs Depending on Usage and Integrations
While the core platform may have a base cost, the overall cost can escalate depending on the number of users, the specific integrations chosen, and the pricing models of the third-party applications. Clinics need to carefully evaluate the total cost of ownership, including the costs of all necessary integrations.
Reliance on the Platform Vendor’s Ecosystem
The effectiveness of a platform solution heavily relies on the quality and availability of the third-party applications in its ecosystem. Clinics are somewhat dependent on the platform vendor’s decisions regarding which applications are supported and how the integrations are maintained.
Data Privacy and Security Considerations Across Multiple Integrations
Integrating multiple third-party applications can introduce additional data privacy and security considerations. Clinics need to ensure that all integrated applications comply with relevant regulations and that data sharing between systems is secure and appropriately managed. The responsibility for overseeing the security of the entire integrated ecosystem can be more complex than with a single, unified proprietary solution.
Types of Behavioral Health Clinics That Could Benefit from Platform EHR

Behavioral health EHR (Electronic Health Record) platforms offer tailored features that can enhance a wide variety of behavioral health clinics. The following types of clinics stand to benefit significantly.
Counseling Centers
Clinics offering individual, couples, or family counseling can use EHRs to streamline documentation, scheduling, and billing, while securely managing sensitive patient information.
Psychiatric Practices
These clinics benefit from integrated clinical documentation, e-prescribing, and medication management features, supporting the complex needs of psychiatric care.
Substance Use Disorder Treatment Centers
EHRs help with compliance, confidentiality (especially under 42 CFR Part 2), and coordination of care across different providers, which is crucial for addiction treatment.
Community Mental Health Centers
These organizations, often serving high volumes and diverse populations, benefit from scalable EHR solutions that support care coordination, outcome tracking, and reporting.
Telehealth-Based Behavioral Health Clinics
Clinics providing remote therapy or psychiatric services can use EHRs with integrated telehealth support, secure messaging, and virtual documentation features.
Types of Behavioral Health Clinics That Should Not Consider Platform EHRs
While platform EHRs offer significant benefits, certain behavioral health clinics may find them unsuitable due to specific challenges and limitations.
Clinics With Minimal Documentation Needs
Solo practitioners or very small clinics that only require basic recordkeeping and do not need advanced features (like integrated billing, telehealth, or data analytics) may find platform EHRs unnecessarily complex and costly for their needs.
Clinics With Low Digital Literacy or High Resistance to Change
Practices where staff are not comfortable with technology or resistant to changing workflows may experience significant usability challenges, leading to poor adoption, dissatisfaction, and even potential disruptions in patient care.
Clinics Focused Primarily on Non-Clinical Services
Organizations that primarily offer non-clinical behavioral health services (e.g., support groups, educational workshops without individual therapy) might not need the extensive clinical documentation and charting features of a platform EHR. A simpler client management system or even dedicated scheduling and communication tools might be more appropriate.
Clinics Where Interoperability is a Minor Concern
While interoperability is generally beneficial, some very small or isolated practices might not have a significant need to exchange data with other healthcare providers or systems. In such cases, the interoperability features of a platform EHR might be an unnecessary cost and complexity.
Key Considerations for Choosing the Right Solution
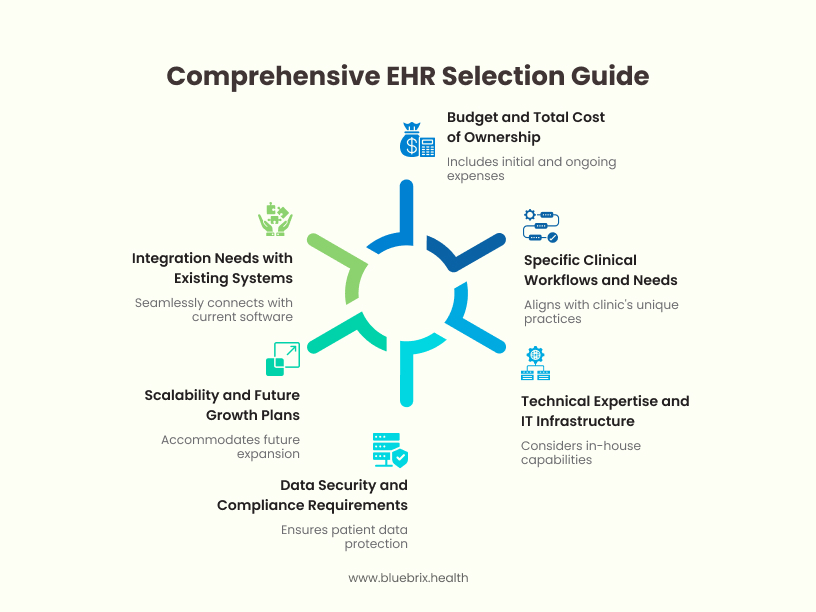
The decision of whether to choose Open Source, Proprietary, or a Platform solution is a multifaceted one that requires careful consideration of a behavioral health clinic’s unique circumstances and priorities. Several key factors should be weighed:
Budget and Total Cost of Ownership
This includes not only the initial purchase or subscription costs but also the ongoing expenses related to implementation, customization, maintenance, support, training, and potential upgrades. A thorough analysis of the total cost of ownership over the long term is crucial.
Specific Clinical Workflows and Needs
The chosen software must align with the clinic’s specific clinical workflows, treatment modalities, documentation requirements, and reporting needs. Clinics with highly specialized practices may find the customization capabilities of open source or the integration options of platforms more appealing.
Technical Expertise and IT Infrastructure
The level of in-house technical expertise and the existing IT infrastructure will significantly influence the feasibility of implementing and maintaining different types of solutions. Open source often requires more technical proficiency, while proprietary solutions typically offer more user-friendly interfaces and vendor support.
Data Security and Compliance Requirements
Ensuring the security and privacy of sensitive patient data is paramount for behavioral health clinics. The chosen software must meet all relevant regulatory requirements. While both proprietary vendors and open-source communities can prioritize security, the responsibility for implementation and ongoing compliance ultimately rests with the clinic. Platform solutions require careful consideration of the security implications of integrating multiple applications.
Scalability and Future Growth Plans
The software should be able to scale to accommodate the clinic’s future growth in terms of patient volume, staff size, and service offerings. Platform solutions are often designed with scalability in mind, while open-source solutions can be scaled with the right technical expertise.
Integration Needs with Existing Systems
Clinics may already have existing software systems (e.g., billing software, telehealth platforms). The ability of the new software to integrate seamlessly with these existing systems is an important consideration to avoid data silos and streamline workflows. Platform solutions often excel in this area due to their focus on integration.
Why Platform-Based EHR Is Generally a Better Choice for Behavioral Health Clinics
When comparing platform-based EHRs to open source and proprietary solutions for behavioral health clinics, platform-based EHRs offer several distinct advantages that make them a superior choice in most cases.
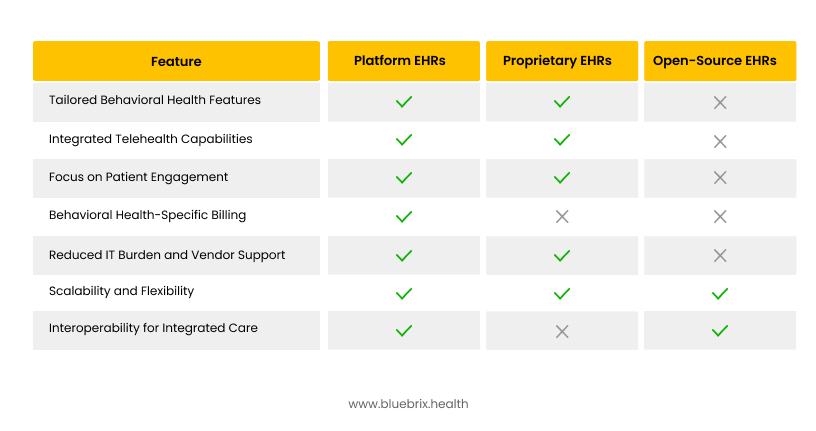
Why Platform EHRs Stand Out
- Platform EHRs provide comprehensive, behavioral health-specific features without requiring extensive customization.
- They offer integrated telehealth, patient engagement, and billing capabilities, reducing administrative burdens.
- Platform EHRs come with dedicated support and lower IT maintenance costs, making them ideal for growing practices.
- Built-in interoperability supports seamless care coordination, critical for holistic behavioral health treatment.
Why blueBriX Is a Strong Choice for Platform-Based EHR in Behavioral Health Clinics
blueBriX stands out as a platform-based EHR purpose-built for behavioral health, offering features and design principles that directly address the unique challenges faced by clinics in this field.
Key Advantages of Choosing blueBriX
blueBriX is a strategic, future-proof choice for behavioral health clinics seeking a platform-based EHR. Its specialized features, automation, seamless integration, and compliance focus help clinics deliver better care, reduce administrative burden, and adapt to the evolving landscape of behavioral health.
Purpose-Built for Behavioral Health
blueBriX is designed specifically for behavioral health, not as a generic EHR with add-ons. This means you get custom documentation templates, flexible treatment planning, and program management tools tailored for mental health, substance use disorder, and intellectual/developmental disability care.
Streamlined, End-to-End Workflows
From intake to discharge, blueBriX connects clinical, administrative, and billing processes in a single platform. This integration reduces errors, eliminates duplicate data entry, and saves time for both clinicians and administrative staff.
AI-Powered Documentation
Automated note suggestions and AI-assisted documentation tools reduce paperwork and help clinicians spend more time with patients. This also helps prevent burnout by making documentation less burdensome and more accurate.
Integrated Telehealth
blueBriX offers built-in telehealth capabilities, allowing providers to conduct, document, and bill for virtual sessions without switching apps or duplicating work. This is essential for clinics offering hybrid or remote care models.
Advanced Scheduling and Patient Engagement
The platform supports online booking, automated reminders, and digital intake forms, reducing no-shows and administrative workload while improving patient access and engagement.
Robust Billing and Revenue Cycle Management
blueBriX automates claims, manages denials, and supports mental health-specific coding, helping clinics get paid faster and with fewer errors.
Compliance and Security
The system is fully compliant with HIPAA, 42 CFR Part 2, and HITRUST, featuring end-to-end encryption, role-based access, and audit logs to safeguard sensitive behavioral health data.
Customizable and Scalable
Clinics can tailor workflows, templates, and dashboards to fit their unique needs, whether operating as a solo practice or a multi-location organization. This flexibility supports growth and adaptation as care models evolve.
Real-Time Collaboration and Care Coordination
Providers can collaborate within the platform, share notes, and manage referrals seamlessly, ensuring continuity of care and effective team-based treatment.
Continuous Support and User-Centered Design
blueBriX incorporates feedback from real behavioral health teams, ensuring the system evolves with your needs. Onboarding, peer mentoring, and ongoing support are built into the experience.