Whether you are part of a small practice, a large physician group, clinic or hospital, your practice’s compensation and cash flow depend on timely and accurate coding and submission of your medical services to the insurance carriers. In this blog we’ll help you understand if outsourcing medical coding is the right fit for your practice.
In healthcare, administrative overload isn’t just an inconvenience—it’s a growing threat to operational efficiency and revenue integrity. Practices are grappling with staff shortages, ever-evolving ICD-10 and CPT code updates, and increasing claim denials tied to documentation gaps or coding errors. Meanwhile, the pressure to accelerate reimbursements and remain compliant with payer-specific rules has never been higher. Amid this chaos, medical coding has emerged as a high-stakes function—central to both compliance and cash flow. With in-house teams stretched thin and error margins tightening, many healthcare organizations are now asking a critical question: Is outsourcing medical coding the smarter, more sustainable move?
But is it the right move for your practice? There’s no simple yes or no answer. This decision requires a thoughtful assessment of your circumstances, challenges, and goals. At blueBriX, we understand the nuances of healthcare administration, and this guide is designed to offer a balanced perspective—helping you make an informed decision about outsourcing your medical coding.
Why Practices Consider Outsourcing
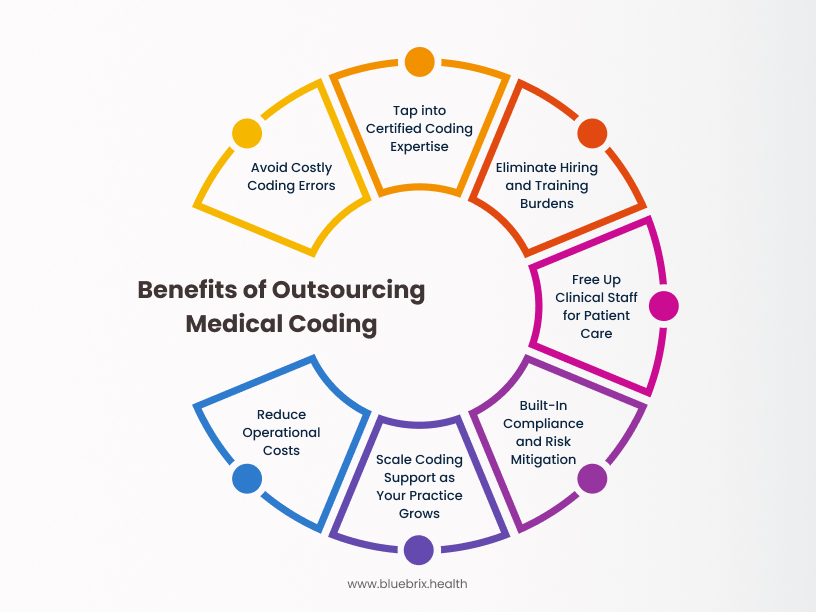
Outsourcing medical coding is a cost-saving tactic as well as a strategic response to the growing pressures, complexities, and operational challenges faced by healthcare practices today. It’s also a strategic move aligned with the industry’s shift toward value-based care (VBC). Here’s why more practices are making the switch.
Increasing Complexity of Medical Coding
Keeping up with annual updates to ICD-10, CPT, and HCPCS codes, payer-specific rules, and evolving regulatory requirements demands significant time and expertise. Mistakes in coding can trigger claim denials, reimbursement delays, and revenue loss. The added scrutiny around medical necessity and documentation only increases the challenge, requiring in-depth knowledge to stay compliant and efficient.
Access to Certified Expertise
Top-tier outsourcing partners bring specialized coders with certifications and experience across multiple specialties. These professionals stay up to date with changing coding standards and payer policies—something that’s often hard to maintain in-house. This depth of knowledge directly translates to greater accuracy, fewer denials, and faster reimbursements.
Staffing Relief for Healthcare Practices
The hiring market for medical coders is tight—and expensive. Recruiting, onboarding, and retaining certified professionals comes with high costs and workflow risks due to turnover. Outsourcing relieves your practice from these burdens and eliminates the need for constant training cycles, helping you maintain continuity without overextending your internal resources.
Reclaiming Clinical Time
Administrative overload, especially around coding and billing, pulls clinical staff away from direct patient care. This fragmentation contributes to burnout and lost productivity. By offloading coding to experts, providers and staff can refocus on high-value tasks: diagnosing, treating, and building stronger patient relationships.
Compliance and Risk Management
Medical coding is governed by HIPAA, OIG, and payer-specific rules—all of which are continuously evolving. Outsourcing partners like blueBriX implement strong internal quality control and operate under Business Associate Agreements (BAAs), ensuring regulatory compliance and reducing exposure to audits or penalties.
Scalability and Operational Flexibility
Patient volumes fluctuate. Outsourcing allows practices to scale their coding support up or down as needed—whether due to seasonal spikes, provider absences, or growth. This adaptability helps maintain efficiency without the fixed costs of full-time hires or overcommitting internal staff.
Cost-Efficiency
Outsourcing reduces overhead tied to in-house teams—salaries, benefits, office space, software, and training. Many vendors operate on flexible, pay-per-service models, allowing your coding spend to align with actual workload. The added benefit? Reduced claim rework, fewer denials, and better cash flow.
Potential Challenges and Considerations in Outsourcing Medical Coding

While the benefits of outsourcing medical coding are significant and can truly transform a healthcare practice’s operations, it’s crucial for healthcare providers to approach this decision with a clear understanding of potential challenges. Acknowledging and preparing for these considerations is key to a successful partnership.
Loss of Direct Control
Some practices naturally feel apprehensive about giving up direct control over a function as critical as medical coding. Concerns about reduced oversight, potentially slower response times for specific queries, and less visibility into day-to-day operational steps are valid. To mitigate this, it’s essential to establish clear communication channels upfront, define explicit Service Level Agreements (SLAs), and maintain regular, structured contact with your outsourcing partner.
Data Security and Confidentiality (HIPAA Compliance)
Entrusting (PHI) to an external entity demands utmost care in ensuring robust data security and unwavering HIPAA compliance. Providers must thoroughly vet potential outsourcing partners, scrutinizing their security protocols, certifications, and proven experience in handling sensitive healthcare data. A comprehensive and legally sound Business Associate Agreement (BAA) explicitly outlining responsibilities for data protection is non-negotiable and necessary to the partnership.
Communication and Coordination Challenges
Effective communication and seamless coordination between your practice and the outsourced coding team are absolutely vital for a successful partnership. Potential hurdles can include time zone differences, unclear reporting structures, or inadequate communication channels. These factors can slow down issue resolution, affect collaborative efforts, and ultimately impact your revenue cycle performance. That’s where experienced vendors like blueBriX make the difference. We’ve built our delivery model around proactive communication, dedicated account managers, and well-defined reporting structures.
Integration with Existing Systems
A critical technical challenge involves ensuring the chosen outsourcing partner can seamlessly integrate with your existing Electronic Health Record. Compatibility and efficient, secure data exchange are essential for a smooth workflow, accurate coding, and avoiding manual workarounds. Always inquire about their experience with your specific EHR/EMR system and the processes they have in place for integration.
Cultural and Specialty Alignment
The success of an outsourcing partnership often hinges on the partner’s understanding of your healthcare provider’s unique culture, values, and, most importantly, its specialty-specific coding requirements. A lack of alignment in these areas can lead to misunderstandings, inconsistent coding practices, and potentially lower satisfaction for both your providers and your patients.
Dependency on External Vendors
Relying heavily on a third-party vendor for a critical function like medical coding can create a degree of long-term dependency. This might make it challenging to switch providers down the line if issues arise, or to even consider bringing the coding function back in-house. Practices should consider their long-term strategy and the vendor’s reliability.
Quality Control and Performance Monitoring
While outsourcing aims for improved accuracy, maintaining high coding accuracy and compliance requires rigorous quality assurance processes. Providers must ensure the outsourcing partner has strong internal quality control measures, invests in regular coder education and auditing, and offers transparent performance monitoring with clear metrics to ensure ongoing accountability and high claim acceptance rates.
Is Outsourcing Right for Your Practice? Key Questions for Self-evaluation
Deciding whether to outsource medical coding requires a thoughtful evaluation of your practice’s unique circumstances. Consider the following key questions:
Current Performance
- What is your current claim denial rate? Are coding errors a significant contributing factor?
- How long does it currently take for your practice to receive payment on submitted claims?
- Are you experiencing challenges with coder recruitment, retention, or training?
- Do you have a clear understanding of the total cost (salary, benefits, overhead) associated with your current in-house coding operations?
Understanding the strengths and gaps in your current setup is the foundation of any outsourcing decision. These questions help diagnose whether internal inefficiencies are holding your revenue cycle back.
Operational Fit
- Does your medical specialty require highly specialized and niche coding knowledge? Does your current team possess this expertise?
- Are you a small practice where the cost of a full-time, certified in-house coder might be disproportionately high?
- Are you a large or rapidly growing practice struggling to scale your coding resources to keep pace with patient volume?
The complexity and scale of your practice directly influence your coding demands. These questions help assess whether your current resources align with your specialty and patient volume.
Financial Strategy
- Are you actively looking for ways to reduce overhead costs and improve your bottom line?
- Are you aiming to optimize your revenue cycle, reduce claim denials, and improve cash flow?
Medical coding impacts revenue at every level. These questions align the decision to outsource with your broader financial objectives.
Risk & Compliance Readiness
- How comfortable are you with entrusting sensitive patient data to a third-party vendor, provided they meet stringent security and compliance standards?
- Are you prepared to invest the time and resources necessary to conduct thorough due diligence in selecting the right outsourcing partner?
Long-Term Objectives
- What are Your Long-Term Strategic Goals?
- Do you want to free up your internal staff to focus more on patient care, practice growth, and other strategic initiatives?
- Are you anticipating significant expansion or changes in your practice that would strain your existing coding resources?
Outsourcing isn’t just a short-term fix and it involves handing over critical tasks to an external partner. These questions help evaluate your readiness and comfort level with that transition.
What to Look for in a Medical Coding Outsourcing Partner
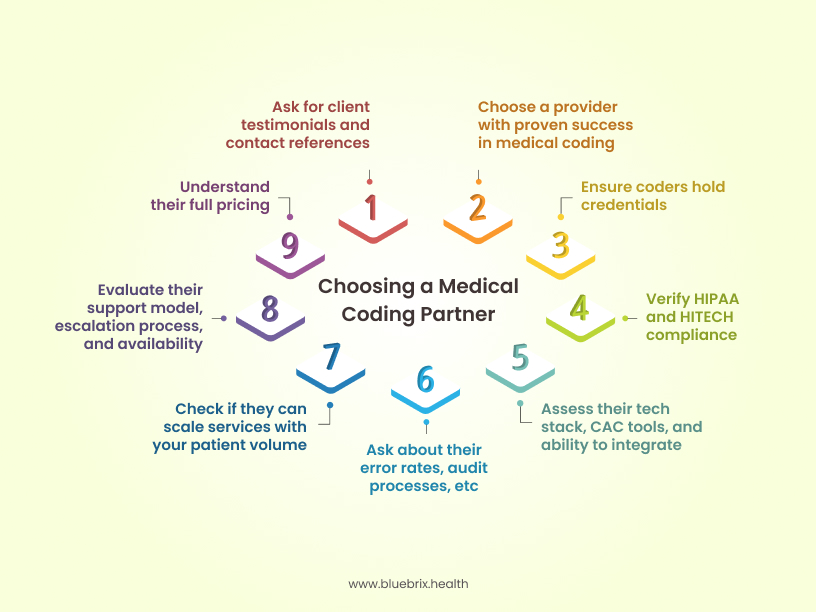
Once you’re certain that outsourcing medical coding might be the right move for your practice, carefully evaluating potential partners is the next step. Here are the key criteria to consider when making this critical decision:
Experience and Specialization
- Look for a provider with a proven track record specifically in medical coding, ideally within your specific medical specialty. Specialized expertise ensures accurate coding for the unique procedures and diagnoses relevant to your field.
- Ask about their longevity in business, their client retention rates, and their experience with practices similar in size and scope to yours.
Certified and Qualified Coders
- Ensure the outsourcing company employs certified medical coders with recognized credentials from reputable bodies such as AAPC (American Academy of Professional Coders) or AHIMA (American Health Information Management Association) (e.g., CPC, CCS, COC).
- Confirm that their coders receive ongoing education and training to stay current with the latest coding standards, regulatory updates, and payer-specific guidelines.
Compliance and Data Security
- Verify their unwavering commitment to HIPAA compliance and other relevant healthcare regulations (e.g., HITECH Act) to rigorously protect patient health information (PHI).
- Inquire about their specific security protocols, the robustness of their security infrastructure, and any history of data breaches or compliance issues. A comprehensive Business Associate Agreement (BAA) is non-negotiable.
Technology and Integration Capabilities
- Assess the technology stack they utilize, including their coding software, use of advanced tools like Computer-Assisted Coding (CAC), and their compatibility with your existing Electronic Health Record (EHR) or Electronic Medical Record (EMR) system.
- Seamless integration with your current systems is essential for efficient workflows and accurate, secure data transfer.
Quality Assurance and Accuracy
- Inquire about their internal quality control processes, including their typical error rates, auditing practices, and how they ensure consistent coding accuracy.
- Look for partners that provide regular, transparent feedback reports on coding accuracy and claim performance, demonstrating a strong focus on minimizing errors and denials.
Scalability and Flexibility
- Confirm their ability to easily scale services up or down based on your practice’s fluctuating patient volume, seasonal trends, or periods of staff absence.
- Their flexibility in service offerings should ensure that your practice’s evolving needs can be met without disruption.
Responsiveness and Communication
- Assess their communication channels (e.g., dedicated account manager, online portal, direct phone lines), their responsiveness to queries, and their approach to issue resolution.
- Clear, prompt, and proactive communication is vital for smooth collaboration and timely problem-solving, preventing backlogs and misunderstandings.
Transparent Pricing Structure
- Understand their complete pricing model—whether it’s a flat fee per claim, percentage-based, or another structure—and ensure there are no hidden or variable costs that could lead to unexpected expenses.
- Compare quotes and detailed contract terms from multiple providers to ensure you are receiving competitive value for the services rendered.
Reputation and References
- Request and thoroughly check client references and testimonials to gauge their reputation, reliability, and service quality from actual users.
- Directly contact references to learn about their real-world experience regarding ease of working together, problem-solving, and overall satisfaction with the outsourcing partner.
KPIs to Track After Outsourcing Medical Coding
These metrics give you a clear, ongoing picture of how well your outsourcing partner is performing and whether the partnership is actually delivering ROI.
Clean Claim Rate (CCR)
Tracks the percentage of claims paid on first submission without edits or rework. A higher CCR means fewer delays and denials.
Benchmark: 95%+ is ideal; 75–85% is common industry average.
Denial Rate
Measures how many claims get denied relative to total submissions. This reflects both coding accuracy and documentation quality.
Benchmark: 5–10% is average; <1% is best-in-class.
Days in Accounts Receivable (A/R)
Indicates how quickly you’re getting paid. This ties directly to coding speed, accuracy, and billing process efficiency.
Benchmark: <30 days is excellent; 40–50 days is typical; >60 days needs review.
Discharged But Not Coded (DNC)
Shows the volume of patient records waiting to be coded. Delays here slow down billing and disrupt cash flow.
Benchmark: Keep under 48 hours.
Coding Accuracy Rate
Represents the percentage of codes correctly assigned per industry standards and documentation.
Goal: As close to 100% as possible.
Claim Lag Time
Measures how long it takes from the date of service to claim submission. Shorter times reduce delays and improve revenue recognition.
Goal: As low as possible—ideally under 3 days.
Net Collection Rate
Reflects how much of your collectible revenue you’re actually capturing after adjustments.
Goal: As close to 100% as possible.
SLA Compliance
Monitors whether your coding partner is meeting agreed-upon metrics like turnaround time, accuracy, and responsiveness.
Goal: 100% compliance.
Why blueBriX is the best Medical Coding Outsourcing Partner for Your Practice
Having weighed the factors, understood the challenges, and identified the essential criteria for a successful partnership, we can say that blueBriX aligns perfectly with provider’s needs. At blueBriX, we are more than just an outsourcing partner; we try to be a strategic extension of your practice, dedicated to optimizing your revenue cycle and freeing you to focus on patient care.
Here’s why blueBriX is consistently chosen as a preferred medical coding outsourcing partner:
Experience and Specialization
blueBriX has a proven track record in medical coding, serving a diverse range of specialties for more than 2 decades. Our deep institutional knowledge, built over years in the industry, ensures that whether your practice handles common procedures or highly complex, niche diagnoses, our experts have the specialized expertise to code accurately and efficiently.
Certified and Highly Qualified Coders
Our team is comprised exclusively of highly certified medical coders, holding their credentials from recognized bodies like AAPC and AHIMA. We believe in continuous improvement, which is why blueBriX invests heavily in ongoing education and rigorous training programs. This practice ensures our coders are always at the forefront of the latest coding standards, regulatory updates, and payer-specific guidelines, minimizing errors and maximizing compliance.
Compliance and Data Security
At blueBriX, HIPAA compliance isn’t just a buzzword; it’s the foundation of our operations. We adhere to the strictest regulatory requirements to protect patient health information (PHI) with robust security protocols and state-of-the-art infrastructure. Our comprehensive Business Associate Agreements (BAAs) reinforce our commitment to safeguarding your sensitive data, giving you absolute peace of mind.
Superior Quality Assurance and Accuracy
blueBriX implements rigorous multi-layered quality control processes and performs regular internal audits to maintain exceptionally low error rates. We are dedicated to delivering consistently accurate coding, leading to higher clean claim submission rates and faster reimbursements. We provide transparent performance reports, so you always have full visibility into our accuracy metrics.
Scalability and Unmatched Flexibility
We understand that patient volumes can fluctuate. blueBriX offers scalability, allowing your practice to easily adjust coding resources up or down based on your evolving needs. Whether you’re experiencing a seasonal surge, planning an expansion, or simply managing staff absences, our flexible models ensure your coding needs are consistently met without the burden of hiring or managing fluctuating internal staff.
Transparent and Proactive Communication
We believe strong partnerships are built on clear and consistent communication. blueBriX assigns dedicated account managers, provides easy-to-access communication channels, and offers transparent reporting mechanisms. Our team is highly responsive to queries and proactive in addressing any potential issues, ensuring a smooth and collaborative working relationship.
Clear and Competitive Pricing Structure
blueBriX is committed to transparency. Our pricing models are straightforward, competitive, and designed to offer exceptional value without any hidden fees. We work with you to understand your specific needs and provide a clear cost structure that helps you budget effectively and realize tangible cost savings.
Proven Reputation and Trusted References
Our strong industry reputation is built on delivering consistent results and long-term client relationships. We are confident in our service quality and are always happy to provide client references and testimonials, allowing you to hear directly from practices that have achieved remarkable success by partnering with blueBriX.
Conclusion
The decision of whether to outsource medical coding is a significant one that can have a profound impact on your practice’s financial health and operational efficiency. While it offers numerous potential benefits, including cost savings, access to expertise, and improved compliance, it’s crucial to carefully consider the potential challenges and ensure you choose the right partner.
If you’re navigating these considerations and exploring whether outsourcing medical coding is the right fit for your practice, blueBriX offers comprehensive solutions tailored to your unique needs. Our expert team of certified medical coders is ready to ensure accuracy, compliance, and an optimized revenue cycle, allowing you to focus on providing exceptional patient care.
Ready to explore if outsourcing medical coding is the right fit for your practice?
Frequently Asked Questions
In value-based care accurate and timely coding is foundational to quality reporting, risk adjustment, and population health insights. Outsourcing ensures you have access to certified, specialized coders who can handle complex, VBC-aligned coding (e.g., HCC, RAF, HEDIS) with precision and speed. This reduces documentation gaps, improves coding integrity, and drives better performance on payer contracts tied to patient outcomes and chronic condition capture.
Yes. An experienced coding partner can directly impact your HEDIS scores, RAF capture, STARS ratings, and other VBC-related quality metrics by ensuring compliant and complete documentation coding. This enables better reporting to payers and CMS, improves risk adjustment accuracy, and ensures that conditions contributing to shared savings models are properly reflected.
At blueBriX, our coders are trained to support value-based care models. They understand how to code for risk adjustment, quality reporting, and payer-specific guidelines. We work closely with your team during onboarding to align coding with your clinical workflows and care goals—whether you’re in an ACO, MSSP, or other VBC programs. We also run regular audits to make sure coding supports accurate reimbursements, quality scores, and compliance. With blueBriX, your coding helps you succeed in value-based care, not just fee-for-service.
Not with blueBriX. We’re built for transparency and control.
Our platform gives you real-time visibilityinto coding activity, turnaround times, accuracy rates, and compliance metrics—so you’re never in the dark. We operate with SLA-based accountability and provide detailed reports that go beyond basic productivity metrics to show you how coding impacts your revenue cycle and care outcomes.