In this blog, we’ll break down the common causes of claim denials, the effects they create, and the practical strategies to minimize them. Because at the end of the day, reducing denials is a financial necessity as well as a strategic move for long-term success.
Claim denials are a persistent and costly pain point in healthcare, significantly impacting both financial stability and patient satisfaction. Despite advancements in technology and sophisticated data analytics, many practices continue to grapple with stubbornly high denial rates. Consider the financial weight of this issue: industry benchmarks reveal that, on average, 5-10% of all submitted healthcare claims are denied initially, translating to billions of dollars in potentially lost revenue annually for the U.S. healthcare system alone. These high denial rates necessitate extensive rework, place significant strain on already stretched administrative resources (with the average cost to rework a single denied claim estimated between $25 and $118), and lead to protracted payment cycles – all of which can severely undermine operational efficiency and, ultimately, negatively affect patient outcomes.
It’s not merely about lost revenue; it’s about proactively protecting your bottom line, safeguarding patient trust in the billing process (as studies indicate that billing errors and denials are a leading cause of patient dissatisfaction), and sustaining a healthy and predictable cash flow, which is increasingly critical in an evolving value-driven market where financial performance is directly linked to quality of care and patient experience.
Reasons Behind Claim Denials

They can stem from errors in the initial claim submission, issues related to patient eligibility and coverage, lack of medical necessity documentation, coding inaccuracies, and a host of payer-specific rules and regulations.
-
Errors in Claim Submission
- Simple errors such as misspelled names, incorrect dates of birth, inaccurate insurance identification numbers, or missing demographic details
- Incorrect, outdated, or missing codes
- Failure to obtain the prior approval before rendering the service
- Submitting the same claim multiple times, even unintentionally
-
Issues Related to Patient Eligibility and Coverage
- Lapsed, terminated, or inactive insurance coverage at the time of service
- Care provided by an out-of-network provider
- Policy limitations or exclusions for specific services, procedures, or medications
- Errors in coordinating benefits for patients with multiple insurance policies
-
Lack of Medical Necessity Documentation
- Insufficient detail in the medical record to support the diagnosis and treatment
- Documentation does not clearly link the diagnosis to the services provided
- Medical necessity criteria not aligned with payer-specific guidelines
-
Coding Inaccuracies
- Assigning codes that do not accurately reflect the complexity or level of service provided
- Billing separately for services that should be bundled together under a single comprehensive code
- Using incorrect or missing modifiers
How Denial Management Drives Success in Healthcare
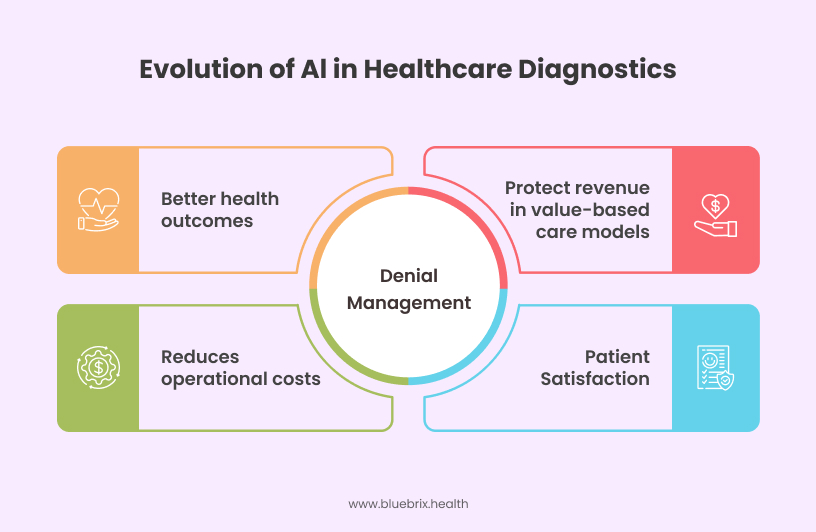
Effective denial management is a strategy that directly impacts the financial viability of healthcare organizations and their ability to deliver high-quality patient care. The importance of denial management is amplified by several key trends:
- The Shift Towards Value-Based Care: In the value-based care paradigm, revenue is increasingly tied to achieving specific quality metrics and managing costs effectively. High denial rates directly undermine these goals by reducing revenue and increasing administrative overhead, making it harder to invest in initiatives that improve health outcomes and patient satisfaction.
- The Growing Emphasis on Patient Satisfaction: Claim denials can be a significant source of frustration and anxiety for patients, leading to dissatisfaction with their healthcare experience. Patients who receive surprise medical bills may lose trust in their providers and the healthcare system. Effective denial management, including transparent communication and proactive resolution of issues, contributes directly to improved patient satisfaction.
- Cost Reduction in Healthcare: In an environment where cost containment is a paramount concern, the administrative burden and financial losses associated with claim denials are simply unsustainable. Efficient denial management strategies contribute directly to cost reduction in healthcare by minimizing rework, maximizing revenue capture, and freeing up resources for patient care.
- Improved Health Outcomes: By ensuring financial stability, healthcare organizations can invest in better technology, staff training, and patient education programs, all of which can positively impact the quality of care delivered and ultimately lead to better patient outcomes. Also, by reducing administrative burdens on clinicians, they can spend more time focusing on direct patient care.
Strategies for Effective Denial Management
Implementing a reliable denial management strategy requires a multi-faceted approach that encompasses proactive prevention, efficient identification, timely analysis, and rigorous follow-up. It’s not just about appealing denied claims; it’s about building processes and leveraging technology to minimize denials in the first place.
1. Proactive Prevention
The most effective way to manage denials is to prevent them from occurring in the first place. This requires a strong focus on front-end processes and staff training:
- Enhanced Patient Registration and Eligibility Verification: Implement processes for accurately capturing patient demographic and insurance information at the point of registration. Utilize electronic eligibility verification tools to confirm coverage in real-time and identify potential issues proactively.
- Comprehensive Pre-Authorization and Pre-Certification Processes: Establish clear workflows for identifying services that require prior authorization and ensure that these authorizations are obtained before the service is rendered. Utilize technology to track authorization requirements and deadlines.
- Strong Clinical Documentation Improvement (CDI) Programs: Implement CDI programs that focus on ensuring the medical record accurately and completely reflects the patient’s condition, the services provided, and the medical necessity for those services.
- Accurate Coding Practices: Invest in certified and experienced coding professionals and provide them with ongoing training on the latest coding guidelines and updates. Implement coding audits to identify and correct potential errors before claims are submitted.
- Regular Communication and Collaboration with Payers: Establish open lines of communication with insurance payers to stay informed about their policies, procedures, and any changes in their requirements.
2. Efficient Identification and Analysis
Despite the best preventive efforts, some denials will inevitably occur. The key is to identify these denials quickly, analyze the root causes, and prioritize them for appeal:
- Timely Reconciliation of Remittance Advice and Electronic Funds Transfer Data: Implement processes for the daily or regular reconciliation of RAs and EFT data to identify denied claims promptly.
- Categorization and Tracking of Denials: Utilize billing software or dedicated denial management systems to categorize denials based on the reason code provided by the payer. Track denial trends over time to identify recurring issues and areas for improvement.
- Root Cause Analysis: For significant denial trends or high-value denials, conduct thorough root cause analyses to understand the underlying reasons.
- Prioritization of Appeals: Develop criteria for prioritizing appeals based on factors such as the dollar value of the claim, the likelihood of a successful appeal, and the impact on patient care.
3. Timely and Effective Follow-Up
Once denials are identified and analyzed, timely and effective follow-up is crucial to recovering lost revenue:
- Well-Defined Appeal Processes: Establish clear and documented appeal processes that comply with payer-specific requirements and deadlines. Ensure that appeals are supported by comprehensive documentation, including relevant medical records, coding justifications, and explanations addressing the payer’s reason for denial.
- Electronic Claim Appeals: Utilize electronic claim appeal submission methods whenever possible to streamline the process and improve efficiency.
- Persistence and Follow-Through: Track the status of all submitted appeals and follow up with payers as needed to ensure timely resolution.
- Regular Review of Appeal Outcomes: Analyze the outcomes of appeals to identify trends in payer behavior and refine internal processes accordingly.
The Power of Purpose-Built EHRs in Denial Management
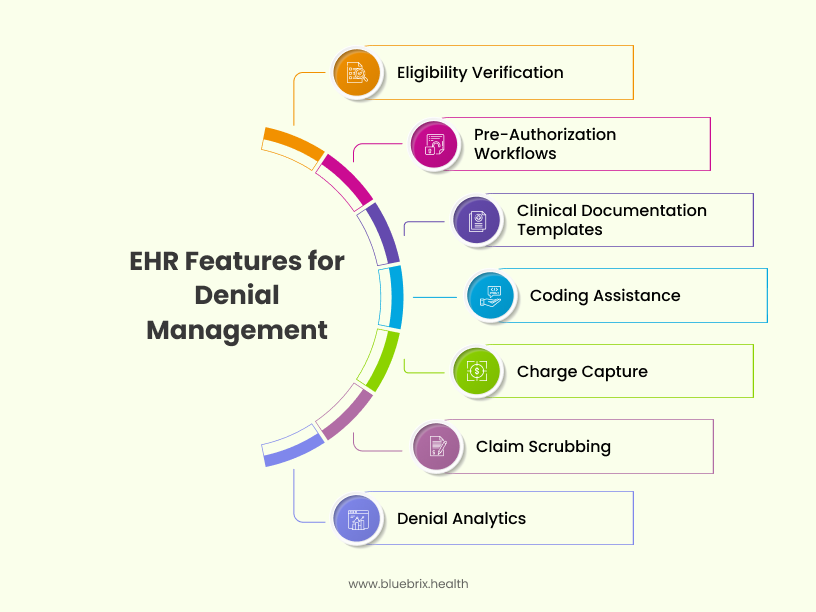
While a dedicated denial management system can be invaluable, a purpose-built EHR plays a crucial role in preventing denials and streamlining the entire denial management process. Unlike generic EHRs, those designed with denial management in mind offer features and functionalities that can significantly enhance revenue cycle management:
- Integrated Eligibility Verification: Seamless integration with payer systems allows for real-time eligibility checks directly within the EHR workflow, preventing claims from being submitted for ineligible patients.
- Pre-Authorization Workflows and Tracking: The EHR can incorporate workflows that guide users through the pre-authorization process, track authorization status, and alert staff to expiring authorizations.
- Clinical Documentation Templates and Prompts: Purpose-built EHRs can include documentation templates and prompts that guide clinicians in capturing the necessary information to support medical necessity and accurate coding.
- Coding Assistance and Validation: Some purpose built EHRs offer integrated coding tools that provide suggestions, flag potential coding errors, and ensure compliance with coding guidelines.
- Automated Denial Flagging: Intelligent EHR systems can automatically flag high-risk claims based on predefined triggers, reducing the manual effort required to identify potential denials.
- Denial Reason Mapping: Advanced denial management tools map specific denial reasons to root causes, helping organizations target the most impactful corrective actions and reduce future denials.
- Integrated Work Queues: Purpose-built EHRs offer integrated work queues that streamline denial follow-up by grouping related tasks and improving visibility for revenue cycle teams.
- Appeal Management Tools: Automated appeal management tools guide users through the appeals process, including drafting, submitting, and tracking appeals to reduce administrative burden and improve recovery rates.
- Real-Time Alerts & Dashboards: Real-time alerts and performance dashboards provide instant insights into denial trends, helping organizations quickly identify and address revenue cycle issues.
- Payer-Specific Rules Engine: An integrated rules engine allows organizations to apply payer-specific guidelines, reducing the risk of avoidable denials and ensuring claims are correctly processed the first time.
- Charge Capture and Reconciliation Tools: Integrated charge capture functionalities ensure that all billable services are accurately recorded and linked to the corresponding clinical documentation. Reconciliation tools help identify discrepancies between documented services and billed charges.
- Real-time Claim Scrubbing: Before claims are submitted, the EHR can perform automated checks (claim scrubbing) to identify potential errors and inconsistencies that are likely to result in denials.
- Denial Analytics and Reporting: A purpose-built EHR can provide reliable reporting and analytics capabilities that allow organizations to track denial rates, identify the most common reasons for denials, and monitor the effectiveness of their denial management efforts.
Conclusion: Charting a Course Towards Financial and Clinical Health
Claim denials are a significant challenge in the healthcare industry, impacting financial stability, administrative efficiency, patient satisfaction, and the overall cost of healthcare. In the era of value-based care, preventing claim denials is not just a financial imperative; it’s a fundamental aspect of delivering high-quality, cost-effective care that prioritizes positive patient outcomes and responsible resource utilization. Beyond delaying payments, denials disrupt the data continuity required for accurate risk scoring, quality measurement, and shared savings tracking—key pillars of value-based reimbursement.
By embracing a culture of accuracy, efficiency, collaboration, and a strong focus on the cost factor, we can move towards a healthcare system where “denied” becomes the exception, not the rule, ultimately benefiting all stakeholders and paving the way for a truly value-driven and financially sustainable future. Take the first step toward fewer denials. Discover how blueBriX can streamline your revenue cycle, reduce denials, and improve financial performance. Contact us today.