Managing a chronic condition shouldn’t feel like a constant battle. Yet, without the right support, small health issues can quickly spiral into hospital visits. That’s where Chronic Care Management steps in—helping patients stay on top of their health with proactive care, personalized support, and better coordination between providers. So, how exactly does chronic care management reduce hospitalizations? Read the full blog here!

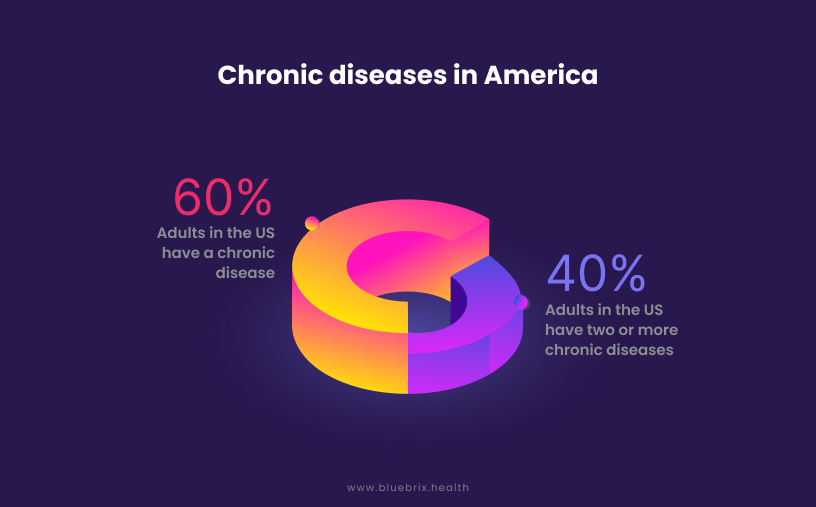
Hospital readmissions pose a significant challenge to healthcare systems, impacting both patient outcomes and financial stability. Chronic diseases, including diabetes, heart disease, and chronic obstructive pulmonary disease (COPD), primarily contribute to these frequent readmissions. In 2018, there were approximately 3.8 million readmissions in the U.S., costing an average of $15,200 per readmission. Heart failure and COPD were among the leading causes of these readmissions. The burden of unplanned hospital returns not only strains resources but also reflects potential gaps in patient care continuity.
Chronic Care Management (CCM) programs offer a promising solution by facilitating ongoing, coordinated care for individuals with chronic conditions. By fostering regular communication, proactive monitoring, and personalized care plans, chronic care management aligns seamlessly with the principles of value-based care. It emphasizes improved health outcomes, reduced hospital utilization, and cost efficiency, creating a framework where healthcare providers and systems can prioritize quality over quantity. This blog delves into the vital role of chronic care management in mitigating readmissions and highlights its benefits for both patients and healthcare providers.
What is Chronic Care Management?
Chronic Care Management refers to a comprehensive care coordination service provided to patients with two or more chronic conditions. These conditions are expected to last at least 12 months (or until the patient’s death). This model emphasizes the development of a comprehensive care plan that details treatment goals, medications, and management strategies tailored to each patient’s unique needs. A cornerstone of chronic care management is the continuous coordination among healthcare providers—including doctors, nurses, and specialists—to ensure consistent and holistic care.
Critical to this approach is ongoing health monitoring through regular check-ins and Remote Patient Monitoring (RPM), which allows for proactive interventions. By addressing gaps in post-discharge care, chronic care management effectively minimizes hospital readmissions through proactive care coordination and seamless communication among providers. The use of personalized care plans and remote monitoring—reimbursed under Medicare CPT codes—enables consistent oversight that not only reduces the risk of hospital readmissions but also enhances overall well-being while lowering healthcare costs.
Chronic Care Management exemplifies a shift from episodic treatment to proactive, continuous care, redefining the patient-provider relationship to prioritize value-driven, holistic care, over reactive interventions.
How does Chronic Care Management help reduce Hospital Readmissions?
Patients respond differently to care services, with factors such as immunity and chronic condition severity influencing outcomes. While hospital readmissions remain a persistent challenge, chronic care management programs help identify at-risk patients and implement targeted strategies to enhance health outcomes. Here’s how chronic care management programs can drive this impact:
Risk Stratification
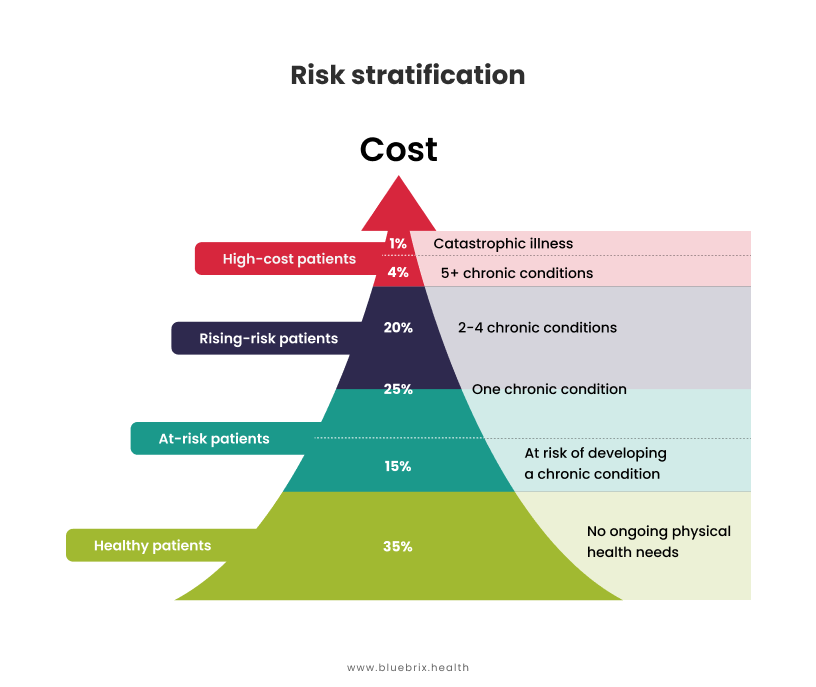
Chronic Care Management plays a critical role in risk stratification and population health by identifying high-risk patients more likely to experience hospital readmissions. Digital health tools with advanced analytics and predictive modeling help monitor patient data in real-time, flag potential health deteriorations, and facilitate timely interventions. Personalized treatment plans, coordinated follow-ups, and medication adherence through Chronic Care Management programs help address the root causes of readmissions and enable providers to take preventive measures.
Medication Management, Adherence, & Patient Education
Chronic Care Management programs enhance transparency and accuracy in care delivery by meticulously capturing and analyzing patient data. These insights enable better decision-making for medication management and adherence tracking. Proactive interventions prevent escalations, reduce comorbidities and hospital readmissions. Medication adherence and patient education significantly reduce hospital readmissions and improve overall health outcomes.
Personalized Care Plans
Chronic Care Management programs require healthcare providers to gain a comprehensive view of a patient’s health history. An integrated Electronic Health Record (EHR) system enables providers to gain a comprehensive view of the patient’s health and create personalized care plans tailored to individual needs. Digital health solutions with predefined templates that can be customized, will help manage personalized care plans that are both effective and responsive to unique patient requirements. By addressing specific requirements, providers can improve adherence and reduce the likelihood of readmissions.
Seamless Care & Coordination
Technology solutions enable patient-centered chronic care management by enhancing communication and collaboration among care team members. Seamless integration ensures all providers are aligned in their approach, resulting in effective decision-making based on accurate, up-to-date data. This collaborative framework significantly reduces hospital readmissions by ensuring personalized, well-coordinated care that meets individual patient needs.
Timely Interventions & Remote Monitoring
With remote patient monitoring capabilities, Chronic Care Management programs allow healthcare providers to access real-time patient data and customize alerts for timely interventions. For example, notifications can be triggered when a patient’s vitals exceed predetermined thresholds, enabling providers to adjust care plans proactively. This capability has demonstrated a significant reduction in hospital readmissions by addressing potential issues before they escalate. Moreover, research indicates that patients who actively engaged with RPM were less likely to return to the emergency department within 90 days compared to those who did not participate in RPM programs (19.8% vs. 23.6%)—demonstrating the potential for remote patient monitoring to enhance continuity of care and reduce acute care utilization.
Proactive Care Beyond the Clinical Setting
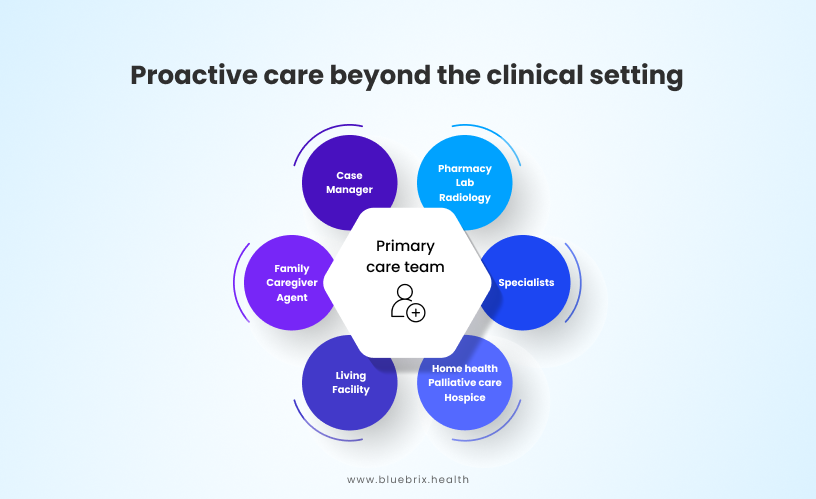
Chronic Care Management programs represent a shift from reactive to proactive care, emphasizing intervention before crises occur. Providers can leverage Chronic Care Management programs to monitor patient health trends in real-time and address concerns before they escalate into emergencies. By extending care into patients’ daily lives—through Remote Patient Monitoring and addressing Social Determinants of Health (SDOH)—Chronic Care Management programs empower providers to deliver holistic care that reduces hospitalizations. This approach reframes the provider’s role from a problem-solver to a health partner, reinforcing trust and long-term engagement.
Healthcare providers can leverage digital health tools to identify and address patients’ SDOH by connecting them with community resources, ultimately improving outcomes and reducing hospital readmissions.
Future Trends in Chronic Care Management to Reduce Hospital Readmission
Integrated Care Models
There is a growing trend toward integrated care models that facilitate collaboration among various healthcare providers, including primary care physicians, specialists, and community health workers. This coordinated approach helps ensure seamless transitions between care settings and reduces the likelihood of readmissions due to miscommunication or lack of follow-up care.
Addressing Social Determinants of Health
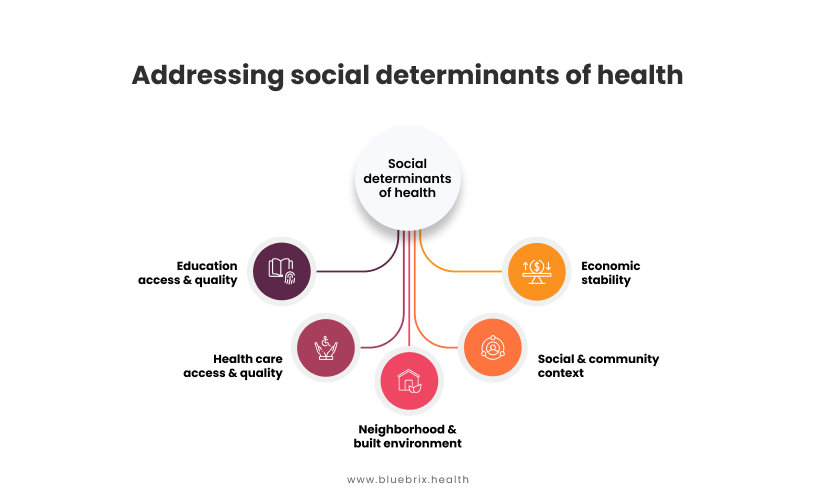
Recognizing the impact of social determinants on health outcomes is critical. Future Chronic Care Management initiatives will increasingly incorporate assessments of social factors such as housing stability, transportation access, and food security into care planning. By addressing these issues proactively, healthcare providers can help mitigate risks that contribute to hospital readmissions.
Data Analytics and Predictive Modeling
Advanced data analytics and predictive modeling techniques will be utilized to identify high-risk patients more effectively. By analyzing historical data and real-time patient information, healthcare organizations can implement targeted interventions for those most likely to experience readmissions.
Patient Engagement Tools
Empowering patients through engagement tools—such as mobile apps that track symptoms, medication adherence, and appointment reminders—will be crucial for improving self-management skills. Enhanced patient engagement leads to better health literacy and ownership of their health journey, which can significantly reduce readmission rates.
Focus on Transitional Care Management
As part of efforts to improve discharge processes, transitional care management programs will continue to evolve. These programs aim to provide comprehensive support during the transition from hospital to home or other care settings, ensuring that patients receive appropriate follow-up care and resources.
By embracing these trends in Chronic Care Management, healthcare providers can create a more proactive approach to patient care that not only reduces hospital readmissions but also enhances overall health outcomes for individuals with chronic conditions.
Final Take
By strategically implementing Chronic Care Management programs, healthcare providers can enhance patient care, reduce costs, and effectively manage resources, particularly in addressing the rise in hospital readmissions among chronically ill patients. As the industry shifts towards value-based care, care management solutions like blueBriX enable the creation of tailored care models aligned with operational goals. Embracing these innovative solutions fosters improved patient outcomes, optimizes resource utilization, and positions providers for success in a dynamic, value-driven healthcare landscape.