Healthcare is fueled by clinical documentation, but nearly 80% of that critical intelligence remains locked in unstructured narrative text. When a high-risk patient deteriorates, warning signs are often documented but scattered across dozens of notes, making timely review impossible. When quality measures fail, the interventions were recorded—but impossible to find without manual chart review. The intelligence is already there, but its inaccessibility renders it operationally useless.
AI, particularly Natural Language Processing (NLP) fundamentally changes this reality. It reads clinical notes like a skilled clinician automatically extracting key insights and transforming narrative text into structured, actionable data. Let’s examine how NLP transforms healthcare operations—from today’s fractured reality to what becomes possible.
The unstructured data crisis in healthcare
Physicians rely on free-text notes to capture the full depth of patient encounters—nuanced judgments, patient stories, and contextual details that structured fields can’t hold. But this data isn’t limited to EHR entries. It includes handwritten notes, voice dictations, scanned referrals, lab reports, and annotated images like wound photos or scans.
This mix of unstructured and semi-structured formats creates a core problem: critical insight-like symptoms, diagnoses, treatment responses; care gaps are buried in narrative rich text with no standardized way to extract them.
And the downside is that key information that resides between many pages, unavailable for real-time decision support, population health, quality reporting, or regulatory needs. This drives inefficiency, delays interventions, and hinders measurable improvement in care. Until advanced tools can reliably unlock these sources, clinical intelligence remains hidden in plain sight.
Let’s examine the impact across four critical areas:
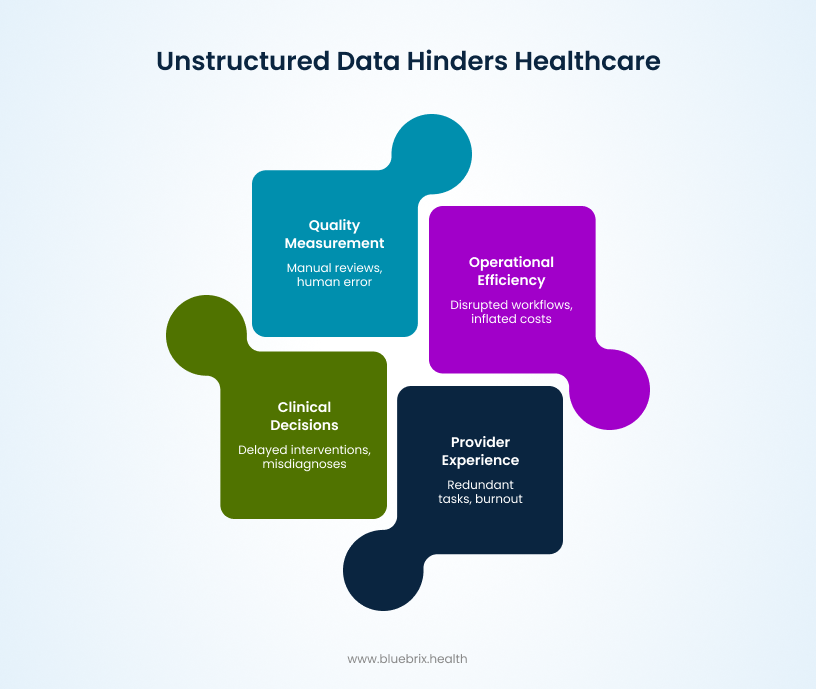
On clinical decision-making
When you need to find symptoms buried in piles of clinical notes, the manual search is tedious and time-consuming. This delays critical interventions and increases the risk of missing key information, leading to misdiagnoses or suboptimal care. Poor data quality from unstructured sources directly harms patient outcomes and impairs clinical decisions, forcing clinicians to struggle with incomplete or hard-to-access information. In fast-paced settings like emergency rooms, this gap can mean the difference between timely care and preventable complications.
On quality measurement
Assessing outcomes and compliance becomes a laborious, weeks-long ordeal of manual chart reviews to pull together data for metrics like readmission rates or treatment efficacy. Quality teams sift through unstructured notes to extract details on post-discharge progress or adverse events, a process prone to human error and inconsistency. This inefficiency hampers efforts to benchmark performance, comply with regulations, or participate in value-based care models. Without quick access to these insights, organizations miss opportunities to improve protocols, and the broader healthcare ecosystem suffers from fragmented reporting—ultimately slowing advancements in evidence-based medicine.
On operational efficiency
Daily operations grind to a halt as staff spend hours hunting through notes for specific information, such as a patient’s vaccination history or allergy details scattered across multiple entries. This scavenger hunt disrupts workflows, inflates administrative burdens, and drives up costs—think of the time lost in coordinating care across departments or preparing for audits. Unstructured data’s lack of standardization exacerbates storage and sharing challenges, making it difficult to integrate with other systems and leading to silos that prevent seamless collaboration. In an era where data volumes are exploding, this inefficiency isn’t just frustrating; it’s a financial drain, with industries recognizing unstructured data management as a hidden cost that demands strategic solutions.
On provider experience
Clinicians face a cycle of redundant frustration: they document once in detailed narratives to capture the full picture, yet must re-enter the same information into structured fields elsewhere for billing, reporting, or interoperability. And when it comes time to review, they must read everything from scratch, often across fragmented records. This redundancy contributes to burnout, with providers spending more time on paperwork than patient interaction—exacerbating shortages and turnover in an already strained workforce. The emotional toll is real, as the inability to quickly access “hidden” intelligence undermines confidence and job satisfaction, turning what should be a supportive tool into a daily adversary. Addressing this crisis isn’t optional; it’s essential for reclaiming the true potential of clinical data and empowering those on the front lines.
These fractures aren’t inevitable—they’re solvable. NLP bridges the gap between what’s documented and what’s actionable, transforming narrative chaos into clinical clarity.
What makes natural language processing an expert in clinical data extraction?
Natural Language Processing is a branch of artificial intelligence (AI) that empowers computers with the ability to understand, interpret, and generate human language, both written and spoken. It combines computer science, AI, and linguistics to process unstructured language data and perform tasks like translation, sentiment analysis, and speech recognition.
NLP achieves this through several specialized techniques that work together to unlock clinical intelligence:
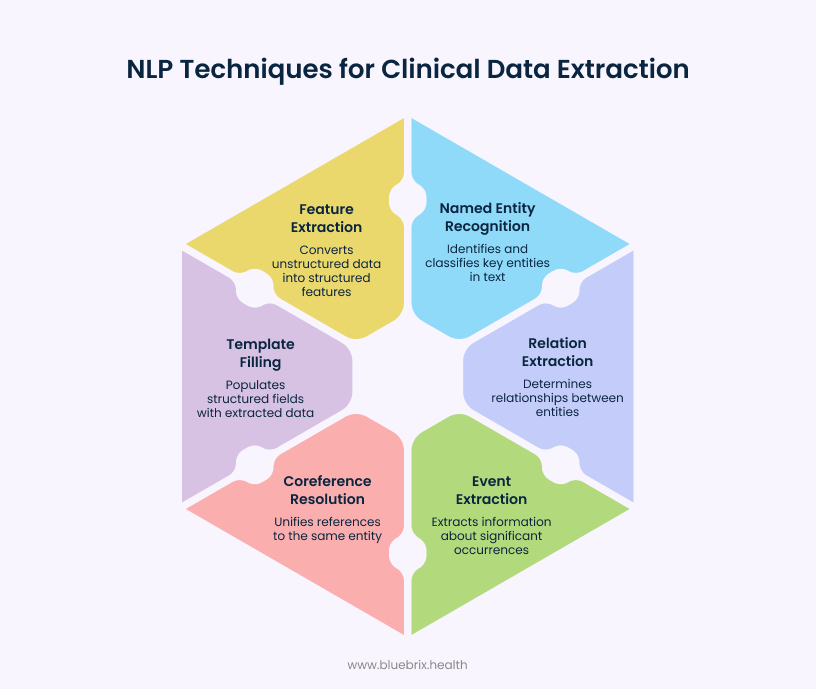
Named entity recognition
It pinpoints and classifies key entities such as names, places, dates, and organizations within large documents or datasets. This makes it possible to quickly find relevant information without manual review.
Relation extraction
Determines relationships between entities, such as identifying which doctor prescribed a medication to which patient, or linking specific medications to the conditions they’re treating. This allows deeper insights from otherwise unconnected data points.
Event extraction
Extracts information about significant occurrences documented in clinical text, such as hospital admissions, medication changes, surgical procedures, or adverse reactions. The process captures not just the event itself (e.g., “discharge,” “fall incident”), but also essential contextual details like who was involved (patient, provider), when it occurred (dates), where it happened (facility or care setting), and why (clinical indication).
Coreference resolution
Resolves pronouns or alternative mentions (e.g., “he”, “the hospital”) to unify all references to the same real-world entity, ensuring data is coherent.
Template filling and open information extraction
Automatically populates structured fields like medication names, dosages, diagnoses, and procedure dates. When a clinician writes ‘started patient on sertraline 50mg for moderate depression,’ NLP instantly extracts each element into the correct structured field, eliminating double documentation and manual errors.
Feature extraction
It translates unstructured clinical notes into structured data that machine learning algorithms can analyze. When a clinician documents patient symptoms, treatments, and diagnoses in free text, the system identifies key elements—tracking word frequency, recognizing medical concepts, and detecting clinical themes—then converts these into numerical features that reveal patterns, enable predictions, and support data-driven decision-making.
These techniques form the foundation—but how do they actually work in practice? Let’s see that.
From narrative to intelligence: real-time application of intelligence in healthcare documentation
AI-powered NLP has evolved beyond simple data extraction. Modern systems flag missing information, identify documentation gaps, and help close them in real time. This advancement directly supports more accurate coding, smoother claim processing, and improved compliance. In healthcare’s complex environment, AI-driven NLP acts as an intelligent assistant, making clinical documentation more complete, actionable, and reliable.
Let’s explore how these capabilities play out across key operational areas:
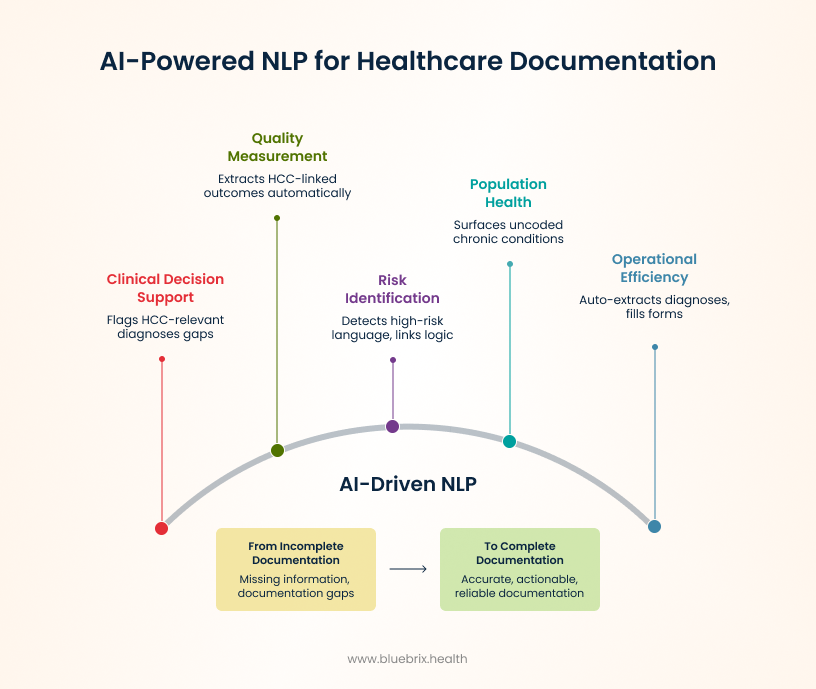
Clinical decision support & hcc coding
The challenge: Providers must ensure complex conditions are not missed, diagnoses are accurately coded, and risk-adjustable factors are thoroughly documented for optimal Risk Adjustment Factor (RAF) scoring.
NLP solution:
- Flags potential gaps in HCC-relevant diagnoses or documentation
- Suggests appropriate HCC codes based on extracted data
- Surfaces comorbidities, complications, and status changes across all encounter notes
- Prompts clinicians to complete missing elements (e.g., specificity, chronicity, linkage between conditions and treatments)
Example: If “diabetes” is written, but not whether it’s type 1 or type 2, the system will alert the user to add that missing info.
Quality measurement and reporting
The challenge: Auditing performance and outcomes against payer or regulatory requirements is painfully manual.
NLP solution:
- Extracts HCC-linked outcomes (e.g., documented improvements in chronic conditions)
- Automatically compiles risk scores and code justifications from narrative text
- Fills in gaps for accurate population-level analysis
Example: For payment integrity review, NLP finds all patients with diabetes and ensures proper linkage to complications and HCC codes, reporting compliance rates without hours of manual chart audits.
Risk identification and prevention
The challenge: Risk factors affecting RAF or outcomes aren’t consistently coded unless surfaced in real time.
NLP solution:
- Detects high-risk language (“increased falls,” “ESRD,” “insulin-dependent” etc.) and links to risk adjustment logic
- Flags unresolved or ambiguous disease status for further review
Example: Patient note mentions “new shortness of breath, congestive heart failure history”—NLP highlights as both a risk for acute events and a missed HCC opportunity unless fully documented.
Population health management
The challenge: Capturing and coding SDOH and clinical risk variation across large panels is labor-intensive.
NLP solution:
- Surfaces uncoded chronic conditions, complications, or barriers impacting risk scores
- Prioritizes patients with potential under-coded conditions for review
Example: NLP scan identifies patients reporting “food insecurity” or “dialysis,” flags for SDOH and HCC coding in care management workflow.
Operational efficiency and compliance
The challenge: Audits and payer submissions demand complete, accurate, and codified documentation.
NLP solution:
- Auto-extracts HCC-relevant diagnoses and justifications for payer packets
- Fills referral/pre-auth forms with precise coded data, cutting turnaround time
- Supports audit responses by compiling supporting text and code references automatically
Example: For a Medicare Advantage audit, NLP gathers all supporting documentation for HCC codes in minutes, reducing compliance risk and workload.

