If you talk to any care coordination leader in a US healthcare system today, they’ll tell you the same thing: managing patients is the easy part. Managing the payers and programs wrapped around those patients is what turns each day into a balancing act.
On paper, a healthcare system may look like one unified organization supporting a single population. But operationally, it behaves more like a network of parallel financial and performance frameworks, each with its own rules, exclusions, timelines, and definitions of success. A patient’s care may be continuous, but the reporting reality underneath is anything but.
To see how this plays out, imagine a single patient moving through different coverage types, shifting risk arrangements, and being attributed to various chronic care or ACO models along the way. Nothing changes clinically for the team caring for them. Yet internally, each transition resets eligibility requirements, measure definitions, submission workflows, and incentive mechanics. Multiply this by thousands of patients and dozens of contracts, and you get a system where coordinators spend a growing portion of their time proving the work they already did.
This is the real friction point. Even as value-based care adoption accelerates and regulators push for tighter care coordination standards, clinics are juggling more fragmented reporting responsibilities than ever before. And the more programs a patient is part of, the harder it becomes for teams to keep a clean, consistent narrative of what was done, why it was done, and which payer actually cares.
The result is a growing operational paradox: The better VBC organization get at coordinating care, the harder it gets to report that work accurately across payers.
That’s the landscape this blog explores. Not just the technical pain points, but the human and financial pressure behind them. And more importantly, how a unified operational intelligence layer can shift the burden off care managers and restore alignment across the entire multi payer, multi program ecosystem.
How clinics currently manage multi payer reporting and why it fails?
Most teams already have a system they’ve pieced together over years of solving problems on the fly. A note in the EHR, a spreadsheet to keep track of who counts for what, a bookmarked list of portals each payer requires, and a running mental checklist that only the coordinators truly understand. It works because the people are committed, not because the process is built well.
The strain shows the moment program volume increases. Add a few new contracts, adjust a measure definition, introduce a Medicaid requirement with a different submission cadence, and the routine that once felt stable starts to wobble. A single follow-up call suddenly needs to be interpreted three different ways, checked against separate timelines, and entered into systems that were never designed to speak to one another. Coordinators end up stitching together the reporting story manually, one patient at a time.
This is where most clinics hit a wall. The workflows weren’t designed for constant rule changes or multi program participation, so the burden shifts onto people to keep everything aligned. And people can only scale so far. What starts as small workaround habits eventually turns into a system where accuracy depends on memory, capacity, and timing luck. The result is entirely predictable: rising administrative load, uneven reporting, and financial performance that no longer reflects the quality of care being delivered.
Core multi payer reporting challenges in US clinics
If the introduction shows why reporting becomes messy, the next step is understanding where that mess begins. In most clinics, the breakdown isn’t caused by one dramatic failure. It comes from dozens of small inconsistencies that expand every time a new payer contract or disease program is added.
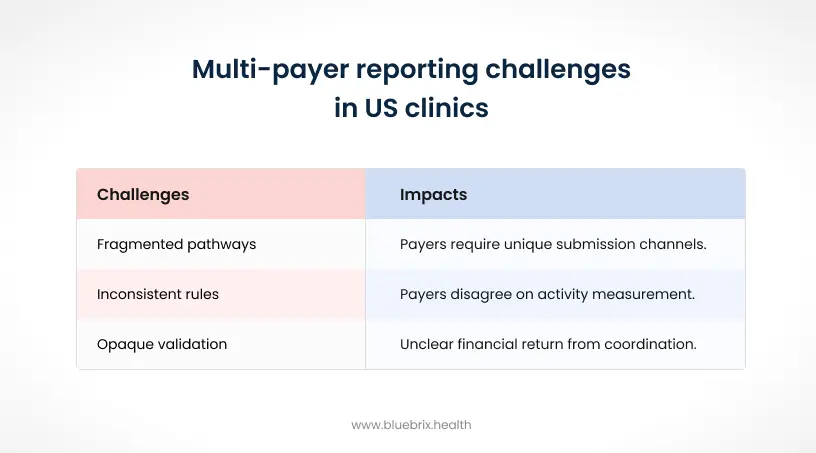
Below are the three core friction points that consistently drain coordinator time, distort program performance, and reduce the financial return provider groups expect from their value-based care strategy.
1. Inconsistent rules for mapping care activities to measures
Even when coordinators follow a single workflow, payers rarely agree on how those actions should be counted.
A simple example would be a post-discharge telehealth call. One payer may award credit for the encounter, a second may exclude telehealth entirely, and a third may only count it if medication reconciliation occurs within 48 hours. The activity is identical, but the value changes based on the contract sitting behind the patient.
In practice, this means:
- Coordinators maintain multiple documentation patterns for identical work,
- Parallel checklists emerge for ACOs, Medicaid P4P, and commercial quality programs,
- Small rule changes create ripple effects across hundreds of active patients.
Clinics have reported losing up to 15 percent of coordination time to measure-by-measure adjustments that should never be necessary in the first place.
And this is before seasonal rule updates or program renewals add more variability.
2. Fragmented submission pathways across payers and programs
Once activities are documented, another bottleneck appears:
each payer requires its own submission channel, file format, and validation process.
A large health system may need to submit:
- QPP uploads through CMS portals,
- Bundle reporting via claims extracts,
- Disease program performance data via XML uploads,
- Patient experience scores through CAHPS registries,
- State Medicaid performance packets through separate dashboards.
Each of these has unique deadlines, login structures, file schemas, and quality checks. The coordinator who just spent 20 minutes counseling a heart failure patient may spend the next 40 minutes rekeying that encounter into a different submission tool.
Across multi-program clinics, this easily consumes a significant share of coordinator FTE time, turning clinical navigators into part-time data entry specialists.
3. Opaque performance validation and unpredictable true-ups
Even when coordinators do everything right, clinics often struggle to determine the financial return from those efforts.
Why? Because each payer uses different attribution methods, savings models, risk corridors, and reconciliation calendars. One program may finalize results quarterly. Another may true-up 18 months later. Yet the coordinator workload feeding those calculations is essentially the same.
This creates several issues:
- Provider organizations can’t see, in real time, whether coordination work is improving performance.
- Internal dashboards rarely match payer reports, creating distrust and confusion.
- Incentive dollars shrink when programs offset each other during reconciliation.
Health systems estimate that 10 to 25 percent of potential VBC incentives disappear in this opacity, not because the care wasn’t delivered, but because proof of that care couldn’t be aligned across payers.
If these challenges feel interconnected, it’s because they are. Documentation inconsistency fuels submission complexity. Submission complexity fuels performance ambiguity. And the cycle repeats until care coordination becomes more about surviving the process than improving patient outcomes.
Next, we’ll walk through how provider organizations break this cycle with unified operational intelligence.
Why is reporting complexity rising now?
By now, most VBC organization expect reporting complexity. Several regulatory, financial, and workforce forces have converged at the same moment, making coordination reporting harder than at any time in the past decade. Even organizations with mature VBC teams are feeling the strain.
Below are the four shifts reshaping the landscape.
CMS model expansions add more coordination-heavy requirements
The newest iterations of TEAM bundles and ACO REACH place far more emphasis on post-acute follow-ups, medication reconciliation, SDOH documentation, and transitional care planning. These models were designed to promote multi payer alignment, but each payer still applies its own exclusions and timing rules.
The result:
- VBC organization must track more measures per patient,
- coordinators must document more granular detail,
- programs increasingly overlap and conflict.
APCM 2025 pushes more reimbursement weight onto coordinator-driven workflows
The Advanced Primary Care Management model ties reimbursement directly to care coordination tasks such as chronic care management, transition monitoring, behavioral health outreach, and patient engagement.
However, payers still require program-specific submission workflows, meaning provider groups must:
- document once,
- transform documentation multiple times,
- validate performance in different portals.
During a period of national workforce shortages, these expectations force VBC organization to choose between hiring more coordinators or improving systems. Not surprisingly, 70 percent of provider groups now rank coordination reporting as their highest FHIR automation priority.
State Medicaid programs introduce more variability, not less
More than 35 states now operate Medicaid VBC programs claiming alignment with federal models. But in practice, each:
- uses different reporting portals,
- enforces different data schemas,
- applies unique timing thresholds,
- maintains independent attribution logic.
This misalignment is particularly painful for multi-site health systems spanning multiple states. One coastal network saw the same hypertension outreach measure translated into three different definitions across its Medicaid contracts. As a result, they lost 15 to 25 percent of potential incentive dollars simply because reporting cadence didn’t match federal timelines.
Workforce strain meets growing VBC participation
Care coordinator burnout now exceeds 40 percent, with documentation and submission work cited as the leading cause. At the same time, nearly 60 percent of clinics participate in three or more VBC contracts, and many are layering on disease programs to improve population outcomes.
But scaling programs without improving reporting infrastructure creates a widening operational gap:
- More patients in programs,
- More coordinators required,
- More portals and uploads,
- Fewer hours spent in actual patient-facing work.
It’s a cycle that becomes unsustainable without automation and unified systems.
As all these forces collide, VBC organization recognize that the old approach of “more spreadsheets, more meetings, more checklists” won’t survive. The environment now demands an operational intelligence layer that reduces fragmentation and restores clarity.
Next, we’ll shift from the external pressures to a more strategic point of view: what this complexity means for the future of care delivery and how VBC organization can reposition technology as an enabler, not just a compliance requirement.
Solutions for multi program reporting complexity
If the biggest reporting problems come from fragmentation, the solutions come from creating a single operational source of truth. The most successful clinics are the ones replacing parallel processes with unified systems that document once and report everywhere, regardless of the payer or program behind the patient.
Before looking at what that unified model enables, it’s important to understand the point where most provider groups begin to feel their existing workflows pulling apart. As programs expand, provider groups eventually reach a point where the old way of managing reporting just can’t keep pace. Each new contract introduces a different set of timelines, exclusions, and data schemas, and the manual routines that once felt workable start creating more friction than clarity. Coordinators spend more time translating requirements than supporting patients, and leaders struggle to understand why performance swings even when clinical workflows stay consistent.
The real problem isn’t the team or the effort. It’s that the reporting foundation underneath them was never built for this level of payer variation or program overlap. When the system can’t keep up, people absorb the complexity, and that’s what unified intelligence is designed to reverse. This is where the shift toward a unified operational model begins: not by adding more steps or adjusting documentation habits, but by redesigning the system so the complexity stays inside the workflow engine instead of landing on coordinators.
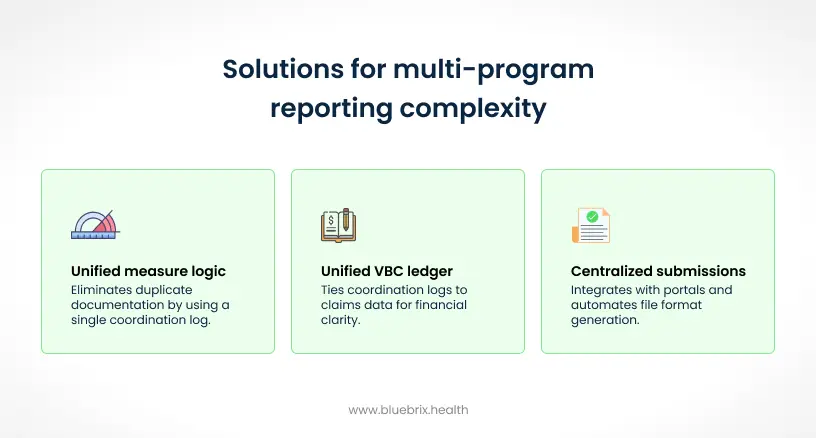
Below are the three solution pillars that consistently reduce coordinator load and recover significant value-based incentives.
1. Unified measure logic that removes duplicate documentation
The first step is eliminating the need for coordinators to document the same activity in multiple ways. A unified coordination log allows the team to record one action and let the system decide how it maps across ACOs, Medicaid programs, bundles, and P4P metrics.
How it works in practice:
- A multi-payer rules engine automatically interprets care activities against payer-specific exclusions or requirements.
- Capture outreach, follow-ups, telehealth, education, and reconciliation tasks in a single workflow.
- Coordinators see, in real time, which programs will count the activity before they complete documentation.
Consider a real scenario: A VBC organization’s COPD program requires 7-day post-discharge calls; its Medicaid contract requires 14-day follow-ups; its cardiac bundle excludes telehealth encounters entirely. With unified measure logic, one documented outreach attempt is evaluated against all three sets of rules instantly, without extra effort from the coordinator.
Impact: The VBC organization typically reclaim 50 to 70 percent of abstraction time and redirect 15 percent of coordinator hours back to high-risk patient management.
2. Centralized submissions that replace multiple portals and formats
Once activities are mapped correctly, the next burden to eliminate is the maze of submission channels.
A centralized submission hub integrates with all required portals and automatically generates the correct file formats (CSV, EDI, XML) from the same unified dataset.
Key capabilities include:
- Pre-built connectors to QPP, bundle claim portals, CAHPS registries, and state Medicaid dashboards.
- Automated validation that detects schema mismatches or missing fields before submission.
- A consolidated deadline calendar that alerts teams across programs and payers.
- Single-sign-on access spanning major commercial and government payers.
Here’s where complexity becomes real: One regional health system had 14 active value-based agreements across Medicare, Medicaid, and three commercial payers. Before centralization, they submitted 40+ files per quarter, each with unique formats and timelines. After implementing a unified submission engine, the same reporting effort dropped to 12 automated runs, with coordinators only reviewing exceptions.
Impact: This reduces administrative drain by 70 to 80 percent, while nearly eliminating rekeying errors and penalty risks.
3. A unified VBC ledger that finally clarifies ROI
Even after documentation and submission are fixed, provider groups still need a clear financial picture. That’s where a unified VBC ledger becomes essential.
The ledger ties coordination activity logs to claims data and models payer-specific attribution, risk corridors, and retroactive reconciliations.
What it enables:
- Predictive true-up simulations that forecast how different programs will offset each other.
- Drill-down analytics that show which coordinator actions directly improved performance.
- Automated reconciliation based on eligibility feeds, remits, and updated payer files.
For example: A health system participating in a Medicare ACO, a hypertension collaborative, and a surgical bundle saw three different savings calculations arrive months apart. The bundle’s penalty partially canceled out ACO gains, but the hypertension program’s achievements were never credited because documentation was mismatched during audit. After moving to a unified ledger, the team could model these interactions ahead of time and adjust workflows, preventing a six-figure revenue loss the following year.
Impact: Clinics accelerate incentive realization by 6 to 12 months and recover 20 to 30 percent of lost VBC revenue previously tied up in reconciliation errors.
When these three pillars work together, care coordination stops being a reactive reporting function and becomes a proactive, financially aligned engine for patient-centered care.
Next, we’ll look at why VBC organization feel the pressure more now than ever.
How should provider groups rethink multi payer and multi program reporting beyond compliance?
At some point, every health system reaches the same realization: reporting is not just an administrative function. It’s the operational backbone that determines whether a coordination program delivers value or drains it. And in a multi payer, multi program world, the technology decisions leaders make today shape their financial and clinical performance for years to come.
The shift VBC organization need to make is subtle but transformative. Instead of treating reporting as the last step in the process, they must redesign their workflows so reporting is simply a byproduct of good coordination, not a separate workload.
Here’s what that mindset change looks like in practice.
1. Move from documenting work to orchestrating work
Traditional workflows force coordinators to log activities, adjust documentation for each payer, and then retroactively push that information into reporting systems. But mature VBC organizations flip this model. They build systems where:
- Documentation happens once,
- Mapping is automated,
- Reporting happens in the background,
- Coordinators focus on care, not compliance.
In this model, reporting accuracy improves not because staff try harder, but because the workflow is architected correctly from the start.
2. Re-center reporting around the patient, not the program
In multi program environments, patients often belong to several disease programs, ACOs, bundles, or risk arrangements at the same time. When reporting is structured program by program, each visit generates:
- Duplicate documentation,
- Duplicate performance checks,
- Duplicate submissions.
But if the workflow starts with a single longitudinal patient record, programs simply become “lenses” applied on top of one unified story. When data is patient-centered, reporting becomes additive instead of duplicative.
3. Treat operational intelligence as essential infrastructure
Clinics often view VBC technology as optional, something to add after programs are already in motion. But the volume and variability of multi payer requirements make operational intelligence a prerequisite, not a luxury.
This includes:
- Real-time measure mapping,
- Unified activity logs,
- Submission automation,
- Predictive ROI modeling,
- Payer reconciliation feeds.
When these pieces work together, leaders gain a transparent view of performance across programs, eliminating the guesswork that previously led to delayed payments or lost incentives.
4. Focus on staff relief as a strategic priority
Many health systems still underestimate the role coordinator burnout plays in declining performance. A VBC organization can have sophisticated payer contracts and strong clinical teams, but if coordinators are drowning in reporting work, programs stall.
A technology investment that removes even 20 percent of administrative load can translate directly into:
- Better patient outreach,
- Higher follow-up rates,
- Fewer avoidable admissions,
- Faster incentive capture.
The fastest-improving systems are the ones treating staff capacity as a financial asset, not just a scheduling problem.
As provider groups adopt this new mindset, reporting transitions from an obstacle to an accelerator. The fragmented ecosystem begins to feel manageable, and care teams finally get the breathing room to focus on patients instead of portals.
Re-centering care on the patient
Multi payer and multi program ecosystems aren’t getting simpler. Every year introduces new models, new incentives, new exclusions, and new pathways that coordinators must navigate. Yet provider groups can’t afford to let this growing complexity distract their teams from what they do best: guiding patients through care.
The systems that thrive will be the ones that redesign their operations so reporting is no longer a burden but a built-in output of well-orchestrated workflows. When documentation is unified, submissions are automated, and financial outcomes are transparent, the coordination team becomes more effective, not more overloaded.
And that’s the shift blueBriX enables. By giving VBC organization a unified performance engine that connects care activities, measure logic, submissions, and ROI modeling, it replaces operational fragmentation with clarity. Coordinators get time back. Leaders get visibility. Patients get better continuity of care.




