The leadership challenge in a multi-program behavioral health network (BHN) isn’t delivering world-class care; you’ve already mastered that. Your clinical teams are saving lives in detox units, stabilizing families in outpatient clinics, and providing critical support in residential facilities every day.
The true operational hurdle that keeps COOs and Compliance Directors awake at 2:00 AM is transforming that exceptional care into compliant, reimbursable data while navigating a patchwork of regulatory mandates that seem to change with the wind.
For executives and decision-makers, the landscape has fundamentally shifted under your feet. We are no longer in the era of check-the-box compliance. With the onset of mandatory CMS Core Set reporting, the technical demands of the ONC’s HTI-2 proposed rule, and the rise of Value-Based Care (VBC) contracts, the old playbook of manual spreadsheets and reactive cleanup projects is now a liability.
Consider the sheer volume of data logistics required just to keep the lights on:
- California providers are wrestling with the Member Information File (MIF) exchanges for CalAIM.
- Texas CCBHCs are calculating time-to-evaluation down to the hour.
- Indiana networks are facing new Social Determinants of Health (SDOH) mandates from DARMHA for SFY 2026.
Moving from a reactive, checklist-driven culture to a proactive, automation-driven architecture is the strategic difference between survival and scalable growth in 2026.
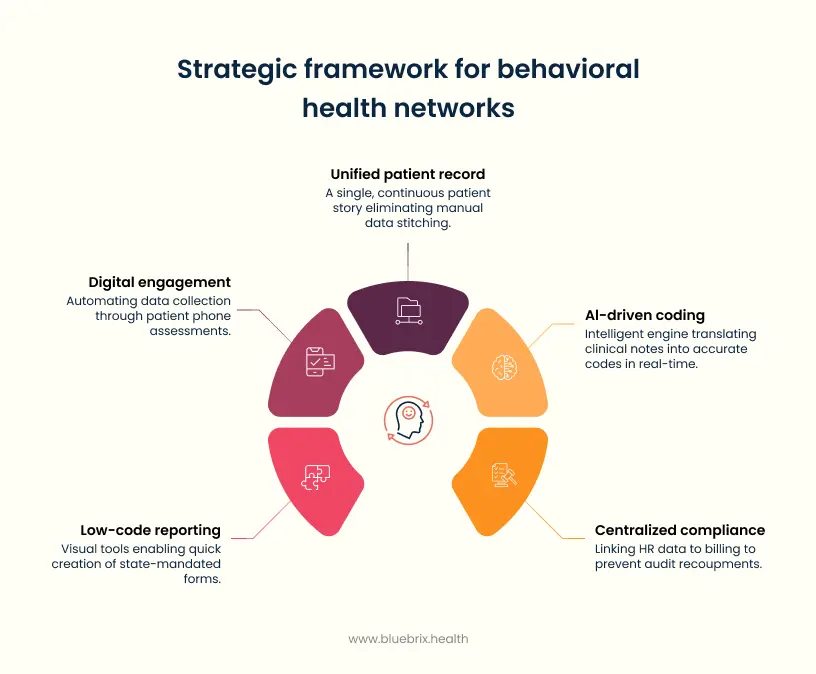
Here are five strategic pillars that move multi-program BHNs beyond simple reporting toward audit-proof operational efficiency, leveraging technology built for the new era of whole-person care.
Pillar 1: Migrating from siloed program data to a longitudinal patient ecosystem
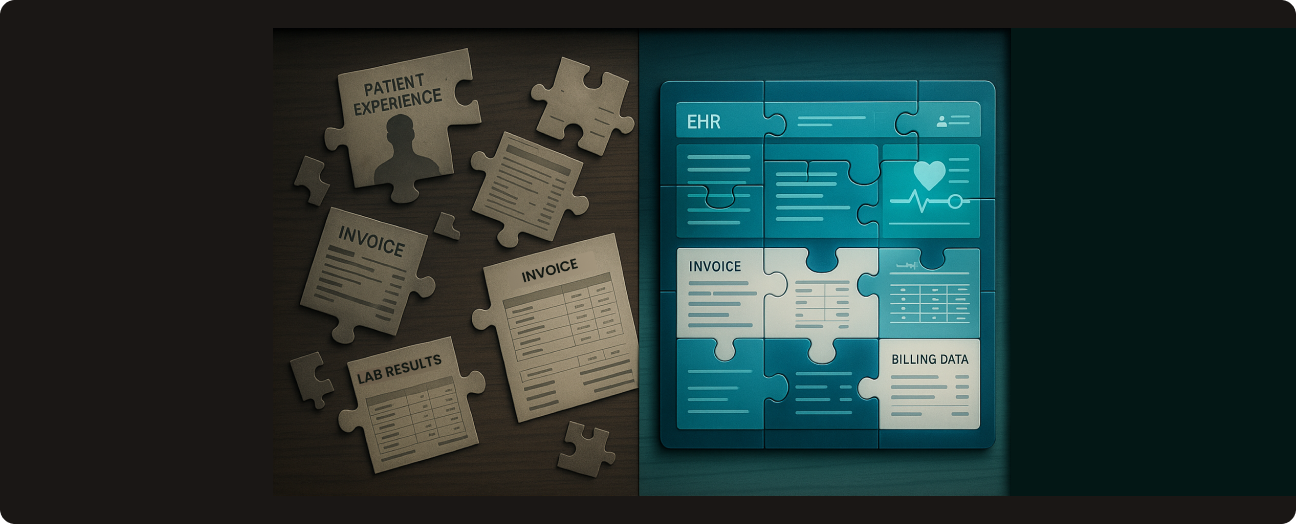
The original sin of behavioral health data is fragmentation.
In a typical multi-program network, the Patient Journey is often an administrative fiction. A patient, let’s call her Sarah, enters your ecosystem through a Crisis Stabilization Unit (CSU). Two weeks later, she steps down to a Residential Substance Use Disorder (SUD) program. Six months later, she is managed by your Outpatient Mental Health clinic.
In most legacy systems, Sarah exists as three distinct people in three separate databases. This fragmentation makes accurate reporting on readmission rates or total cost of care impossible without manual spreadsheet surgery.
The operational nightmare: the CalAIM example
Nowhere is this pain more acute than in California’s CalAIM Enhanced Care Management (ECM) program. To participate, you must engage in complex, bi-directional data exchange. You receive a patient assignment file and must return a detailed report of every outreach attempt—rounded to the minute and categorized by modality.
If your Outreach Team uses a different software than your Clinical Team, your staff is manually tallying minutes to populate the state report. This is slow, expensive, and error-prone.
The strategic imperative: the unified patient record
The modern digital health platform must eliminate the administrative concept of program-level data in favor of the unified, longitudinal patient record.
The blueBriX approach
Imagine a system where Sarah’s Outreach Attempts are captured automatically by the scheduler. The system tags these events with the correct CalAIM service codes. When the reporting deadline arrives, the platform automatically aggregates these events, formats them into the state-mandated file, and readies it for transmission. No spreadsheets. No manual tallying.
Pillar 2: Implementing a dynamic, rules-based clinical-to-regulatory code engine
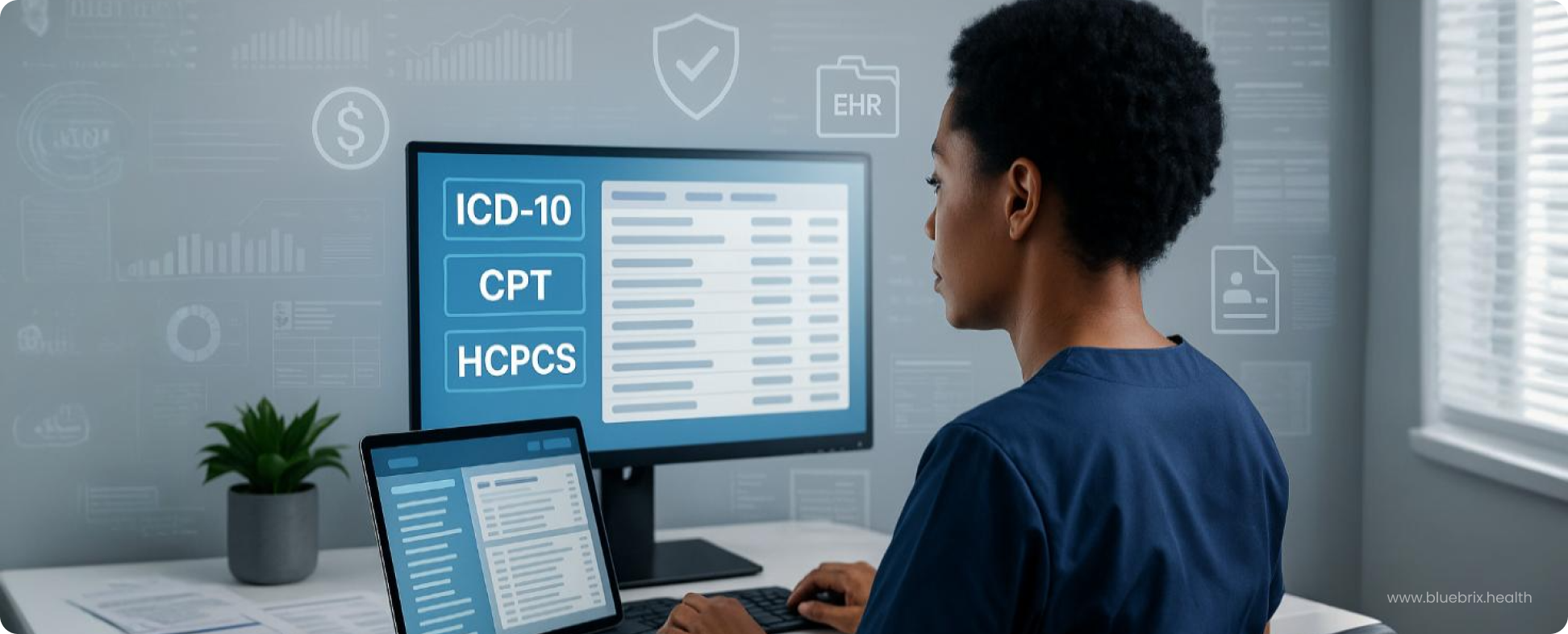
The most common cause of claims denial and audit failure is the misalignment between what the clinician documented and what the regulator requires.
In behavioral health, this friction is intense. A counselor notes a High-intensity group CBT session. The state requires a specific CPT code, a state service code, and often a modifier indicating the practitioner’s licensure level.
The texas CCBHC challenge: time to services
Let’s look at the Certified Community Behavioral Health Clinic (CCBHC) model. Requirements like the I-SERV (Time to Services) measure force you to track the exact minutes between a patient’s initial request for care and their first clinical evaluation. Initial Request might happen via a phone call to your access center, while Initial Evaluation happens in the EHR weeks later. If these two events aren’t linked, your reporting data is invalid.
The operational solution: AI-driven workflow orchestration
A mature platform must replace manual coding with an AI Orchestration engine that automates translation in real-time:
- Contextual Documentation: When the clinician opens the Initial Eval template, the system automatically pulls the Request Date from the intake module.
- Real-Time Validation: If the time-to-service exceeds the 10-day target, the system prompts the clinician to select a Reason for Delay (e.g., Client Rescheduled) during the session.
- Code Translation: The system applies a dynamic rules engine. It sees Psychiatric Evaluation + Duration: 60 mins + MD Provider and automatically assigns the 90791 CPT code, ensuring the claim is clean before it ever reaches the billing team.
For high-volume Medicaid programs, like the CCBHC model in Texas, this is critical. An automated system extracts and stratifies this data, dramatically increasing the Clean Claim Rate and reducing Days in AR.
Pillar 3: The audit-proof matrix: centralized credentialing and compliance monitoring
State reporting increasingly focuses on the operational integrity of the network. A significant audit risk lies in staff credentialing. An auditor’s first move is often to check if the staff member who billed for a service was qualified to deliver it on that exact date.
Every program within a BHN—especially those with SUD or specialized child services—is governed by hyper-specific rules regarding the licensing and training of the staff delivering the service.
The hidden risk: recoupment by technicality
Picture this scenario: An auditor reviews a sample of 100 claims. They find that one of your top counselors, Mark, had his certification expire on June 1st. He renewed it on June 15th.
Every single service Mark delivered between June 1st and June 15th is now considered non-compliant. The auditor recoups those payments and extrapolates that error rate across your entire population of claims. A small administrative oversight becomes a massive financial penalty.
The blueBriX advantage: linking HR to RCM
The solution is a Single Source of Truth for staff credentials hard-linked to your revenue cycle management (RCM).
- Proactive Alerts: The system tracks license expiration dates and automatically issues alerts to the staff member and their supervisor 90, 60, and 30 days out.
- Billing Lockout: The system’s Low-Code/No-Code workflow engine can be configured to execute specific business rules: If Staff License is expired, prevent the submission of any billable claims under that staff ID.
- Audit Trail: During an audit, you can generate a single report proving the staff member was compliant at the time of service. This transforms an audit from a crisis into a routine verification.
Pillar 4: Mastering state-specific reporting with low-code agility
The primary headache for BHN administrators is the variability of state reporting. A network operating across multiple states must comply with totally different requirements—and they change constantly.
The Indiana DARMHA example: agile adaptation
Let’s look at Indiana’s Data Assessment Registry Mental Health and Addiction (DARMHA) system. For State Fiscal Year (SFY) 2026, DARMHA is introducing new requirements, including the mandatory collection of Social Drivers of Health (SDOH) data. In a traditional EHR, adding a specific SDOH questionnaire that maps to the DARMHA export format requires a Change Request to the vendor. This costs money and takes months.
The strategic agility: low-Code/no-code (LCNC)
This is where blueBriX shines:
- Rapid adaptation: Administrators can use visual drag-and-drop tools to map the new SDOH fields to existing clinical data immediately.
- Custom form generation: If a state grant requires a new Critical Incident Report format, you can build the compliant e-form internally without writing code.
- Field mapping: You can map the answers from that form directly to the specific CSV column required by the state manual.
- Future-proofing: LCNC enables you to treat regulatory change—whether from DARMHA, CalAIM, or CMS—as a manageable configuration task, ensuring you are always eligible for new funding streams.
Pillar 5: Automating the quality loop with direct-to-patient digital tools
The final frontier of compliance isn’t about what your doctors write; it’s about what your patients report.
Modern compliance frameworks, especially Value-Based Care and CCBHC grants now mandate the collection of Patient Reported Outcome Measures (PROMs). You are required to track the progression of a patient’s depression (PHQ-9) or anxiety (GAD-7) scores over time to prove your treatment is working.
If you are handing patients a paper clipboard in the waiting room to fill out these forms, you are creating a data quality disaster. Staff must manually transcribe those scores into the EHR. This is slow, prone to data entry errors, and often results in missing data points that lower your quality scores.
The Operational Solution: The Digital Front Door
You need to move compliance to the patient’s own device.
By deploying a white-label Patient Mobile App or a secure Digital Intake Portal, you automate the collection of this critical data.
- Automated prompts: The system automatically pushes a PHQ-9 assessment to the patient’s phone 24 hours before their appointment.
- Direct injection: When the patient submits the form, the data flows directly into the longitudinal record. The system calculates the score, graphs the trend line against previous visits, and flags any High Risk answers (like suicidal ideation) for the clinician immediately.
- Audit readiness: You now have a 100% accurate, time-stamped record of patient outcomes without a single minute of staff data entry.
Turning regulatory friction into competitive velocity
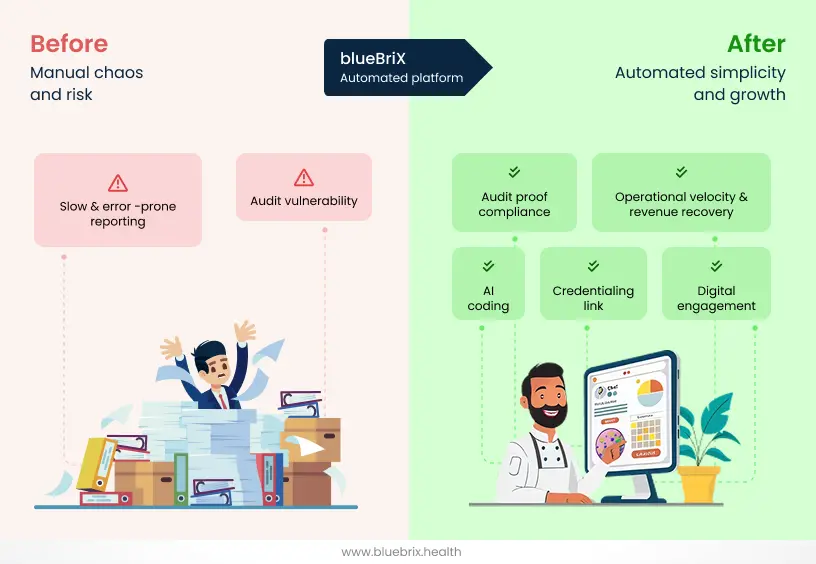
The era of treating state reporting as a back-office burden is over. In the tightening regulatory landscape of 2025, compliance is the primary governor of your network’s growth.
For BHN executives, the choice is stark. You can continue to navigate this complexity with the “Brute Force” method: hiring more administrative staff to patch together spreadsheets, reacting to audits with panic, and accepting high denial rates as the cost of doing business. Or, you can embrace the strategic pivot.
By migrating to a Low-Code/No-Code operational architecture, you don’t just solve today’s reporting headache; you build an immune system for your organization. You transform your data from a fragmented liability into a unified asset. You empower your clinical teams to focus on the patient, knowing the platform is silently orchestrating the compliance, billing, and privacy logic in the background.
When you automate the complexity of state reporting, you do more than just pass an audit. You unlock the velocity required to scale, secure new funding, and deliver on the promise of true, integrated whole-person care.
The question isn’t whether you can afford to modernize your compliance infrastructure. It’s whether your network can afford to survive another year without it.