As the healthcare industry braces for a 30% surge in diagnostic demand over the next decade, the limitations of traditional systems are becoming increasingly apparent. Fragmented data, rising diagnostic complexity, and clinician burnout have created critical gaps in patient care. Studies show that 1 in 10 medical diagnoses is delayed or inaccurate, and diagnostic errors are responsible for nearly 80,000 preventable deaths annually in the U.S. alone. These challenges underscore the urgent need for smarter, more responsive diagnostic tools.
This is where agentic AI steps in, reshaping diagnostics by moving beyond rule-based systems to intelligent, self-learning agents that can interpret complex medical data, predict outcomes, and autonomously guide clinical decisions. From radiology to genomics, these AI-driven systems are transforming the diagnostic landscape, offering a proactive approach that minimizes human error, accelerates clinical workflows, and drives better patient outcomes. In fact, hospitals that have integrated agentic AI have reported up to 50% faster diagnostic turnaround times and 20% lower mortality rates in critical conditions like sepsis.
In this article, we explore how agentic AI is not just augmenting healthcare diagnostics but fundamentally redefining how care is delivered in an increasingly data-driven world.
Challenges in current diagnostic systems
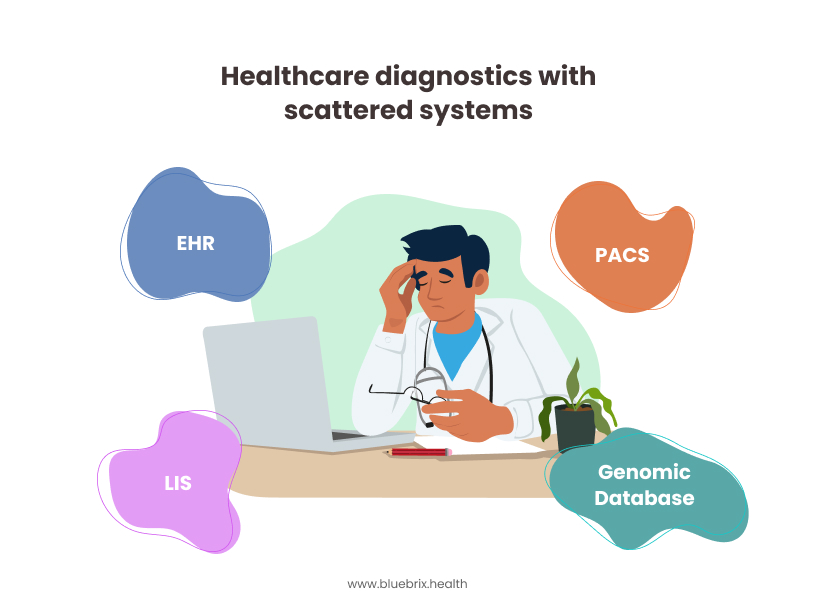
Before discussing what’s transforming, it’s critical to understand what’s broken.
- Fragmented data sources: Clinical information is often scattered across disparate systems—EHRs, PACS, LIS, genomics platforms—leading to data silos that obstruct a comprehensive view of the patient.
- Rising complexity: Clinicians must interpret vast amounts of structured and unstructured data, including imaging, genomics, and continuous monitoring feeds. Manual review is time-consuming and prone to oversight.
- Human fatigue and burnout: Radiologists, pathologists, and lab technicians are expected to review hundreds of cases daily. This contributes to diagnostic errors, with studies estimating that 1 in 10 diagnoses is incorrect or delayed.
- Inconsistencies in diagnosis: Variability between providers—due to experience level, time constraints, or cognitive biases can result in inconsistent or delayed diagnostic outcomes.
- Reactive approach: Most diagnostics still rely on symptoms surfacing rather than predictive monitoring. This delays intervention and escalates treatment costs.
These challenges have exposed a critical need, that is diagnostic systems must evolve from static tools to dynamic agents that operate across modalities, predict outcomes, and guide decisions proactively.
From rules to reasoning: The evolution toward agentic AI
To understand what makes agentic AI so transformative, it helps to look at how healthcare AI has evolved over the years—from simple, rule-following tools to intelligent agents capable of making decisions in real time.
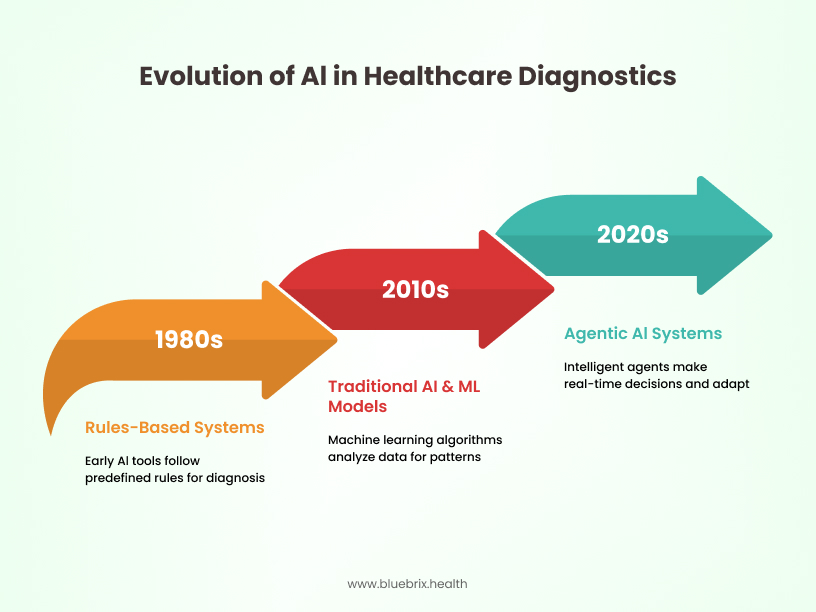
Healthcare’s journey with AI diagnostics has followed a three-stage evolution:
1. Rules-based systems
Early diagnostic tools relied on hard-coded logic or flowcharts. These offered consistency but lacked flexibility. They could only operate within predefined scenarios and broke down when cases became complex.
2. Traditional AI & ML models
Next came supervised machine learning algorithms trained on labelled data (e.g., X-rays with confirmed pneumonia). These models could identify known patterns but struggled with edge cases or unexpected findings. They required frequent retraining and lacked real-time adaptability.
3. Agentic AI systems (current phase)
Today’s cutting-edge diagnostic systems behave like intelligent agents. They:
- Reason contextually: Evaluate clinical scenarios dynamically, even when data is incomplete.
- Act autonomously: Propose and initiate follow-ups (e.g., suggesting next tests, flagging critical patients).
- Learn continuously: Improve from new inputs, feedback, and outcome data—reducing the need for manual retraining.
This evolution marks a transition from rule-following assistants to cognitive collaborators that support clinicians across complex, high-volume diagnostic environments.
Adoption trends and success metrics in healthcare AI
With this technological evolution underway, how far has the healthcare industry come in adopting agentic AI? The following section explores adoption patterns and measurable impact.
The healthcare industry’s adoption of AI technologies—especially agentic systems—is accelerating, though the pace varies by region, infrastructure, and regulatory maturity.
Adoption highlights
- Adoption rate: According to the World Economic Forum and Accenture, over 75% of healthcare executives surveyed in 2024 reported piloting or deploying AI diagnostic solutions within clinical workflows.
- Growth forecast: The global market for AI in diagnostics is projected to grow at a compound annual growth rate (CAGR) of 30%, expected to exceed $11 billion by 2027.
- Radiology & imaging: Nearly one in three U.S. hospitals have implemented AI for radiology triage or decision support.
- Genomics & rare disease: AI systems have helped reduce rare disease diagnosis times from months to under 14 days in clinical pilots.
Success metrics
- Diagnostic accuracy: Studies show AI-enhanced diagnostic tools improve detection accuracy by 15–25% compared to unaided clinicians.
- Workflow efficiency: Agentic AI reduces diagnostic turnaround times by up to 50% in pathology and imaging workflows.
- Mortality reduction: Predictive AI agents have contributed to 20% lower mortality in sepsis and other acute conditions where early intervention is key.
These numbers are not just promising—they reflect a strategic inflection point. AI is not a fringe experiment but a central pillar in diagnostics transformation.
Practical applications of agentic AI in clinical diagnostics
Having seen the scale of adoption, let’s explore where and how agentic AI is making a direct impact across different clinical specialties. Agentic AI is being applied across various clinical specialties to augment diagnostic processes, minimize manual workload, and improve speed and accuracy. Here’s how it is making a difference across key domains:
Radiology: AI as a diagnostic co-pilot
Radiology was one of the first specialties to embrace medical AI, and agentic AI now serves as a diagnostic co-pilot for imaging. These systems help identify abnormalities in X-rays, CT scans, and MRIs and assist with prioritizing cases for radiologist review. Advanced AI models can detect subtle patterns in images—such as small lung nodules, early signs of stroke, or hemorrhages—and present annotated findings to radiologists.
They also provide comparison tools that evaluate current scans against prior images, helping clinicians assess disease progression or recovery. In emergency settings, AI can flag critical scans within seconds to ensure rapid follow-up.
Benefits
- Automates scan analysis, saving radiologists time
- Flags abnormalities for quick review
- Boosts detection accuracy and reduces missed findings
Pathology: Enhancing laboratory diagnostics
Digital pathology is being transformed through AI-powered slide analysis. AI agents analyze whole-slide images for signs of malignancy, inflammation, or abnormal cell patterns. These tools help pathologists detect cancer cells, quantify biomarker expressions (like HER2 or PD-L1), and ensure diagnostic consistency across labs.
AI can also assist with grading tumours, identifying mitotic figures, and flagging atypical cell populations—functions that traditionally require highly trained eyes and time-intensive effort.
Benefits
- Speeds up the slide review process
- Improves consistency across different pathologists
- Increases cancer detection sensitivity significantly
Genomics: Accelerating genetic diagnosis
In genomics, agentic AI helps clinicians navigate the massive complexity of DNA sequencing. AI systems compare a patient’s genetic profile against curated databases of known pathogenic variants and apply statistical models to predict which mutations are likely responsible for disease.
These tools can prioritize genes for follow-up, suggest confirmatory tests, and propose treatment options aligned with a patient’s unique genetic makeup. This is especially useful in paediatrics and oncology, where time-sensitive decisions hinge on fast, accurate interpretation.
Benefits
- Rapidly narrows down genetic suspects
- Supports diagnosis of rare diseases
- Helps personalize treatment plans
Predictive diagnostics: Early warnings and decision support
Agentic AI systems synthesize real-time patient data from monitors, labs, and clinical notes to identify signs of deterioration before they become clinically obvious. These models are trained to detect patterns that precede cardiac arrest, respiratory failure, or sepsis.
For example, an AI model might integrate decreasing oxygen saturation, subtle heart rate variability, and recent infection history to forecast septic shock risk and prompt early antibiotics or ICU evaluation. Clinicians receive alerts in a dashboard or mobile app and can customize thresholds based on patient populations.
Benefits
- Flags early signs of critical conditions
- Supports clinical decision-making
- Reduces mortality and ICU transfers
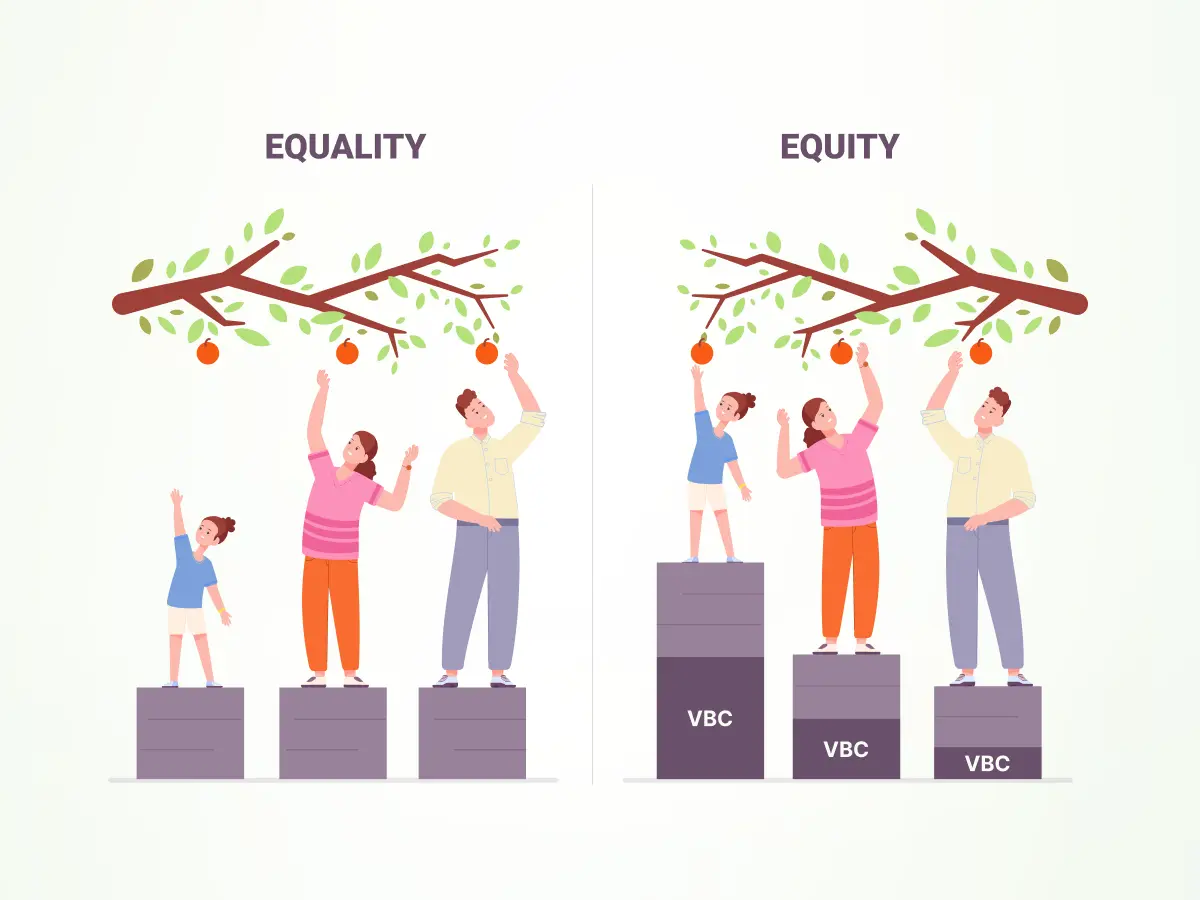
- Agentic AI and Value-Based Care Alignment
Agentic AI is not just a diagnostic enhancer—it is also a critical enabler of value-based care (VBC), where healthcare providers are rewarded for better outcomes rather than higher volumes of services. These intelligent systems help drive proactive and personalized care, aligning clinical operations with financial incentives.
Agentic AI contributes to value based care in several ways:
- Early detection for preventive action: By identifying signs of illness before symptoms appear, AI enables timely interventions, which reduce hospital admissions and improve recovery rates.
- Risk stratification and care planning: AI analyzes a broad range of factors—comorbidities, lifestyle data, social determinants—to stratify patients by risk and guide customized care pathways.
- Continuous monitoring and alerting: AI agents track real-time data like vitals and lab results to catch complications early and help avoid escalation to high-cost care.
- Documentation and reporting support: AI automates clinical documentation and ensures coding accuracy, which improves compliance with quality measures and optimizes reimbursement under VBC models.
What happens when agentic AI Is deployed: A before-and-after story
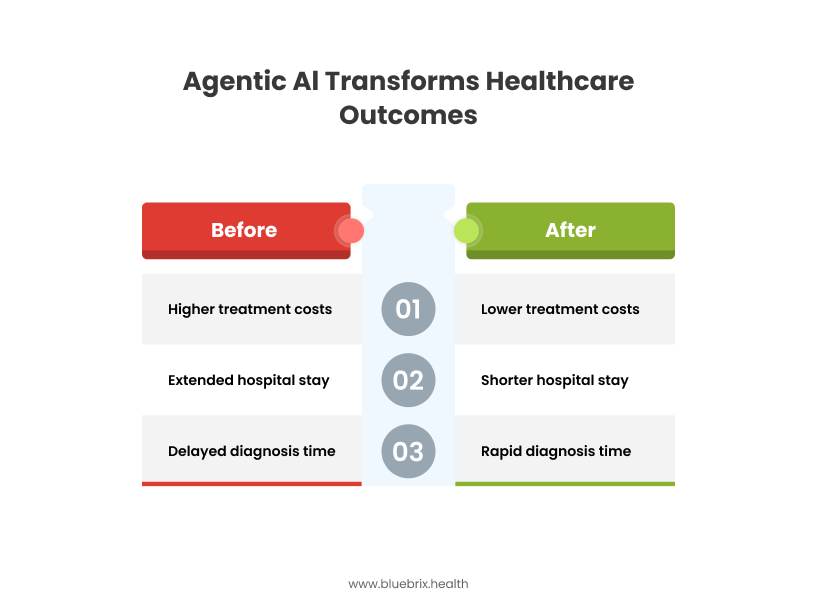
To illustrate the real impact of agentic AI, let’s explore a narrative from the perspective of both the healthcare team and the patient.
Before: A fragmented, reactive experience
Maria, a 62-year-old woman with a history of diabetes and hypertension, visited her regional hospital with complaints of fatigue and shortness of breath. Due to an overburdened diagnostic workflow, her chest X-ray and lab tests faced a backlog. It took over 72 hours to get the radiology report reviewed. Meanwhile, her condition deteriorated unnoticed, and by the time sepsis was identified, it was already in a critical stage. Her hospital stays extended to nearly two weeks, and she required intensive care.
The medical team later noted that warning signs were present in her vital trends, but they were buried under volumes of patient data. The delay in diagnosis not only escalated the clinical risk but also resulted in higher treatment costs and emotional stress for the patient and family.
After: A connected, proactive workflow
Now imagine the same hospital system after implementing agentic AI solutions powered by a secure and interoperable digital health platform. Maria visits again with similar symptoms. This time, the AI agent automatically reviews her chest imaging within minutes and highlights signs of pneumonia. Simultaneously, a predictive AI model running in the background flags her elevated temperature, abnormal WBC count, and subtle oxygen level changes—suggesting a high likelihood of early sepsis.
An alert is sent to the attending clinician through the hospital’s EHR interface, prompting immediate action. Within hours, antibiotics are started, and further deterioration is prevented. Maria is discharged within four days, with no ICU stay required.
In this scenario, both the patient and clinical staff benefit from faster insights, coordinated actions, and significantly improved outcomes. Agentic AI not only reduced diagnostic time but became a proactive partner in patient safety and operational efficiency.
Future outlook: Integrating AI with EHR and digital health
As agentic AI matures, its next chapter will be defined by how well it integrates into the broader digital health ecosystem—transforming not just diagnostics, but entire models of care.
To unlock the full potential of agentic AI, seamless integration into clinical workflows and digital ecosystems is essential. This integration ensures AI insights are contextually relevant, accessible in real-time, and actionable within the existing tools clinicians use daily.
Agentic AI is evolving from standalone tools into embedded intelligence across hospital infrastructure, remote care models, and data ecosystems. These agents will no longer operate in silos but will be integral to clinical decision-making, population health management, and continuous monitoring.
Trends to watch
- Seamless integration with hospital systems: AI agents are being directly embedded into EHRs, LIS, PACS, and clinical decision support platforms, enabling physicians to access AI-powered insights without disrupting their workflows. Integration also allows AI agents to auto-populate notes, suggest orders, or initiate protocols.
- Remote monitoring beyond hospital walls: With the rise of wearable devices and home-based care, AI agents are extending their reach to monitor patients outside traditional care settings. They analyze data from smart devices to detect risk, prompt early intervention, and escalate care when thresholds are crossed—reducing ER visits and hospitalizations.
- Multi-modal AI for holistic diagnosis: Future diagnostic AI will combine inputs from imaging, labs, genomics, patient history, and social determinants of health. These agents will synthesize all relevant data points to deliver personalized, evidence-based diagnostic pathways that go beyond siloed clinical interpretations.
- Interoperability and federated learning: AI agents will increasingly be built to operate across institutions through interoperable frameworks. Federated learning will allow models to improve using anonymized data from multiple hospitals without compromising privacy.
This future positions agentic AI as a connected, intelligent layer within the healthcare delivery fabric—continuously learning, adapting, and improving outcomes at every stage of the care journey.
How blueBriX accelerates diagnostic AI adoption
Turning the promise of agentic AI into real, scalable outcomes requires the right digital foundation. That’s where blueBriX comes in.
As the healthcare industry races toward intelligent, data-driven diagnostics, blueBriX emerges as the launchpad for organizations ready to adopt agentic AI with confidence and speed. More than a platform, blueBriX acts as the connective tissue between clinical systems, AI agents, and real-time decision-making.
What sets blueBriX apart
- Plug-and-play agentic AI integration: Rapidly deploy intelligent diagnostic agents without disrupting existing workflows. blueBriX’s modular architecture enables seamless onboarding of AI tools across radiology, pathology, and genomics.
- Cross-agent coordination: Enable collaboration between AI agents—for example, letting a predictive agent flag a risk and a documentation agent auto-summarize it for physician review.
- Designed for value-based care: Automate quality reporting, detect risk gaps, and help clinicians document accurately—all while meeting Value Based Care compliance standards.
Whether you’re piloting AI in a single department or scaling across a health system, blueBriX ensures that intelligent diagnostics become a reality—not just a roadmap.