
You Have Less Than a Month.
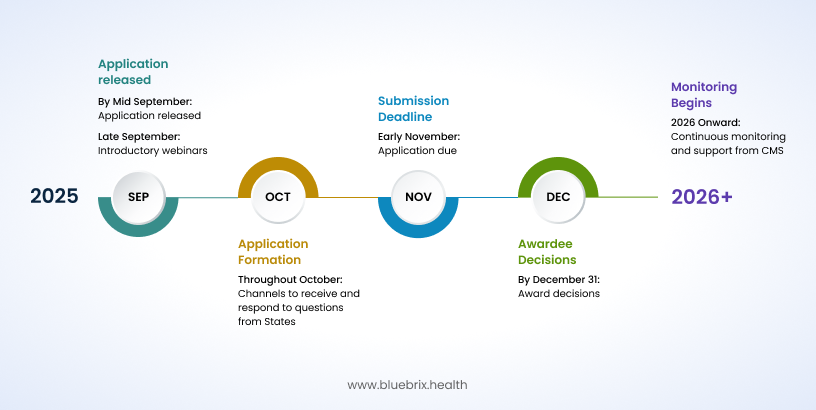
November 5 2025, is the deadline for the Rural Health Transformation Program. $50 billion in federal funding to overhaul rural healthcare delivery across America. This isn’t an annual grant cycle. There’s no reapplication next year. One window. One chance. Missing the deadline could mean leaving substantial funding untapped and rural communities without critical improvements in care delivery.
For healthcare providers, the question isn’t whether you can afford to participate in this transformation—it’s whether you can afford not to.
The $50 billion game-changer: understanding what’s at stake
Over 700 rural hospitals, roughly one-third of the nation’s total, are at risk of closing soon. The launch of Rural Health Transformation Program aims to reverse this scenario through providing access to cutting-edge AI-powered diagnostic tools, robust telemedicine infrastructure, and the resources to retain top-tier healthcare professionals for the next five years.
The program operates on a simple but powerful premise: though the program is set to expire after 5 years, the strategic investments and systemic built are designed to endure, strengthening rural healthcare long after the dollars stop flowing. Unlike traditional grants that fund isolated projects, this initiative takes a holistic ecosystem approach, recognizing that sustainable change requires coordinated effort across entire regions.
How the money flows: a strategic distribution model
The $50 billion isn’t distributed randomly. CMS has designed a sophisticated allocation model that rewards both participation and performance:
- 50% baseline funding: Distributed equally among all approved states, ensuring every participating state gets a substantial foundation
- 50% workload funding: Allocated based on application scores. It’s distributed using two kinds of scores:
- Rural score factors: These are based on numbers and facts, like how big the state’s rural population is, how many rural health clinics and hospitals it has, how much unpaid care those places deliver, and what share of state health services are in rural areas.
- Technical score factors: These measure how strong and practical the state’s plan is, the quality of what they propose, and (in later years) how much they accomplish with the money.
While baseline funding guarantees participation value, performance funding is the multiplier. States with the greatest rural health challenges and most compelling, data-driven strategies can access 2-3x more resources than baseline alone.
The formula is simple: Stronger evidence of need + more innovative solutions = significantly larger allocations.
The urgency factor: why November 5th changes everything
If you’re running a 25-bed rural hospital exploring the Rural Health Transformation Program, you need to act now. Applications must be submitted by states, not individual providers—meaning your state’s designated agency requires detailed input from healthcare stakeholders like you to craft a competitive proposal. That window is closing fast.
Here’s the reality: You’re not just competing against other rural hospitals. You’re up against large healthcare systems, ACOs, and technology companies across your entire state for inclusion in a single state application.
The clock is ticking.
Strategic positioning for healthcare providers: your roadmap to inclusion
Understanding your role in the state application process
While healthcare providers are not the direct applicants for the Rural Health Transformation Program, your input deeply influences the state’s application making you a strategic implementation partner. States require detailed insights from frontline providers to shape their Rural Health Transformation plans. This data and feedback allow states to accurately represent the local healthcare landscape, identify gaps, and design targeted proposals that meet both CMS requirements and community needs.
Your role is pivotal, not in grant writing but in helping your state craft a competitive application that can secure a slice of the $50 billion pie.
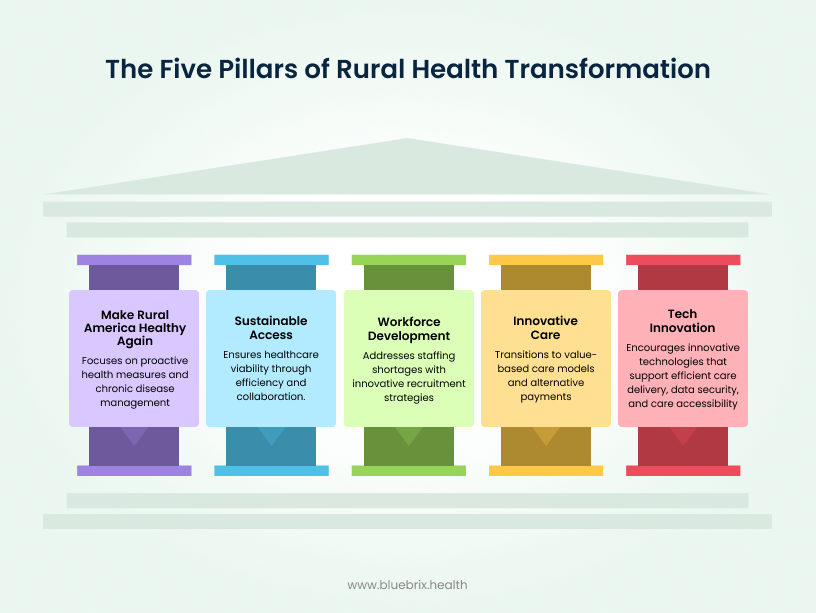
By actively sharing outcomes, sustainable practices, and innovative strategies that align with the five pillars, you help prove to CMS that your state’s plan is grounded and ready for successful implementation. This engagement increases the likelihood that your priorities are included and funded.
Technology investment: the core of rural health transformation
The Rural Health Transformation Program explicitly prioritizes technology innovation, and for good reason. Rural healthcare’s most persistent challenges such as geographic isolation, workforce shortages, and resource limitations, precisely the problems that innovative technology solutions can address most effectively.
The Rural Health Transformation Program explicitly prioritizes technology innovation. Why? Because rural healthcare’s biggest barriers are distance, staff shortages, limited resources which can’t be solved with traditional approaches alone. Here technology is the equalizer. Telemedicine closes geographic gaps, AI-driven tools stretch limited clinical capacity and unified data platforms enable coordination that manual processes never could.
The program recognizes what forward-thinking providers already know: innovation isn’t optional anymore. It’s the only scalable solution to rural healthcare’s structural problems.
Approved technology investment categories include:
- Training and technical assistance for advanced technologies like AI and robotics
- IT infrastructure improvements focusing on efficiency and enhanced cybersecurity
- Consumer-facing chronic disease management solutions
- Remote care and digital health tools that expand access beyond traditional facility walls and facilitates coordinated care
The ROI reality: why technology investment pays off
Healthcare technology ROI isn’t theoretical. It’s measurable and substantial. Effective EHR optimization drives significant administrative cost savings, typically achieving payback within a few years while delivering substantial overall returns.
But the real gain isn’t just cost savings, it’s revenue optimization through improved care coordination. Modern care coordination platforms enable:
- Enhanced quality scores that trigger bonus payments in value-based contracts
- Reduced length of stay through better discharge planning and follow-up care
- Improved chronic disease management that prevents expensive emergency interventions
- Streamlined administrative processes that free up staff for patient-facing activities
Multi-stakeholder transformation: everyone has a role
Rural healthcare transformation isn’t a top-down initiative, it’s a community-wide collaboration requiring active participation from patients, providers, payers, and system leaders.
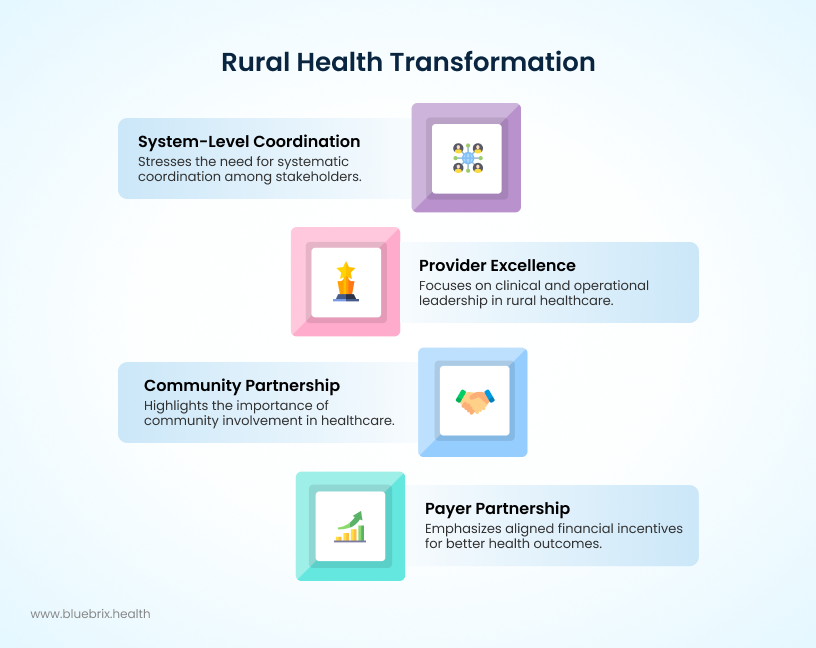
Provider excellence: clinical and operational leadership
Rural providers must embrace dual excellence: clinical outcomes and operational efficiency. This means investing in quality measurement systems, care coordination platforms, and technology proficiency development while maintaining the personal touch that rural communities value.
Success requires:
- Implementing robust data analytics for population health management
- Developing proficiency with AI-powered clinical decision support tools
- Participating actively in value-based care arrangements
- Collaborating effectively across regional healthcare networks
- Promoting evidence-based, measurable interventions to improve prevention and chronic disease management
Payer partnership: aligned incentives for better outcomes
The most successful Rural Health Transformation initiatives will feature strong payer partnerships that align financial incentives with improved outcomes. This means developing shared savings programs, quality bonus arrangements, and risk-sharing agreements that reward providers for keeping patients healthy rather than treating them when they’re sick.
Effective payer partnerships include:
- Real-time data sharing for performance analytics and care management
- Streamlining administrative processes such as prior authorizations to reduce provider burden.
- Joint investments in technology infrastructure to support digital health tools, interoperability, and care coordination.
Community partnership: meeting social needs for better health
The Rural Health Transformation Program encourages strong community involvement as a key pillar. This means identifying patient needs related to housing, transportation, and food security, and supporting programs for opioid and substance use disorders as well as behavioral health.
Effective community partnerships include:
- Connecting patients to social services that affect their health.
- Expanding outreach for mental health and substance use treatment.
- Acting as advocates and feedback channels to keep transformation efforts grounded in real community needs.
System-level coordination: the integration imperative
Rural healthcare transformation requires systematic coordination across all stakeholders. This means developing communication protocols, resource allocation strategies, and performance measurement systems that ensure everyone is working toward common goals.
Implementation strategy: from vision to reality
The phased approach to technology deployment
Successful technology implementation in rural settings requires a carefully orchestrated approach. Start with infrastructure assessment and planning, move through system selection and procurement, implement comprehensive training and change management programs, and establish ongoing performance monitoring and optimization processes.
The key is avoiding the “big bang” implementation mistake. Rural healthcare organizations typically have limited IT support and constrained training resources, making gradual, well-supported technology adoption more sustainable than dramatic overnight changes.
Success metrics That Matter
The Rural Health Transformation Program emphasizes measurable outcomes, making robust performance measurement essential. Key metrics include:
- Clinical outcomes: Readmission rates, quality scores, patient satisfaction
- Financial performance: Cost per episode, revenue optimization, operational efficiency
- Operational metrics: Staff productivity, technology adoption rates, care coordination effectiveness
- Community impact: Access improvements, population health indicators, workforce retention
The time-sensitive opportunity: your next steps
With the November 5th application deadline approaching, healthcare providers must act quickly to position themselves for inclusion in their state’s Rural Health Transformation application.
Immediate action items include:
- Contact your state’s designated RHT Program agency to understand their application strategy and timeline
- Document your current technology capabilities and identify specific areas for improvement
- Develop measurable outcome projections for your proposed technology investments
- Build stakeholder coalitions with other regional healthcare providers
- Prepare detailed implementation timelines and resource requirements
The long-term vision: sustainable rural healthcare transformation
As Centers for Medicare and Medicaid Services administrator Mehmet Oz said, “We think we have an opportunity not just to plug a few of the holes, but to transform in a lasting way the rural health care system in this country.” The Rural Health Transformation Program isn’t just about the next five years, it’s about building sustainable healthcare delivery systems that will serve rural communities for generations. Technology investment serves as the foundation, but the real transformation comes from coordinated care, engaged communities, and aligned stakeholders working together toward common goals.
For rural healthcare providers, November 5th, 2025, represents more than an application deadline—it’s a pivotal moment that will determine whether your community thrives in the evolving healthcare landscape or gets left behind.