Direct Primary Care (DPC) is transforming healthcare offering affordable, personalized care outside traditional insurance models. But as the DPC market grows, projected to reach $15 billion by 2033, many clinics are facing a new challenge: how to grow and retain patients while staying lean and efficient.
The answer isn’t just more staff or longer hours, but smarter infrastructure. The most successful DPC practices use technology to streamline care coordination, simplify referrals, personalize care plans, and improve patient engagement.
If your DPC is looking to expand panels, improve satisfaction, or attract employer contracts, this guide will show you how the right DPC technology platform like blueBriX can help.
What’s driving the growth of Direct Primary Care?
Let’s start with the facts: DPC isn’t just trending, it’s transforming primary care delivery across the globe.
- Market Expansion: The global direct primary care market grew from $65.61billion in 2024 to $70.42billion in 2025, posting a 7.3% compound annual growth rate (CAGR).
- Long-Term Outlook: Projections show DPC surging to $92.51billion by 2029, fueled by increased demand for personalized care, dissatisfaction with traditional fee-for-service models, and the rising burden of chronic disease.
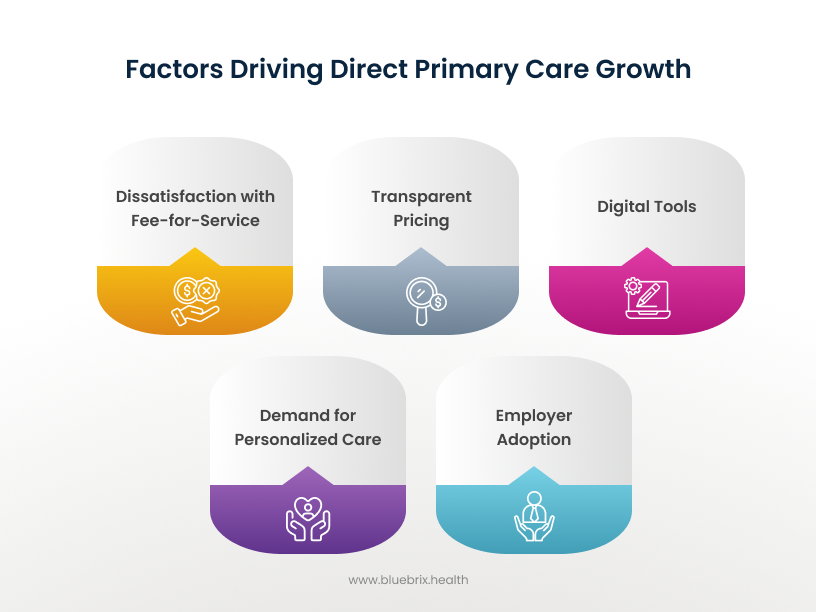
- Driving Forces: Key reasons for DPC’s popularity include:
- A holistic, patient-first approach.
- Simpler access and flexibility
- Transparent, predictable costs for both patients and providers.
- The burnout and shortage crisis in conventional primary care.
DPC’s relevance is further amplified by demographic and health trends:
- Chronic disease prevalence, particularly diabetes and obesity, highlights the need for continuous, coordinated primary care.
- Patients want longer appointments, more direct communication, and proactive wellness—all DPC hallmarks.
The Revolutionary Tax Advantage: Pre-Tax Benefits for DPC
On July 4, 2025, the “One Big Beautiful Bill Act” (OBBBA) was signed into law. Section 71308 represents a watershed moment for the DPC industry—creating financial pathways that make this model more viable for both individuals and employers.
Key Regulatory Changes (Effective January 1, 2026):
- HSA Eligibility: For the first time ever, individuals with High Deductible Health Plans (HDHPs) can maintain HSA eligibility while enrolled in qualifying DPC arrangements. Previously, the IRS considered DPC a form of insurance excluding millions of HSA holders from using their funds for DPC fees.
- Pre-Tax Payment: DPC membership fees are now classified as qualified medical expenses, meaning patients can use pre-tax HSA dollars to pay for their monthly subscriptions—unlocking meaningful savings.
- Monthly Limits:
- Up to $150/month for individual coverage
- Up to $300/month for family coverage
Both limits will be indexed for inflation annually
- Employer Benefits:
These changes make it easier for employers to offer DPC as a covered benefit, knowing that HSA-eligible employees can now use pre-tax dollars to participate—boosting retention and reducing healthcare costs in the long term.
Direct Primary Care isn’t just growing—it’s gaining momentum from market demand, clinician support, and now, federal policy. With new tax advantages and regulatory clarity, DPC is positioned to become a mainstream solution for personalized, affordable, and value-driven care in 2026 and beyond. But with growth comes complexity. Clinics often struggle with manual coordination, patient follow-up, and data reporting—especially as they scale or serve employer populations.
Increasing Patients in Your DPC Practice: The Modern Playbook
Growing your DPC patient base relies on both delivering value and making sure people know about it.
- Prioritize Whole-Person Care: Today’s patients are choosy. They expect everything – access, compassion, proactive management, and easy communication.
- Emphasize Accessibility: Online booking, telemedicine, and same-day visits help you stand out.
- Be Transparent: Publish your pricing, services, and wait times on your website.
- Educate the Market: Use blogs, webinars, and local events to explain DPC’s advantages, especially around chronic disease management and long-term cost savings.
- Leverage Patient Referrals: Positive word of mouth is especially powerful in primary care. Make it easy for happy patients to refer friends and family.
- Create a Seamless Experience: Every interaction should be effortless, from sign-up to appointment reminders to follow-up.
- Partner with Employers: Many companies now offer DPC as an employee benefit. Build relationships with local businesses.
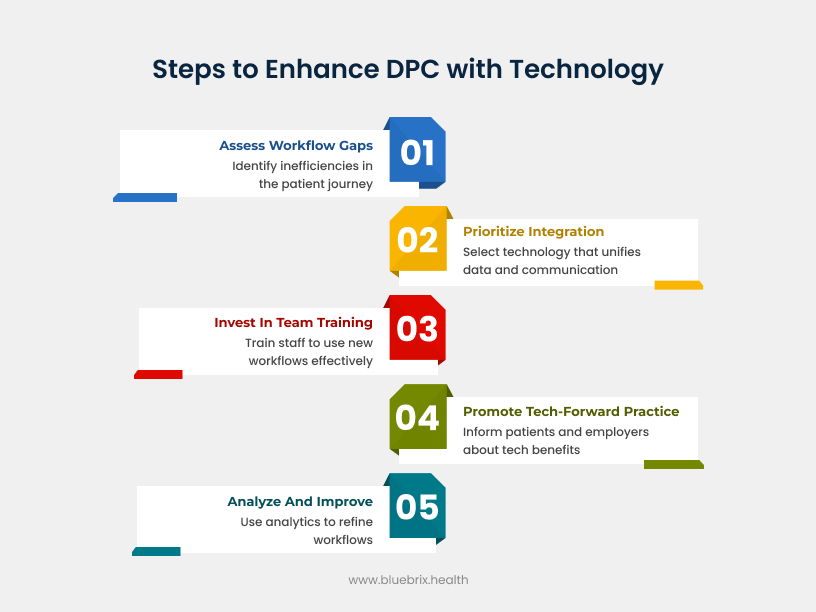
- Invest in Right Technology: An integrated all-in-one technology will help practice management, care delivery and patient engagement proactive, thereby reducing escalations, costs and burnout.
Why Technology Is the Growth Engine
You can’t scale modern DPC or provide the best patient experience without the right technology. DPC’s appeal is direct access and sustained relationships, but without smart technology, even the most dedicated provider gets stretched thin. The key lies in adopting a Direct Primary Care technology platform that includes:
- Care coordination tools to track follow-ups, labs, and referrals
- Referral management software that closes the loop with external specialists
- Patient engagement platforms to send reminders, secure messages, and updates
- Customizable care plan templates for chronic and preventive care
- Population health dashboards to demonstrate value to employers
Here’s how technology empowers DPC practices to grow:
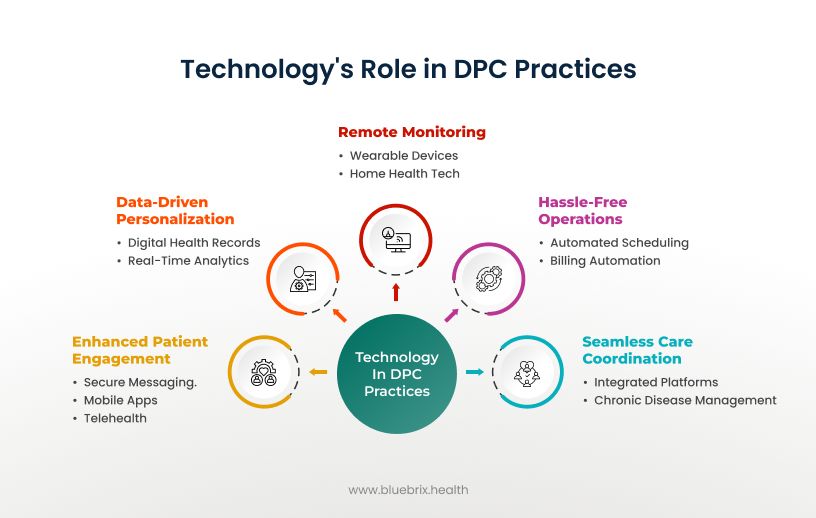
- Enhanced Patient Engagement:
- Secure messaging and mobile apps keep patients connected, boosting satisfaction and adherence.
- Virtual check-ins and telehealth remove barriers to accessing care, especially for busy families or rural patients.
- Seamless Care Coordination:
- Integrated digital platforms ensure everyone on the care team is on the same page – whether handling chronic diseases or routine follow-ups.
- Hassle-Free Operations:
- Automating appointment scheduling, reminders, and billing cuts admin work, reduces no-shows, and drives operational efficiency.
- Data-Driven Personalization:
- Digital health records and analytics allow for real-time tracking of patient outcomes, supporting proactive, personalized care.
- Remote Monitoring:
- Wearable devices and home health tech enable early intervention, often before a patient realizes they need help.
What does this mean for your practice? More time with patients, fewer avoidable emergencies, stronger retention, and the ability to support a larger patient panel without compromising quality.
Why Fragmented Tech Is Holding DPC Back
Let’s be honest: many practices struggle with disjointed systems—separate tools for scheduling, messaging, care planning, patient engagement and analytics. This fragments the patient experience and creates care gaps that lead to:
- Missed escalations and preventable hospitalizations.
- Poor care team coordination.
- Lower patient satisfaction and retention.
- Difficulty tracking and demonstrating value, which is crucial for employer partnerships and payer negotiations.
Eliminating fragmentation is no longer optional—it’s essential for DPC practices that want to thrive.
Top reasons DPC clinics need a care coordination platform
1. Referral Management for DPC Clinics: Prevent Patient Leakage
Without structured referral tracking software, patients referred to specialists or labs often fall through the cracks. In fact, up to 65% of patients never complete a specialist visit if not properly followed up.
blueBriX’s referral management module ensures:
- Real-time status tracking of referrals
- Follow-up alerts for staff
- Seamless communication with external providers
This keeps patients engaged and reduces attrition—crucial for growing panels.
2. DPC Care Plan Software: Scale Personalized Preventive Care
DPC’s promise lies in longitudinal, personalized care—but this becomes harder with larger patient panels.
blueBriX offers:
- A care plan engine that personalizes treatment plans for chronic conditions
- Pre-built templates for diabetes, hypertension, obesity, and more
- Patient-facing progress trackers and alerts
This enables clinics to deliver proactive, value-based care at scale—without adding overhead.
3. DPC Patient Engagement Tools: Boost Retention and Satisfaction
Word-of-mouth drives most DPC growth. That means patient experience is everything.
With blueBriX’s patient communication hub, clinics can:
- Send secure messages and lab reminders
- Schedule check-ins and follow-ups
- Run campaigns (e.g., annual screenings, flu shots)
These tools make patients feel supported—even outside the visit—leading to higher satisfaction, retention, and referrals.
4. DPC Employer Reporting: Prove ROI with Dashboards
As employer-sponsored DPC becomes more popular, so do requests for data.
Employers want to know:
- How many employees are engaged?
- What care gaps are being closed?
- Are emergency visits being avoided?
blueBriX enables clinics to generate:
- White-labeled employer reports
- Real-time dashboards tracking engagement, screenings, and follow-ups
- Population health insights by condition or risk
This helps DPCs win—and retain—employer partnerships.
5. All-in-One DPC Technology Platform: Eliminate Tool Fatigue
Many DPCs cobble together stacks like Elation + Hint + Klara, which leads to:
- Disconnected workflows
- High switching costs
- Limited customization
blueBriX consolidates everything in one care operating system:
- No-code workflow builder
- Referral, task, and care plan engines
- Interoperable modules that plug into labs, EHRs, and billing tools
It’s the best of both worlds: a fully unified DPC tech stack with complete flexibility.
Direct Primary Care vs Value Based Care: What's the Difference—and Why It Matters for Your Tech Stack
While Direct Primary Care and Value-Based Care both aim to improve patient outcomes, lower costs, and prioritize preventive care, they differ significantly in structure, funding, and operational complexity.
Key differences between DPC and VBC:
- Who Pays:
DPC is funded directly by patients or employers through a membership model. Value Based Care is funded by payers (like Medicare or insurance companies) and typically involves complex contracts and reimbursement models. - Regulatory Burden:
DPC operates with fewer compliance requirements. Value Based Care providers must meet detailed reporting standards, risk-adjustment metrics, and government quality benchmarks. - Payment Model:
DPC uses a flat monthly or annual fee with no fee-for-service (FFS) billing. Value Based Care often uses shared savings, capitation, or bundled payments tied to performance. - Care Scope:
DPC focuses primarily on outpatient and preventive primary care. Value Based Care includes a broader spectrum—hospital, specialty, emergency, and post-acute care. - Outcome Measurement:
In DPC, patient satisfaction and continuity drive success. In Value Based Care, performance is measured through payer-defined metrics like HEDIS scores, utilization rates, and cost benchmarks.
Why These Differences Matter for Technology Selection
Even though DPC is simpler, the need for care coordination, patient engagement, and outcome tracking is just as important as in Value Based Care. What’s different is the type of tech infrastructure required:
- DPCs need a lightweight, customizable platform that supports care delivery without unnecessary complexity.
- Value Based Care organizations often require robust compliance and claims analytics, layered with regulatory workflows.
That’s why blueBriX is uniquely suited to DPCs: it offers the same clinical precision and coordination tools used in enterprise VBC models—but without the payer-focused bulk. DPC clinics can manage care plans, referrals, patient communication, and even employer reporting from a single, adaptable platform.
In other words, blueBriX gives DPCs the tech sophistication of a Value Based Care player, with the simplicity and flexibility their model demands.
Real-World Impact: Why the Right Platform Matters
Practices using blueBriX-style, advanced care coordination platforms report:

- Fewer missed interventions, with high-risk patients flagged for outreach automatically.
- Higher patient retention, thanks to personalized care plans and robust engagement channels.
- Demonstrably lower costs—through reduced ER visits, admissions, and streamlined internal processes.
- Improved quality scores (HEDIS, Stars), vital for winning employer contracts and payer negotiations.
- Clinics using structured referral systems see scheduling times drop from days to minutes
- Employer-sponsored DPCs using care coordination platforms report higher engagement and fewer ER visits
- DPC practices with built-in reporting and messaging see higher retention and faster word-of-mouth growth
- Technology-enabled DPCs can scale from solo to multi-location without losing consistency or quality
What to Look for in Direct Primary Care Software
If you’re evaluating Direct Primary Care EHR or care coordination tools, make sure the platform offers:
- A care plan engine to personalize and track patient progress
- A referral tracker to close care loops
- HIPAA-compliant patient messaging and reminders
- Task and workflow management for your care team
- Population health dashboards to monitor outcomes
- Employer-facing reports to show value
- No-code customization to fit your style of care
- Integration with labs, external providers, and existing systems
blueBriX delivers all of this and more in a lightweight, scalable platform built for real-world DPC needs.

