Dementia is a formidable challenge, impacting millions of lives and placing immense pressure on families and the healthcare system. For behavioral health clinics, the landscape of dementia care is evolving, presenting both opportunities and responsibilities. The Centers for Medicare & Medicaid Services (CMS) has introduced a groundbreaking initiative, the Guiding an Improved Dementia Experience (GUIDE) Model, poised to revolutionize how we approach dementia care. This model specifically recognizes the critical role of behavioral health in comprehensive dementia management.
At blueBriX, we understand the complexities and nuances of integrated care. Our purpose-built behavioral health EHR can help behavioral health clinics navigate this new era, positioning themselves for success and, most importantly, improving the lives of individuals living with dementia and their caregivers.
The Growing Challenge of Dementia in Behavioral Health
Dementia is not merely a cognitive decline; it profoundly affects mental and emotional well-being. Individuals with dementia frequently experience a range of behavioral and psychological symptoms (BPSD), including depression, anxiety, agitation, and psychosis. These symptoms significantly impact their quality of life and can exacerbate functional decline.
Beyond the patient, the burden on unpaid caregivers is immense. Studies consistently show that caregivers of people with dementia experience higher rates of stress, depression, and anxiety. For instance, research indicates that caregivers frequently report symptoms akin to post-traumatic stress disorder, and many experience significant psychosocial stressors like role strain and social isolation. The psychological well-being of caregivers is directly linked to the severity of the patient’s neuropsychiatric symptoms.
This interconnectedness underscores the urgent need for integrated behavioral and physical health care. Fragmented care often leads to worse outcomes, increased emergency department visits, and higher rates of institutionalization. Behavioral health professionals are uniquely positioned to address the emotional, psychological, and social complexities associated with dementia, providing crucial support that goes beyond medical management.
The CMS GUIDE Model
Enter the CMS GUIDE Model, or “Guiding an Improved Dementia Experience.” Launched by CMS, this voluntary nationwide model is an eight-year initiative designed to provide comprehensive, coordinated care for people living with dementia (PLWD) and their unpaid caregivers.
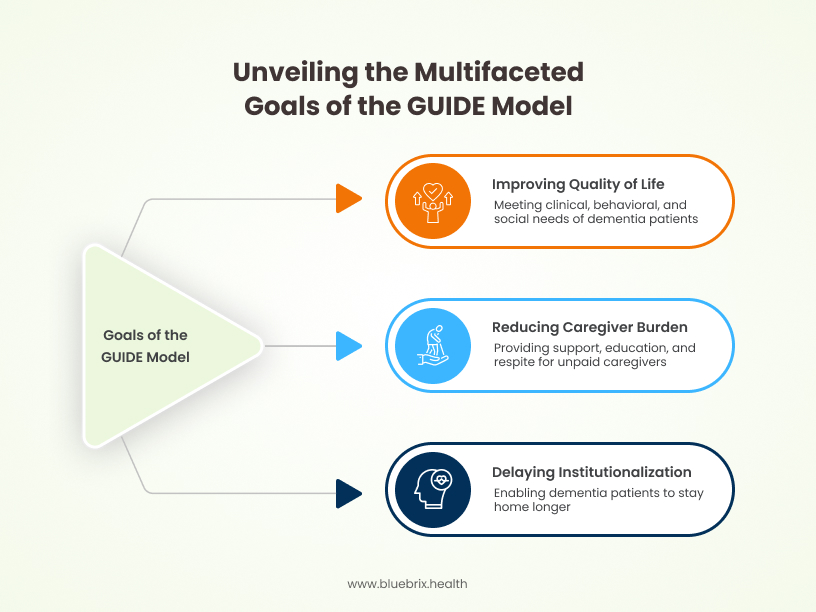
This model represents a significant shift towards value-based care in dementia, recognizing that holistic support, rather than episodic treatment, leads to better outcomes and lower overall healthcare costs.
Why Behavioral Health Clinics Must Pay Attention
The GUIDE Model is not just for primary care or neurology; it’s a call to action for behavioral health clinics. Here’s why:
Behavioral health professionals – psychiatrists, psychologists, social workers, and therapists – are essential in diagnosing and managing the neuropsychiatric symptoms of dementia. Their expertise is vital in developing person-centered care plans that address mood disorders, agitation, and other challenging behaviors, which are often the primary drivers of caregiver stress and patient decline.
By participating in the GUIDE Model, behavioral health clinics can expand their services, integrate more deeply into comprehensive care networks, and access new reimbursement streams. This offers a unique opportunity to enhance patient care by formally recognizing and compensating for the critical behavioral health support that is often overlooked in traditional care models. It’s about building a more sustainable and impactful future for your practice in dementia care.
Deconstructing the CMS GUIDE Model: Key Components for Behavioral Health
The CMS GUIDE Model outlines a comprehensive framework for dementia care, with several key components that directly align with and necessitate the expertise of behavioral health clinics. Understanding these elements is crucial for successful participation.
Core Elements of the GUIDE Mode
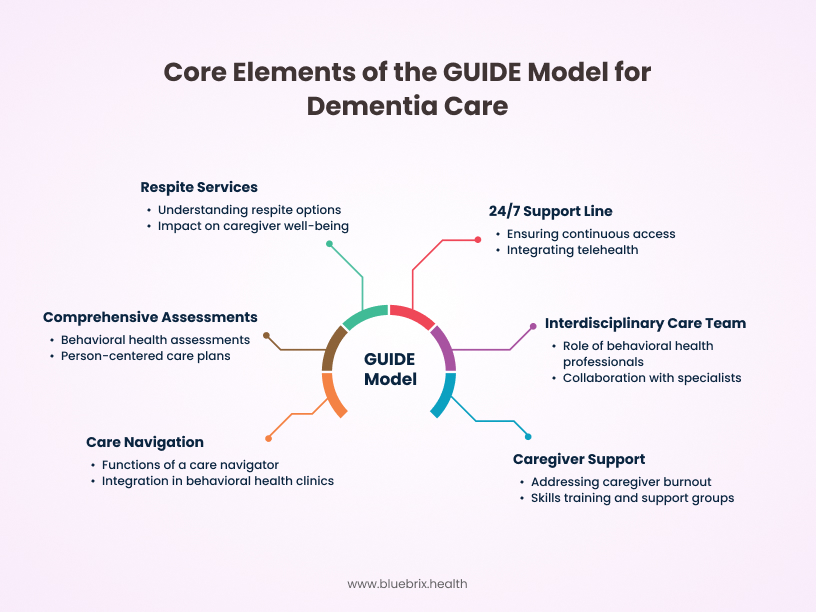
The GUIDE Model mandates a standardized approach to dementia care that is built on a foundation of integrated services.
Comprehensive, Person-Centered Assessments and Care Plans:
A cornerstone of the GUIDE Model is the requirement for comprehensive assessments. For behavioral health clinics, this means performing in-depth evaluations of the patient’s mood, cognition, agitation, psychosis, and overall psychological well-being. These assessments go beyond standard diagnostic criteria to capture the lived experience of dementia and its emotional impact. The care plan must be person-centered, reflecting the individual’s goals, preferences, and needs, as well as those of their caregiver. Behavioral health goals, such as managing anxiety, reducing agitation, or improving sleep patterns, must be explicitly integrated into these plans, with measurable objectives and tailored interventions.
Interdisciplinary Care Team Requirements:
The GUIDE Model mandates an interdisciplinary care team. This is where psychiatrists, psychologists, social workers, and therapists become indispensable. They are not merely consultants but active, integral members of the team, contributing their expertise in areas like medication management for BPSD, cognitive behavioral therapy adaptations, and family counseling. Effective care in the GUIDE Model hinges on seamless collaboration. Behavioral health professionals will work closely with primary care physicians, neurologists, geriatricians, and other specialists to ensure a unified approach to patient care, addressing both physical and mental health needs.
Care Navigation: The Central Hub of Support:
A dedicated Care Navigator is a central figure in the GUIDE Model. This individual acts as a liaison, connecting patients and caregivers with necessary services, managing appointments, and providing ongoing support. They are crucial for ensuring continuity of care and preventing patients from falling through the cracks. Behavioral health clinics can either employ their own care navigators or partner with organizations that provide these services. Given the complexity of behavioral health needs in dementia, a care navigator with a strong understanding of mental health resources and support systems will be invaluable.
Robust Caregiver Support and Education:
The GUIDE Model places significant emphasis on supporting unpaid caregivers, recognizing their vital role. This includes proactively addressing caregiver burnout, depression, and anxiety through dedicated counseling, support groups, and mental health interventions. The high prevalence of mental health challenges among caregivers makes this a direct fit for behavioral health expertise. Behavioral health clinics can offer tailored programs for caregivers, including skills training for managing challenging behaviors, individual and family counseling, and facilitating peer support groups. This not only benefits caregivers but also indirectly improves patient outcomes by reducing caregiver stress and improving the care environment.
Access to Respite Services:
The GUIDE Model includes reimbursement for respite services, which provide temporary relief to caregivers. Behavioral health clinics should be familiar with local respite options (e.g., adult day centers, in-home care) and the reimbursement mechanisms under GUIDE, helping caregivers access these crucial breaks. Respite care is vital for preventing caregiver exhaustion and maintaining their capacity to provide care, ultimately delaying institutionalization and enhancing the stability of the patient’s living situation.
24/7 Access to Support Line:
Participants in the GUIDE Model must ensure 24/7 access to a support line for patients and caregivers. For behavioral health clinics, this means integrating their crisis intervention services or partnering with emergency mental health providers to offer continuous access to behavioral health support, especially for managing acute behavioral symptoms or caregiver distress. Telehealth platforms can be instrumental in providing after-hours behavioral health support, allowing for timely interventions and reducing the need for emergency department visits.
Patient and Provider Eligibility
Understanding who can participate is key to strategizing your clinic’s involvement.
Who is Eligible for GUIDE Model Services?
Beneficiaries eligible for the GUIDE Model must be enrolled in Medicare Parts A & B (Fee-for-Service) and cannot be enrolled in Medicare Advantage or Special Needs Plans (SNPs). They must have a confirmed dementia diagnosis and be living at home or in a community dwelling, not residing in a long-term nursing home or receiving hospice or PACE services. Approximately 10% of Medicare beneficiaries with dementia are estimated to qualify.
Eligibility for Behavioral Health Clinics to Participate:
Requirements for “Dementia Proficiency”
To participate as a “Dementia Care Program” (DCP), organizations must meet specific criteria for “dementia proficiency.” This can be demonstrated if at least 25% of a clinician’s patient panel comprises adults with any cognitive impairment (including dementia), or 25% of their patient panel is aged 65 years or older, or if they have a specialty designation in neurology, psychiatry, geriatrics, geriatric psychiatry, behavioral neurology, or geriatric neurology. Behavioral health clinics with existing expertise in geriatric psychiatry or neuropsychology are ideally positioned to meet these requirements.
Opportunities for New vs. Established Programs
The GUIDE Model offers two tracks: one for established programs ready to implement immediately, and another for new programs interested in scaling to meet GUIDE requirements. This provides a pathway for behavioral health clinics at various stages of dementia care integration.
Reimbursement and Financial Incentives
The financial structure of the GUIDE Model is designed to support the comprehensive care delivery it requires.
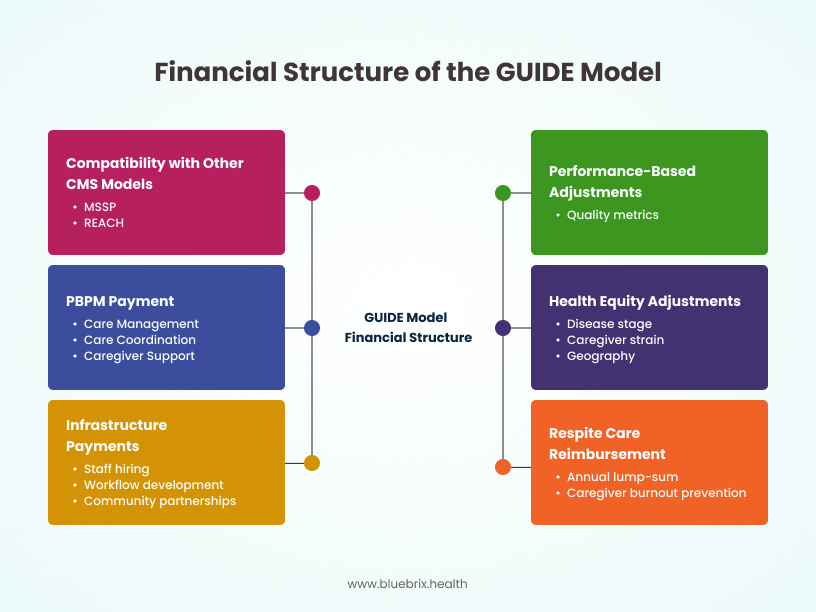
Understanding the Per-Beneficiary Per-Month (PBPM) Payment:
Participants receive a monthly per-beneficiary, per-month (PBPM) payment for providing the required care management, coordination, and caregiver support services. This bundled payment model incentivizes integrated, proactive care.
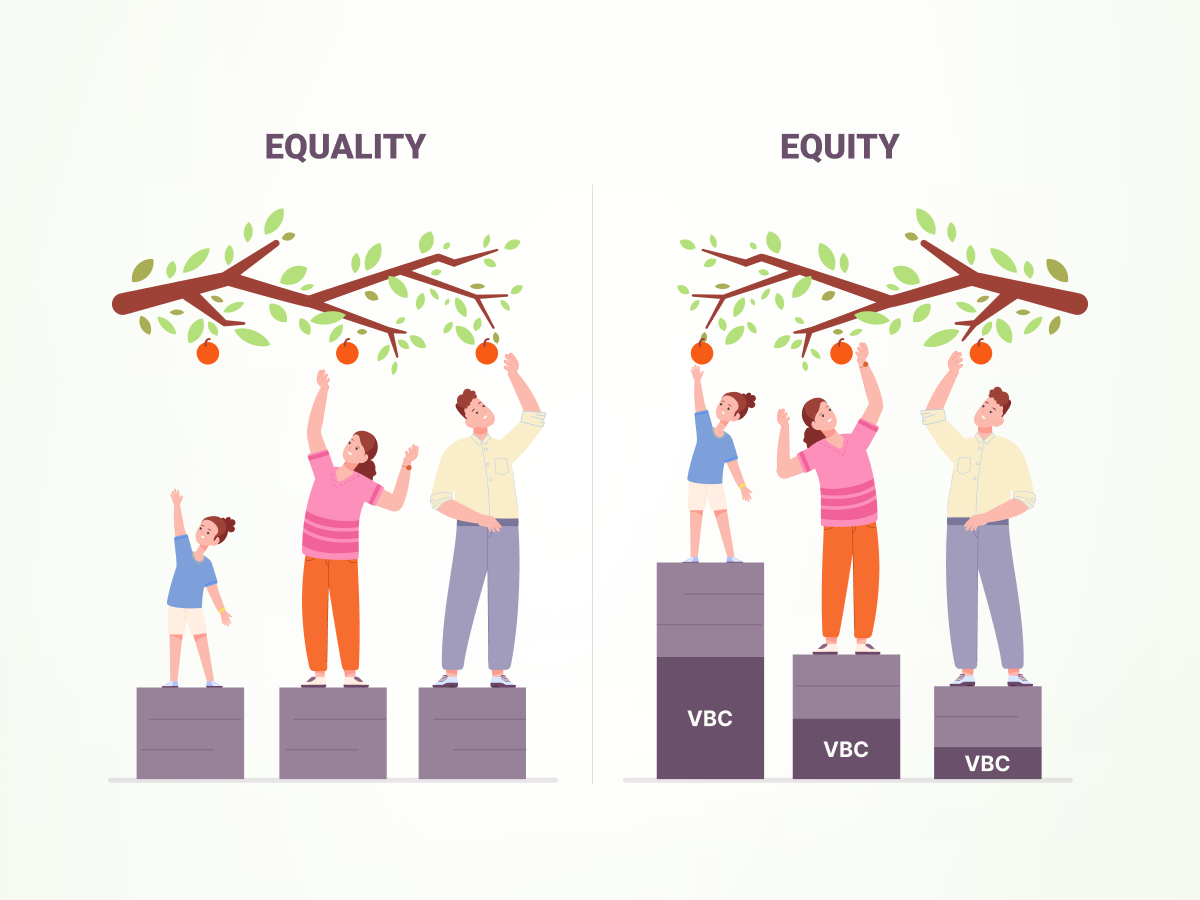
Health Equity Adjustments and Performance-Based Adjustments:
The PBPM payment is adjusted based on various factors, including the patient’s disease stage, the presence and strain of a caregiver, geography, and importantly, health equity adjustments. This incentivizes providers to care for underserved populations. There are also performance-based adjustments linked to quality metrics, encouraging high-quality care.
Respite Care Reimbursement:
A separate annual lump-sum payment (with a cap) is provided for caregiver respite services, offering a direct financial incentive to support caregivers and prevent burnout.
Infrastructure Payments for Program Development:
CMS also offers one-time infrastructure payments to support the development of GUIDE programs, which can be invaluable for behavioral health clinics looking to build out their dementia care capabilities, including hiring and training staff, developing workflows, and establishing community partnerships.
Compatibility with Other CMS Models (e.g., MSSP, REACH):
Crucially, the GUIDE Model is compatible with other CMS payment models like the Medicare Shared Savings Program (MSSP) and Realizing Equity, Access, and Community Health (REACH), allowing clinics to participate in multiple value-based care initiatives simultaneously.
The Behavioral Health Imperative: Why GUIDE is a Natural Fit
The CMS GUIDE Model’s emphasis on holistic, person-centered care for dementia places behavioral health clinics squarely at the forefront of this initiative. Their expertise is not just complementary but essential for achieving the model’s goals.
Addressing Co-occurring Behavioral Health Conditions in Dementia
Individuals with dementia rarely present with cognitive impairment alone. Co-occurring behavioral health conditions are highly prevalent and often lead to significant distress for both the person with dementia and their caregivers.
Depression, Anxiety, Psychosis, Agitation: These are some of the most common and challenging behavioral symptoms. For example, up to 50% of individuals with Alzheimer’s disease experience depression, and anxiety disorders are also widespread. Psychosis and agitation can be particularly distressing, leading to increased caregiver burden and higher rates of emergency visits and institutionalization. Behavioral health professionals possess the diagnostic acumen and therapeutic skills (both pharmacological and non-pharmacological) to effectively assess and manage these symptoms.
The Link Between Behavioral Symptoms and Caregiver Strain: The presence and severity of behavioral symptoms directly correlate with caregiver strain and burnout. When behavioral health needs are unaddressed, caregivers face immense emotional, physical, and financial tolls. By providing expert behavioral health interventions, clinics can significantly alleviate this strain, improving the caregiver’s well-being and their capacity to provide care.
Enhancing Patient Quality of Life Through Integrated Care
Integrated behavioral and physical health care, as championed by the GUIDE Model, is critical for enhancing the overall quality of life for individuals with dementia.
Improved Mood and Function: Addressing depression, anxiety, and agitation can lead to a marked improvement in a person’s mood, sleep patterns, and overall engagement in daily activities. When behavioral symptoms are better managed, individuals with dementia can often maintain a higher level of function for longer, preserving their dignity and independence.
Reduced Hospitalizations and Emergency Department Visits: Unmanaged behavioral symptoms are a leading cause of avoidable hospitalizations and emergency department (ED) visits for people with dementia. These acute care settings are often disorienting and can worsen cognitive and behavioral symptoms. By providing proactive behavioral health interventions and crisis support within a comprehensive care framework, the GUIDE Model aims to reduce these costly and often traumatic events.
Empowering Caregivers as Essential Partners
Caregivers are the backbone of dementia care, and the GUIDE Model recognizes their critical role by mandating robust support. Behavioral health clinics are uniquely equipped to empower these essential partners.
By offering counseling, stress management techniques, and emotional support, behavioral health professionals can directly mitigate caregiver stress. Providing a safe space for caregivers to process their emotions, share their experiences, and learn coping strategies is invaluable for their mental health and resilience.
Behavioral health experts can train caregivers in effective communication techniques, behavior management strategies, and environmental modifications to de-escalate challenging behaviors. This empowers caregivers with practical tools, reduces frustration, and fosters a more positive and supportive care environment.
In essence, the GUIDE Model creates a formal pathway for behavioral health clinics to leverage their core competencies in a way that is financially sustainable and profoundly impactful for the dementia community.
How blueBriX Aligns with GUIDE Model Requirements
Successfully implementing the CMS GUIDE Model requires robust technological infrastructure that supports seamless coordination, comprehensive documentation, and effective patient and caregiver engagement. With over 15 years of experience in digital health, blueBriX offers a comprehensive suite of solutions specifically designed to meet and exceed the demanding requirements of the GUIDE Model.
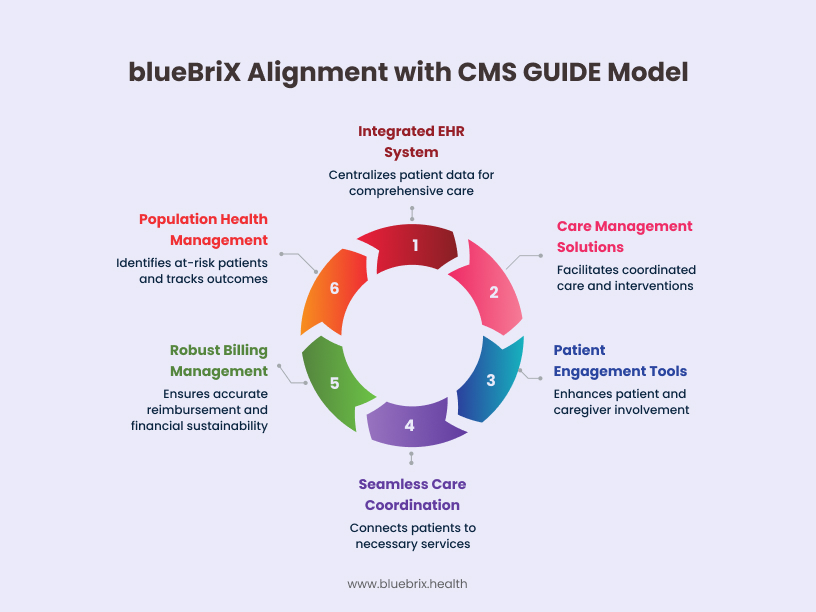
Integrated EHR System for Comprehensive Documentation
The foundation of any successful healthcare program is a reliable and integrated Electronic Health Record (EHR) system.
- Centralized Patient Records for Dementia and Behavioral Health: blueBriX provides a unified EHR platform that centralizes all patient data, including cognitive assessments, behavioral health evaluations (e.g., mood, agitation, psychosis), medication lists, physical health records, and social determinants of health. This eliminates data silos and ensures that every member of the interdisciplinary care team has a complete and current view of the patient’s condition, crucial for integrated dementia care.
- Streamlined Documentation for Assessments, Care Plans, and Progress Notes: Our EHR simplifies the documentation process, offering customizable templates for comprehensive assessments (including those specific to behavioral health), person-centered care plans, and progress notes. This streamlining ensures compliance with GUIDE Model reporting requirements while reducing administrative burden on your clinical staff.
Care Management Solutions for Coordinated Care
Effective care coordination is at the heart of the GUIDE Model, and blueBriX delivers powerful tools to facilitate this.
- Tailored Care Pathways for Dementia Patients with Behavioral Health Needs: blueBriX enables the creation of customized care pathways specifically designed for dementia patients with co-occurring behavioral health conditions. These pathways can incorporate specific behavioral interventions, psychiatric follow-ups, and social work consultations, ensuring that each patient receives targeted and appropriate care.
- Automated Reminders and Workflow Management for Interdisciplinary Teams: blueBriX platform offers automated reminders for appointments, medication adherence, and follow-up tasks, ensuring that no critical step is missed. Workflow management tools facilitate seamless communication and task assignment among psychiatrists, neurologists, social workers, care navigators, and other team members, promoting true interdisciplinary collaboration.
- Real-time Insights and Predictive Analytics for Risk Stratification: blueBriX’s analytics capabilities provide real-time insights into patient populations. This allows clinics to identify at-risk patients (e.g., those with escalating behavioral symptoms or high caregiver strain) and stratify their needs, enabling proactive interventions and preventing crises.
Patient Engagement & Caregiver Support Tools:
The GUIDE Model emphasizes strong patient and caregiver involvement, and blueBriX provides the digital tools to achieve this.
- Secure Patient and Caregiver Portals for Communication and Education: Our intuitive patient and caregiver portals offer a secure channel for communication with the care team, access to care plans, appointment schedules, and educational resources tailored to dementia and behavioral health. This empowers caregivers with information and fosters a sense of partnership in care.
- Remote Patient Monitoring for Behavioral Symptoms: blueBriX can integrate with remote patient monitoring (RPM) tools to track behavioral symptoms, sleep patterns, and activity levels. This provides valuable data to the care team, allowing for timely adjustments to care plans and early intervention for emerging issues.
- Customizable Digital Resources for Caregiver Training: We offer the flexibility to create and deliver customizable digital educational modules, videos, and guides for caregiver training, covering topics such as managing challenging behaviors, self-care strategies, and navigating community resources. This ensures caregivers receive consistent, high-quality education.
Seamless Care Coordination and Referrals:
Connecting patients and caregivers to necessary services is a core GUIDE requirement.
- Facilitating Referrals to Community-Based Services and Respite Providers: blueBriX streamlines the referral process, allowing clinics to easily connect patients and caregivers with a vetted network of community-based organizations, adult day centers, and respite care providers.
- Interoperability with External Systems for Holistic Care: Our platform is built with robust interoperability capabilities, allowing for secure data exchange with external systems used by specialists, hospitals, and other healthcare providers. This ensures a holistic view of the patient’s health journey and supports coordinated transitions of care.
Robust Billing and Revenue Cycle Management:
Navigating the GUIDE Model’s unique reimbursement structure requires precision.
- Ensuring Accurate Reimbursement for GUIDE Model Services: blueBriX’s revenue cycle management (RCM) features are configured to handle the specific billing codes and PBPM payment structure of the GUIDE Model. This ensures accurate claims submission and maximizes your clinic’s reimbursement for the comprehensive services provided.
- Optimizing Financial Performance Under Value-Based Care: Our RCM tools provide insights into financial performance, allowing clinics to track key metrics, identify areas for optimization, and ensure the financial sustainability of their GUIDE Model participation under a value-based care framework.
Population Health Management for Dementia Cohorts:
To truly impact the dementia population, a broader view is necessary.
- Identifying At-Risk Patients and Stratifying Needs: blueBriX’s population health management capabilities allow clinics to identify specific cohorts of dementia patients (e.g., those with high BPSD, frequent ED visits, or significant caregiver distress) and stratify their needs. This enables targeted interventions and resource allocation.
- Tracking Outcomes and Quality Metrics for Performance Reporting: Our platform provides comprehensive reporting tools to track key quality metrics and patient outcomes required by the GUIDE Model. This data is essential for performance-based adjustments, demonstrating the effectiveness of your program, and continuous quality improvement.
By leveraging blueBriX, behavioral health clinics can confidently meet the technological and operational demands of the CMS GUIDE Model, transforming their ability to deliver exceptional, integrated dementia care.
Preparing Your Clinic for the GUIDE Model: A Step-by-Step Approach
Embarking on the CMS GUIDE Model journey requires strategic planning and preparation. For behavioral health clinics, this means assessing current capabilities, understanding the application process, and embracing technology as a cornerstone of success.
Assess Your Current Dementia Care Capabilities
Before diving into the GUIDE Model, take stock of your existing resources and identify areas for growth.
Identify Gaps in Interdisciplinary Team, Care Coordination, and Caregiver Support:
- Interdisciplinary Team: Do you have access to or regularly collaborate with neurologists, geriatricians, and primary care providers? Are your current staff trained in dementia-specific behavioral health interventions? Pinpoint any missing expertise or roles that need to be filled or strengthened through partnerships.
- Care Coordination: How effectively do you currently coordinate care for patients with complex needs? Are there robust systems in place for communication between providers, tracking referrals, and managing follow-ups?
- Caregiver Support: What resources do you currently offer to caregivers? Is there a formal program for education, counseling, or respite referrals? The GUIDE Model places a high emphasis on caregiver support, so any deficiencies here will need to be addressed.
Understand the Application Process and Timeline
The GUIDE Model is a voluntary program, and participation requires a formal application. While the initial application window for GUIDE participants closed, it’s crucial to stay informed about any future opportunities or iterations of the model. CMS typically provides detailed Requests for Applications (RFAs) and supporting webinars. Leverage official CMS resources and industry updates to ensure you have the most current information regarding eligibility, requirements, and deadlines. Keep an eye on CMS Innovation Center announcements.
Leverage Technology for Seamless Implementation
Technology is not just an add-on; it’s a fundamental enabler for successful GUIDE Model participation.
Why a Platform like blueBriX is Crucial for Efficiency and Compliance:
The GUIDE Model demands comprehensive documentation, intricate care coordination, and robust reporting. Manual processes simply won’t cut it. A specialized digital health platform like blueBriX, with its integrated EHR, care management, and RCM capabilities, automates many of these processes. This dramatically improves efficiency, reduces the risk of errors, and ensures seamless compliance with all CMS requirements, from initial assessments to ongoing quality metric reporting. Our 15+ years of experience in digital health have taught us that a well-integrated system is the bedrock of value-based care.
Customization and Scalability for Your Clinic’s Needs:
Every clinic is unique. blueBriX’s modular and customizable nature means it can be tailored to your specific workflows and the size of your patient population. Whether you’re a small behavioral health practice or a large clinic looking to expand your dementia care services, our platform can scale with your needs, supporting sustainable growth within the GUIDE Model framework.
Training Your Team for Success
Technology is only as good as the people who use it. Comprehensive training is vital.
Adapting to New Workflows and Documentation Requirements:
The GUIDE Model introduces new care delivery components and reporting obligations. Your team will need training on new workflows, particularly around interdisciplinary collaboration, care navigation, and enhanced caregiver support. This includes understanding the specific documentation requirements for GUIDE, ensuring all necessary data is captured accurately and efficiently.
Utilizing blueBriX Training and Support:
When you partner with blueBriX, you’re not just getting a platform; you’re getting a team committed to your success. We provide comprehensive training programs and ongoing support to ensure your staff are proficient in using our system. This includes guided onboarding, user manuals, and responsive technical assistance, enabling your team to confidently adapt to the new demands of the GUIDE Model.
By systematically preparing your clinic, you can confidently embrace the CMS GUIDE Model, leveraging your behavioral health expertise to provide exceptional care to individuals with dementia and their families, while also securing your clinic’s growth and financial stability.