
Why is behavioral health billing considered complex? Well, it is because it is a substantially more challenging process to navigate than other types of healthcare billing. That is not to say that other specialties are not fraught with their own various complexities, because they are, it is to emphasize just how much more commitment is required from behavioral health billing.
The Complexities of Behavioral Health Billing
Behavioral health billing differs from other specialties in that the nature of the services provided and the course of treatment are not set variables for either the patient or the provider; neither is the timeline or the length of the treatment. This means that there is a much higher degree of risk involved when it comes to billing for it. For example, a 30-minute therapy session and a 45-minute therapy session might not seem like two drastically different services, but when filing claims and coding for the session, if the service provided isn’t accurately reported by the billing staff, it can have adverse outcomes for both patient and provider.
The provider might receive reduced reimbursement, or delayed reimbursement, or even a claim denial, which would put financial strain on the provider. Simultaneously, it is also an undesirable situation for the patient, who might face difficulties with their insurance coverage, which would lead to financial loss. This is why end-to-end collaboration is crucial for behavioral health billing; because it promotes communication and cooperation during each stage of the care giving process, resulting in a streamlined billing process that satisfies all involved.
What is End-to-End Collaboration in Billing?
End-to-end collaboration in billing means creating a strong connective thread between all involved in the process of treatment. This involves the psychiatrists, therapists, administrative staff, billing specialists, software providers, technology providers, and even the patient. The thread starts with the initial patient interaction, and it does not end until the final payment. The reasoning for this, as stated above, is to create a streamlined, efficient process that minimizes the possibility of errors being made.
Achieving this does require two key components to be implemented:
- Unified Data: Data must be managed in a unified manner, with all necessary patient health and treatment information, being accurately stored and easily accessible to all relevant stakeholders. Without this, the billing process cannot be completed correctly and efficiently.
- Communication: There must be open communication between stakeholders, whether it is in person or digitally, through channels that are secure and allows for clear exchange of information.
The Pitfalls of Siloed Billing Processes
Siloing information makes sense at first glance when it comes to healthcare data, but it is a destructive wrench that disrupts the billing process and creates a host of resulting problems, which compounds on each other. Ineffective communication of data leads to increased billing errors, which leads to delayed reimbursements or outright claim denials, which leads to cash flow issues. It also makes it more difficult for the provider to achieve compliance with regulations, which can result in serious penalties, such as fines, legal troubles, and even loss of license to practice.
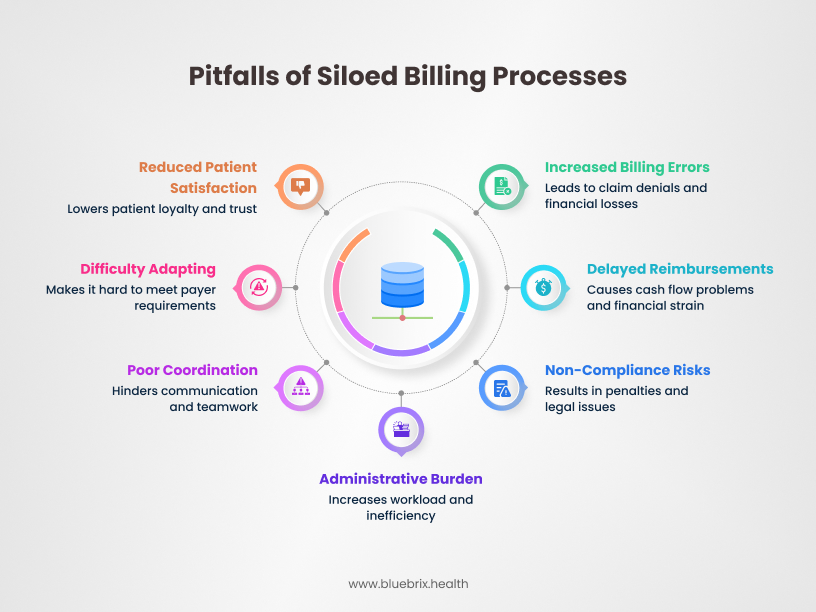
The administrative and billing staff are also burdened by a siloed billing process, as not having necessary information readily accessible would present a major difficulty in adapting to differing payer requirements, which could lead to inefficiencies and errors being made when filing claims, resulting in the staff needing to navigate the complexities of claims denials, as well as ensuring patient satisfaction does not suffer.
Benefits of End-to-End Collaboration
End-to-end collaboration can greatly improve the billing process. Reduction in inaccuracies or errors is one of the many benefits, thanks to data entry being streamlined. Less inaccuracies would lead to faster claims processing, negating the chance of claims denials, and accurate and appropriate reimbursement being received. This also benefits the practice from a compliance perspective, as they would not run the risk of not meeting regulations, which would have led to a variety of unwanted consequences.
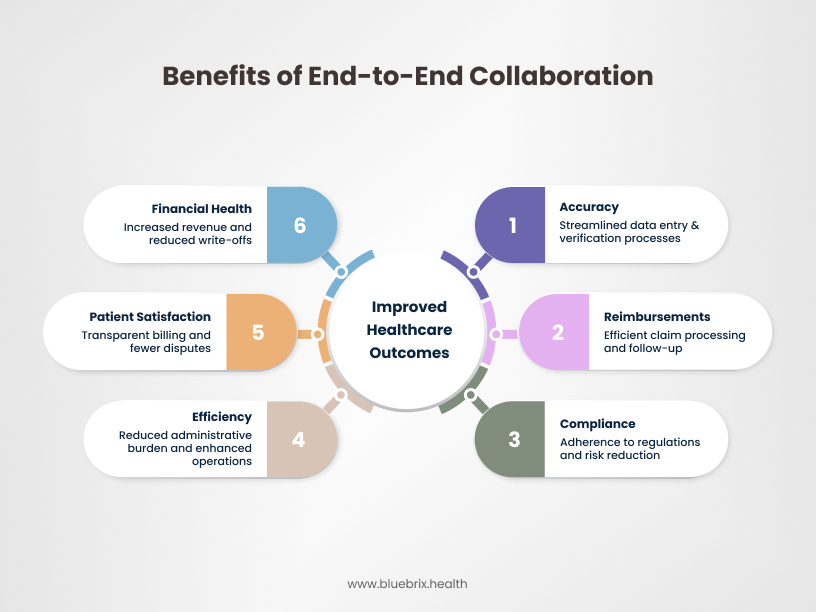
The administrative staff would also benefit from this manner of collaboration, because increased communication and coordination of patient health and treatment data would better inform them, thus improving their efficiency when going through the stages of the billing cycle. Simplified billing processes that are transparent and easy to understand would lead to fewer disputes with patients, as they would be well informed and would not have to deal with unexpected charges or insurance coverage issues, this would in turn enhance patient satisfaction and trust.
All of these would contribute to increased revenue and reduced write-offs, which would assist in improving the financial health of the practice.
Key Strategies for Implementing End-to-End Collaboration in Behavioral Health Billing
Effective end-to-end collaboration is not a luxury but a necessity for behavioral health organizations seeking financial sustainability, reduced denials, and improved patient access. These strategies provide a roadmap for achieving that collaboration:

Adopt Evidence-Based Models
Evidence-based practices (EBPs) are treatment interventions with proven effectiveness. Aligning billing processes with EBPs ensures that services delivered are reimbursable and defensible during audits. This requires clear documentation that reflects the EBP being used, including specific interventions, session duration, and progress toward goals. Studies show that documentation that clearly reflects EBPs is less likely to be denied by payers. For example, accurate coding and documentation of Cognitive Behavioral Therapy (CBT) or Dialectical Behavior Therapy (DBT) sessions are crucial. Many payers are increasingly emphasizing value-based care, which prioritizes outcomes achieved through EBPs. Failure to adhere to EBP documentation guidelines can lead to significant revenue loss and potential legal repercussions. Clinicians must accurately document EBPs, and billing staff must understand these practices to code and bill correctly. Regular training sessions involving both teams are essential.
Integrated Technology Solutions: Practice Management and EHR Systems
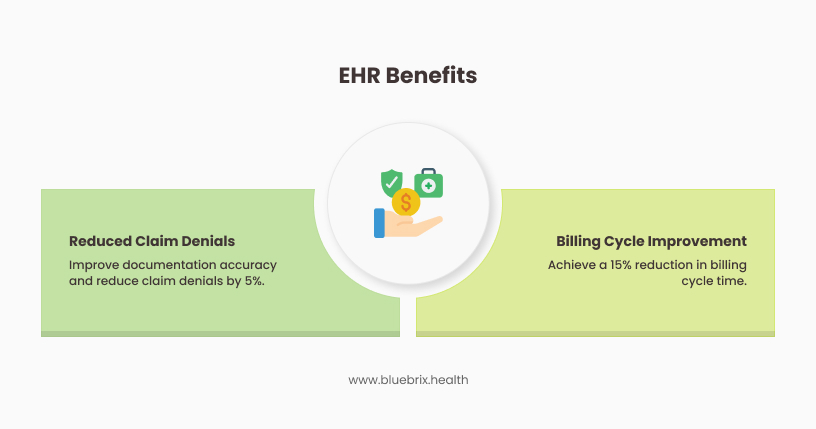
Integrated practice management (PM) and electronic health record (EHR) systems are the backbone of end-to-end collaboration. These systems streamline data flow, reduce manual errors, automate tasks, and improve communication between clinical and administrative staff. Key functionalities include electronic claims submission, real-time eligibility verification, automated coding assistance, and integrated reporting. According to industry reports, practices using integrated EHR/PM systems experience a significant decrease in claim denials (up to 25% reduction) compared to those using separate systems. Automation features within integrated systems can reduce administrative costs by streamlining tasks like claims submission and payment posting. Real-time eligibility verification helps prevent denials due to coverage issues, improving the clean claims rate. Clinicians input data into the EHR, which is then used by the PM system for billing. Seamless data transfer is crucial. Regular meetings between clinical and administrative staff to optimize system use are vital.
Prioritize Measurement-Based Care (MBC)
MBC involves systematically collecting and using patient-reported outcome measures (PROMs) and clinician-rated outcome measures to inform treatment and track progress. Integrating MBC into billing workflows ensures that reimbursement is tied to clinical outcomes, supporting value-based care models. Payers are increasingly interested in reimbursing for services that demonstrate positive outcomes. MBC provides the data to support this. Studies have shown that incorporating MBC into practice can improve treatment effectiveness and patient engagement. MBC data can also be used to justify service necessity and support appeals for denied claims. Clinicians collect and document outcome measures, and billing staff use this data to support claims and negotiate contracts with payers. Data analysis and reporting require close collaboration.
Establish Cross-Disciplinary Teams
Create teams that include clinicians, billing specialists, administrative staff, and potentially IT personnel. These teams should meet regularly to discuss billing-related issues, share best practices, and develop solutions to common problems. Cross-disciplinary teams foster a shared understanding of the billing process and its impact on clinical care and financial stability. Regular meetings improve communication and reduce the likelihood of errors or misunderstandings. Team-based approaches can lead to innovative solutions for complex billing challenges. Regular meetings, shared communication platforms, and clearly defined team goals are essential.
Define Roles and Responsibilities: Ensuring Accountability Across the Billing Cycle
Clearly define the roles and responsibilities of each team member involved in the billing cycle, from intake and registration to claims submission and payment posting. Document these responsibilities in standard operating procedures (SOPs) to ensure accountability and consistency. Ambiguous roles and responsibilities can lead to errors, delays, and lost revenue. SOPs provide a framework for consistent and efficient billing practices. Regular performance evaluations can help ensure that individuals are meeting their responsibilities. All team members must understand their roles and how they contribute to the overall billing process. Training and ongoing communication are key.
Strengthen Patient and Family Engagement
Involve patients and families in the billing process by providing clear and transparent information about costs, insurance coverage, and payment options. Offer patient portals for online bill pay and communication. Address any billing concerns promptly and empathetically. Clear communication reduces patient confusion and dissatisfaction with billing. Offering convenient payment options improves collection rates. Proactive communication can prevent disputes and maintain positive patient relationships. Front desk staff, clinicians, and billing staff all play a role in patient communication. Consistent messaging and a patient-centered approach are crucial.
Optimize Reimbursement Structures
Alternative payment models or APMs are becoming increasingly common in behavioral health. Proactive monitoring of payer policies helps prevent denials and maximize reimbursement. Negotiate favorable contracts with payers based on the value of services provided and the outcomes achieved. Explore APMs that incentivize quality and efficiency. Stay informed about changes in payer policies and coding guidelines. Effective contract negotiation can significantly impact revenue. Billing staff, administrators, and clinicians should collaborate on contract negotiations and APM implementation. Data analysis is essential.
Address Social Determinants of Health (SDOH)
Recognize that SDOH (e.g., poverty, housing instability, lack of access to transportation) can impact a patient’s ability to access and engage in care, which can, in turn, affect billing. Collaborate with community resources and other healthcare providers to address SDOH and improve patient outcomes. SDOH can contribute to higher no-show rates, treatment non-adherence, and ultimately, billing challenges. Payers are increasingly recognizing the importance of addressing SDOH. Collaborating with community partners can improve access to care and reduce billing-related barriers. Clinicians identify SDOH, and care coordinators or administrators work with community resources. Billing staff should be aware of how SDOH affects patient access and engagement.
Standardize Communication Protocols
Establish clear communication protocols for all team members involved in the billing cycle. This includes how to escalate issues, where to document communication, and what information to share. Utilize communication tools within the EHR/PM system to track and document interactions. Clear protocols prevent misunderstandings and ensure timely resolution of issues. Documenting communication provides an audit trail and improves accountability. Efficient communication tools enhance collaboration and reduce delays. All team members must adhere to the established protocols. Regular training and reinforcement are necessary.
Regular Training and Updates: Billing Procedures and Regulations
Provide ongoing training to all staff on billing procedures, coding guidelines, payer policies, and regulatory changes. This training should be tailored to specific roles and responsibilities. Keep staff updated on changes in technology, such as EHR/PM system updates. The billing landscape is constantly evolving, so ongoing training is essential. Well-trained staff are less likely to make errors and more likely to follow best practices. Training on new technology ensures that staff can use the systems effectively. Billing experts, compliance officers, and system administrators should collaborate to develop and deliver training. Feedback from staff should be incorporated into training programs.
By implementing these key strategies, behavioral health organizations can foster a culture of end-to-end collaboration, leading to improved billing efficiency, reduced denials, increased revenue, and ultimately, better patient care.
How does technology facilitate behavioral billing collaboration?
Let’s face it: behavioral health billing can be a beast. It’s complex, it’s detail-oriented, and when things go wrong, it impacts both your bottom line and your ability to provide care. But here’s the good news: technology is a game-changer. It’s not just about automating tasks; it’s about fostering real collaboration between your clinical and administrative teams.
Electronic Health Records (EHRs) Streamlining Documentation and Billing
EHRs are more than just digital filing cabinets. In behavioral health, they’re the central hub for all patient information, and that’s huge for billing.
- What EHRs do:
- They standardize documentation. Think about it: when everyone uses the same templates and workflows, it’s much easier to capture the details needed for accurate coding. This reduces errors and denials.
- They improve communication. Clinicians can enter notes, treatment plans, and diagnoses directly into the EHR, and billing staff can access that information instantly. No more chasing down paper charts or playing phone tag!
- They automate coding. Many EHRs have built-in coding tools that suggest the correct codes based on the documentation. This saves time and minimizes coding errors.
- Why this matters for collaboration:
- EHRs create a shared source of truth. Everyone is on the same page, which reduces misunderstandings and disputes.
- They free up time. Clinicians spend less time on paperwork, and billing staff spend less time on data entry and error correction. This allows everyone to focus on their core responsibilities.
Integrated Billing Software for Automation and Tracking
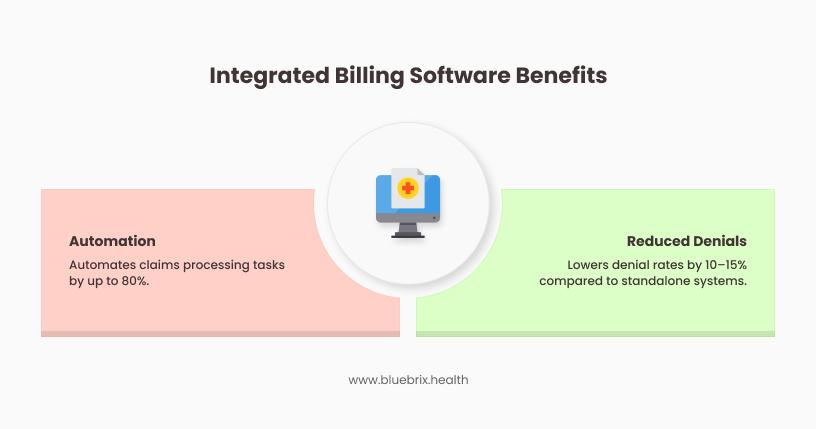
Standalone billing systems are so last decade. Integrated billing software, especially when combined with an EHR, is where the magic happens.
- What integrated billing software does:
- It automates claims processing. From eligibility verification to claims submission to payment posting, many tasks are automated, reducing manual effort.
- It provides real-time tracking. You can see the status of every claim, identify bottlenecks, and track key performance indicators (KPIs) like denial rates and days in accounts receivable.
- It improves revenue cycle management. Integrated systems give you a holistic view of your financial health, allowing you to optimize your revenue cycle and maximize collections
- Why this matters for collaboration:
- Automation reduces errors and speeds up the billing process, which means faster payments and fewer headaches for everyone.
- Real-time tracking gives everyone visibility into the billing process, so you can identify and address issues proactively.
- Improved revenue cycle management means a healthier bottom line, which benefits the entire organization.
AI-Aided Solutions for Billing Accuracy
Artificial intelligence (AI) is no longer a futuristic concept; it’s already transforming healthcare, including billing.
- What AI-aided solutions can do:
- AI can analyze claims in real-time to identify potential errors before they’re submitted, significantly improving accuracy.
- AI can automate prior authorizations, which is a major pain point in behavioral health billing.
- AI can predict denial patterns, allowing you to proactively address the root causes of denials.
- Why this matters for collaboration:
- AI reduces the burden on billing staff, freeing them up to focus on more complex tasks.
- AI improves billing accuracy, which reduces denials and increases revenue.
- AI provides data-driven insights that can help improve billing processes and collaboration.
Technology is not just about making billing easier; it’s about making it better. It’s about empowering your teams to work together more effectively, so you can focus on what matters most: providing quality care to your patients.
The Bottom Line: Invest in Collaborative Billing for a Thriving Behavioral Health Practice
Summit it up, the power of end-to-end collaboration cannot be overstated in the intricate landscape of behavioral health, where compassionate care meets complex reimbursement. It’s more than just a smoother workflow; it’s the bedrock of a healthier, more sustainable practice.
By fostering synergy between clinical and administrative teams, collaborative billing leads to key benefits for a behavioral health practice: reduced denials and increased revenue, improved operational efficiency, enhanced compliance, better patient experience, and data-driven insights for strategic growth.
Ready to Transform Your Behavioral Health Billing and Cultivate a Healthier Practice?
Don’t let fragmented processes hinder your ability to provide exceptional behavioral health care and achieve financial stability. Investing in end-to-end collaboration is an investment in your practice’s future.