Billing for group therapy isn’t as straightforward as it seems. While many assume it’s a one-size-fits-all process, the reality is that payer requirements, documentation standards, and compliance regulations make it far more complex than individual therapy billing. This guide explores key strategies, best practices, and how Behavioral Health EHR systems can optimize your workflow for success.

Mastering the Complexities of Group Therapy Billing
Billing for group therapy isn’t just about submitting the right codes—it’s about understanding the intricacies of insurance policies, compliance standards, and documentation workflows to maximize reimbursements while minimizing denials. Unlike individual therapy, group therapy billing presents unique challenges such as logistical hurdles like scheduling and note-taking for large groups that require a strategic approach, especially when integrated with a Behavioral Health Electronic Health Record (EHR) system. Let’s dive into the common pain points, best practices, and how Behavioral Health EHR solutions can revolutionize your group therapy billing process.
Why Group Therapy Billing is More Complex than Individual Therapy
At first glance, group therapy billing might seem simpler—just one CPT code (90853) for all participants, right? Not quite. Here’s what makes it more challenging:

- Seamless Scheduling for Multiple Stakeholders: Coordinating group sessions across clinicians, subordinate staff, and 20–30 patients is no small feat. Without integrated scheduling tools in your Behavioral Health EHR that sync across calendars, appointment clashes and patient no-shows become inevitable. Behavioral Health EHRs with shared visibility, appointment reminders, and batch rescheduling capabilities can solve this pain point.
- Bulk Documentation with Individual Precision: For every group whether 5 or 10 or 30 or more, the clinician must simultaneously document session-wide activities and create individualized notes that reflect each participant’s engagement, progress, and billing requirements. Without a system that allows for group notes with patient-specific overlays, clinicians may either duplicate effort or miss essential details.
- Preauthorization & Eligibility Checks: Many insurers require preapproval for group therapy. Managing this at scale becomes overwhelming without automated checks built into your system.
- Diverse Payer Requirements: Not all insurers handle group therapy the same way. Some limit group size, session frequency, or require modifiers like GT (telehealth) or 59. While 90853 is the standard code, some insurers impose session duration limits, restrict group sizes, or require additional modifiers. Your Behavioral Health EHR should adapt documentation and claims logic based on payer-specific rules.
- One Session, Multiple Claims: A single group session generates multiple claims—each with its own potential for denial. Multiply this by 30 participants, and the margin for error skyrockets.
- Documentation Compliance: Unlike individual therapy, where notes focus on one patient, group therapy notes must reflect participation levels, engagement, and individualized progress. Payers demand proof of individualized care, even in a group setting. Generic summaries often trigger denials or audits.
- High Denial Rates: The reason that blueBriX as an organization always stresses the importance of pre-authorization, coding and meeting compliance and requirements is because not meeting those markers are what leads to practices getting their claims denied. This stays even more true when it comes to group therapy, where meeting those markers is more challenging, and thus leads to higher denial rates.
- Administrative Burden: In the points above, we’ve stressed the complexity of managing group billing. In the absence of a capable Revenue Cycle Management software or group, the stress of handling group billing would fall upon the administrative staff.
- Variability in Treatment Approaches: The approach taken towards treatment, even in a therapeutic group setting, can vary depending upon who is leading the group. This can cause difficulties in billing, as there in no one size fits all procedure to hold up as the standard.
- Stigma and Patient Engagement: There is still a stigma associated with searching for assistance in dealing with mental health issues, and in patients for whom this is a significant problem, a group setting might dissuade them from actively engaging and thus wouldn’t benefit their health outcomes positively.
- Compliance with Regulations: Compliance must be met (with both state and federal regulations) to receive reimbursement; this stays true for group therapy as well.
Without an optimized workflow, these challenges can lead to claim rejections, audits, and revenue loss.
Best Practices for Streamlined Group Therapy Billing
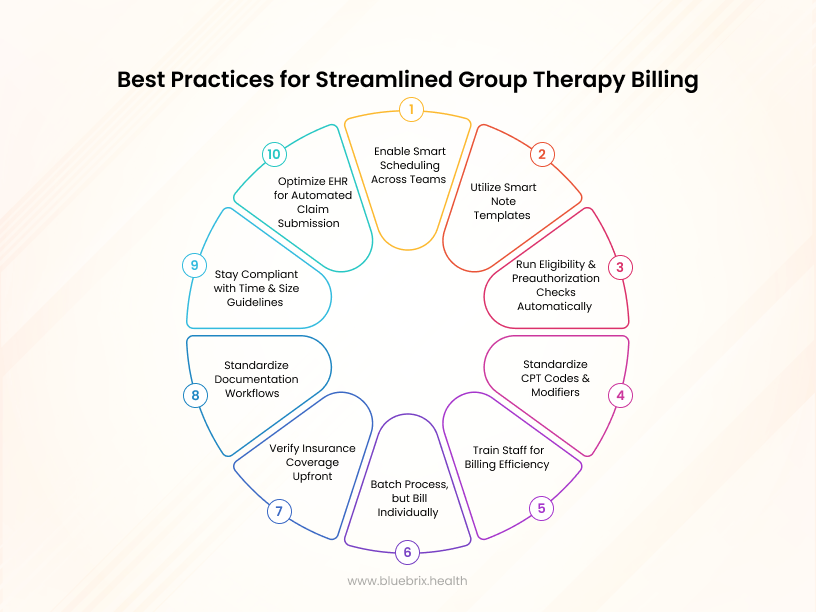
- Enable Smart Scheduling Across Teams
- Use a Behavioral Health EHR that supports multi-user scheduling with drag-and-drop interfaces, batch session creation, calendar syncing, and automated reminders to reduce no-shows and coordination chaos.
- Empower subordinates to manage these tasks independently with defined permissions and visibility controls.
- Utilize Smart Note Templates
- Choose Behavioral Health EHR systems that let clinicians input shared session data once, then auto-generate individual notes with customizable fields.
- Notes should be compliant with payer guidelines—detailing patient-specific insights like participation level and therapeutic response.
- Run Eligibility & Preauthorization Checks Automatically
- Build pre-check workflows into your intake process. This ensures that coverage issues don’t arise after the session has occurred.
- Standardize CPT Codes & Modifiers
- Use 90853 (group therapy), 90849 (multi-family), and apply modifiers as per payer instructions.
- Create payer-specific profiles in your Behavioral Health EHR to automate code logic during claim generation.
- Train Staff for Billing Efficiency
- Schedule monthly training on payer updates, denial trends, and Behavioral Health EHR usage.
- Introduce peer learning forums or quick-help resources within your workflow tools.
- Batch Process, but Bill Individually
- A powerful Behavioral Health EHR should allow batch entry of shared data with branching logic for individual claims—reducing manual repetition without compromising specificity.
- Verify Insurance Coverage Upfront
- Run eligibility checks for all participants before they attend the session.
- Confirm whether insurers limit the number of group sessions per year.
- Standardize Documentation Workflows
- Use Behavioral Health EHR templates designed for group therapy progress notes to save time.
- Maintain individualized notes, attendance, patient progress etc.—generic session summaries often trigger claim denials.
- Stay Compliant with Time and Size Guidelines
- Sticking to guidelines pertaining to the group size and session length is necessary to avoid denied claim filings.
- Meeting compliance, at both state and federal levels, protects the provider from legal and financial threats.
- Optimize Behavioral Health EHR for Automated Claim Submission
- Choose an Behavioral Health EHR system that auto-populates billing fields to reduce manual errors.
- Set up batch claim processing to handle multiple patients simultaneously.
Can Behavioral Health EHR Solutions simplify Group Therapy Billing?
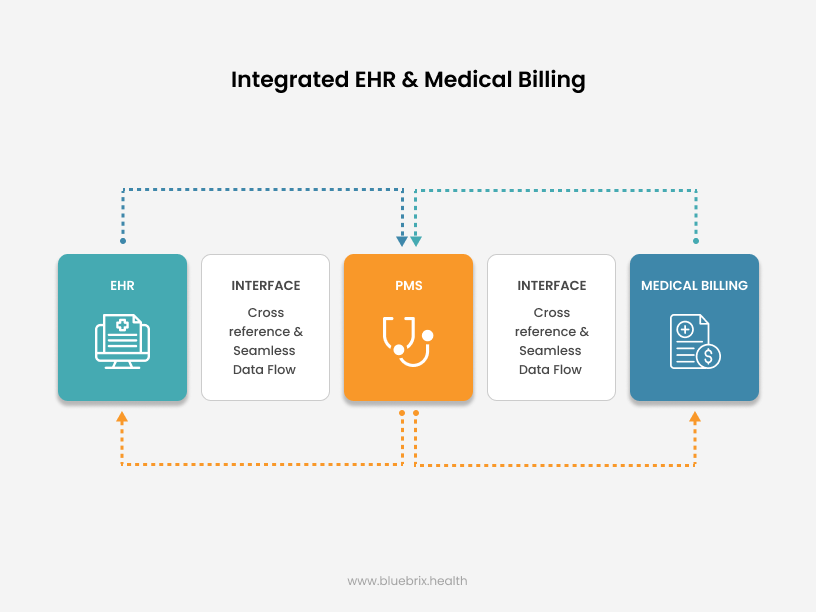
Yes—but only if they’re purpose-built for behavioral health. EHR systems offer a bevy of benefits that can greatly assist in billing for group therapy. These include more accurate claim filings, better documentation of patient and treatment information, as well as reducing administrative burnout and workload, which can improve resource management and usage. Here’s how an optimized Behavioral Health EHR can transform your group therapy billing:
- Automated CPT Code Selection – Reduces coding errors by linking the right CPT code to the session type.
- Prebuilt Documentation Templates – Ensures compliance by guiding clinicians on payer-specific requirements.
- Batch Billing with Claim Customization Features – Allows bulk claim submissions with options to edit specific claims for group therapy sessions.
- Integrated Eligibility and Pre-auth Workflows – Automates insurance checks and authorization processes before group sessions to prevent billing denials.
- Claim Tracking Dashboards – Provides real-time insights into denied claims and resubmission workflows.
- Shared-Session Note Templates with Individual Fields – Allows clinicians to document shared group details once while customizing notes for each participant individually.
- Split-View Note Entry for Group Participants – Enables simultaneous viewing and editing of multiple participant notes side-by-side during or after a group session.
- Real-Time Claim Status and Rejection Alerts – Instantly notifies staff of claim approvals, rejections, or issues to accelerate resolution and reduce revenue delays.
Selecting the right Behavioral Health EHR partner can mean the difference between an efficient billing cycle and constant revenue leakage.
Compliance & Legal Considerations in Group Therapy Billing
With increased payer scrutiny, compliance is non-negotiable. Protect your practice by:
- Ensuring HIPAA-compliant documentation – Avoid using shared patient records; each participant must have their own entry.
- Following insurer-specific supervision requirements – Some payers require a licensed therapist to lead the session, while others allow co-facilitators. There could be multiple supervision models depending on your state/payer (solo facilitator, co-facilitators, etc.).
- Maintaining detailed session records – In case of an audit, progress notes should substantiate medical necessity, attendance, time, session-specific outcomes etc.
- State and Federal Regulations – As we’ve stated earlier in this article, regulations are constantly being updated, with old ones being modified and new ones being introduced. Keeping abreast of these changes ensures successful billing cycles.
The Future of Group Therapy Billing: What to Expect
As the healthcare industry shifts toward value-based care models, group therapy billing will undergo significant changes. Here are some key trends to watch:
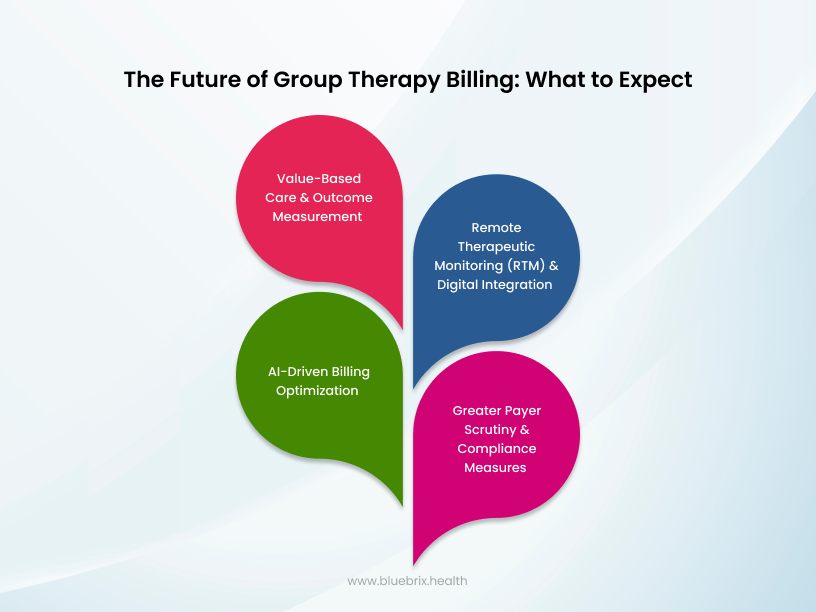
- Value-Based Care and Outcome Measurement
- Payers are moving away from fee-for-service models toward value-based reimbursement, meaning providers will be compensated based on patient outcomes rather than just services rendered.
- Expect more stringent documentation requirements that track individual progress within group settings, potentially requiring standardized outcome measurement tools.
- Behavioral Health EHR systems with built-in analytics and patient-reported outcomes tracking will become essential.
- Remote Therapeutic Monitoring (RTM) and Digital Integration
- RTM codes (e.g., CPT 98975-98978) are gaining traction, allowing clinicians to bill for monitoring patients’ mental health progress remotely through wearables, apps, or telehealth platforms.
- Group therapy providers can leverage RTM to track engagement levels, symptom progression, and adherence to therapy outside of sessions, potentially opening new billing opportunities.
- Insurers may begin integrating blended in-person and virtual therapy sessions as part of reimbursement models.
- AI-Driven Billing Optimization
- Artificial intelligence and automation in Behavioral Health EHR platforms will help reduce coding errors, identify claim risks, and ensure compliance with evolving payer policies.
- AI-driven natural language processing (NLP) tools will make documentation easier by generating real-time therapy notes based on verbal interactions.
- Greater Payer Scrutiny and Compliance Measures
- As billing fraud concerns increase, payers will implement stricter audits for group therapy claims.
- Providers will need to demonstrate medical necessity through robust documentation, including individual progress reports within group settings.
Final Thoughts
The landscape of group therapy billing is evolving. Teletherapy, AI-driven billing automation, and regulatory changes will continue shaping the field. Forward-thinking behavioral health practices are already leveraging advanced behavioral health EHR capabilities to stay ahead of industry trends.
Investing in billing automation, ongoing staff training, and payer-specific knowledge is no longer optional—it’s essential for sustainability and growth.
By refining your group therapy billing process and adopting Behavioral Health EHR-powered efficiencies, your practice can focus more on delivering quality care—without being bogged down by administrative burdens.
Is your practice struggling with group therapy billing inefficiencies? Consider upgrading to blueBriX, an EHR system designed for behavioral health to streamline workflow, ensure compliance, reduce denials, and enhance revenue cycles.