Measurement-Based Care (MBC) has become the gold standard for modern behavioral health transforming intuition into evidence and guesswork into precision. By consistently tracking standardized tools such as the PHQ‑9 or GAD‑7, clinicians can monitor progress in real time, adjust treatment plans early, and detect when a patient’s condition is worsening before it turns into a crisis. Studies show MBC leads to faster recovery, fewer relapses, and more confident clinical decisions.
Despite its proven impact, fewer than 20% of clinicians use MBC consistently. The problem isn’t belief—it’s bandwidth. Manual data entry, disconnected systems, and clunky workflows make ongoing measurement feel like extra work instead of integrated care. Over time, the burden outweighs the benefit, and many providers revert to “business as usual.” Streamlined, automated technology is essential to make MBC sustainable and bring its precision-driven promise to everyday practice.
In this blog, we’ll look at what separates the 20% who scale MBC successfully from the 80% who stall, and what it really takes to make outcomes measurement sustainable at scale.
What trips up the 80%: three reasons MBC fails in most practices
Even with the best intentions, behavioral health programs struggle to reap the full value of Measurement-Based Care. MBC promises better patient outcomes and more efficient operations—but only when the right systems and processes support it. Too often, clinicians and administrators hit hidden obstacles: slow workflows, data trapped in silos, and insights that never turn into action. When these challenges persist, MBC stops being a powerful clinical tool and becomes just another source of frustration.
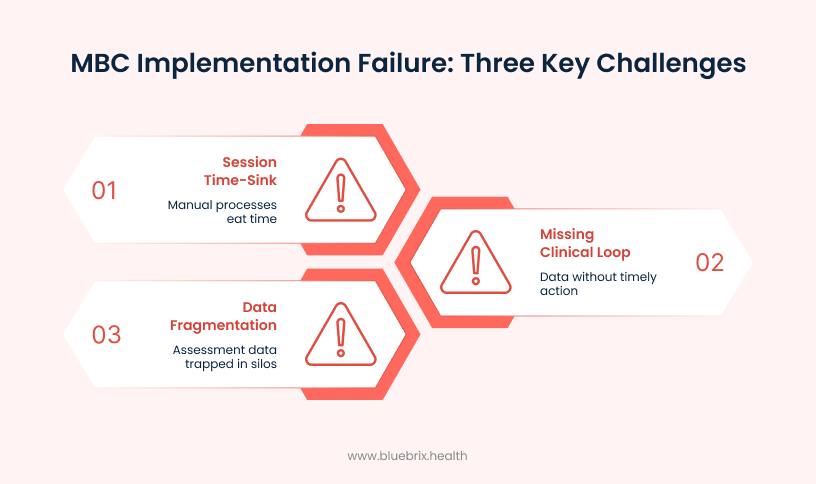
Here’s how these obstacles show up in real-world practice:
Trap 1: the session time-sink
The problem: manual processes eat into limited therapy time
Behavioral health providers typically have just 45 minutes per session to deliver care and complete required administrative tasks for Measurement-Based Care. Using paper forms to track symptoms, manually scoring assessments, and re-entering data into EHRs takes up valuable minutes that could be spent with patients. These repetitive tasks create a workflow bottleneck that makes it nearly impossible to implement MBC effectively while managing a full caseload.
The clinician’s dilemma: documentation vs. Connection
The therapeutic relationship is the foundation of effective behavioral health treatment, but MBC requirements force clinicians to choose between completing paperwork and building rapport with patients. When therapists are focused on filling out forms and entering scores, sessions become transactional instead of relational—reducing opportunities for the trust and empathy that drive healing. This constant tension between documentation demands and meaningful patient connection leads to provider stress and burnout, undermining the very core of quality behavioral health care.
Trap 2: the data fragmentation black hole
The problem: assessment data trapped in silos
You’ve collected the data, but is it actually movable? Most assessment data from MBC ends up scattered across disconnected systems—stored as PDFs in EHRs, buried in spreadsheets, or lost in separate files. This valuable information sits isolated and inaccessible, making it impossible for providers to track patient progress over time or identify meaningful trends. Instead of a complete picture, critical insights remain fragmented and hidden.
The administrative consequence: no big picture reporting
When data is fragmented, administrators and clinical leaders can’t generate reports to demonstrate program effectiveness or patient improvement across their organization. Without clear, aggregated information, it becomes impossible to prove the value of care to payers, secure funding, or make informed quality improvement decisions. Instead of actionable insights, they’re left with disconnected pieces that don’t tell a coherent story about outcomes or impact.
Trap 3: the missing clinical loop
The problem: data without action
Measurement-Based Care only works when data drives timely action. In manual or fragmented systems, providers don’t get alerts when a patient’s condition worsens or stalls, so warning signs slip through the cracks. Without real-time notifications, MBC data sits unused and recorded but never acted upon. Providers miss chances to adjust treatment or escalate care when it matters most, turning MBC into a compliance checkbox instead of a clinical tool. When clinicians don’t see tangible benefits, engagement drops and MBC loses its purpose.
The abandonment point: losing the clinical value
When MBC processes are cumbersome and the data doesn’t lead to real action, clinicians start treating it like just another paperwork task instead of a tool that actually improves care. It becomes a checkbox to satisfy audits rather than something that helps catch warning signs early or guides treatment decisions.
Now, you have a clear view of the real reason behind MBC implementation failure—not having the right tech partner. That’s exactly what separates the struggling majority from the thriving 20%. So what did these successful programs find in their technology partner that made all the difference? Let’s find out.
The tech-enabled solution: how the 20% thrive with a purpose-built behavioural health ehr
While most providers struggle with administrative tasks—documentation, manual scoring, and hunting for data—the winning few have already cracked the code. The difference? A purpose-built behavioural health EHR designed specifically for behavioral health workflows. Here’s how blueBriX transforms the three biggest time drains into seamless, automated processes that put clinical care back at the center of your day.
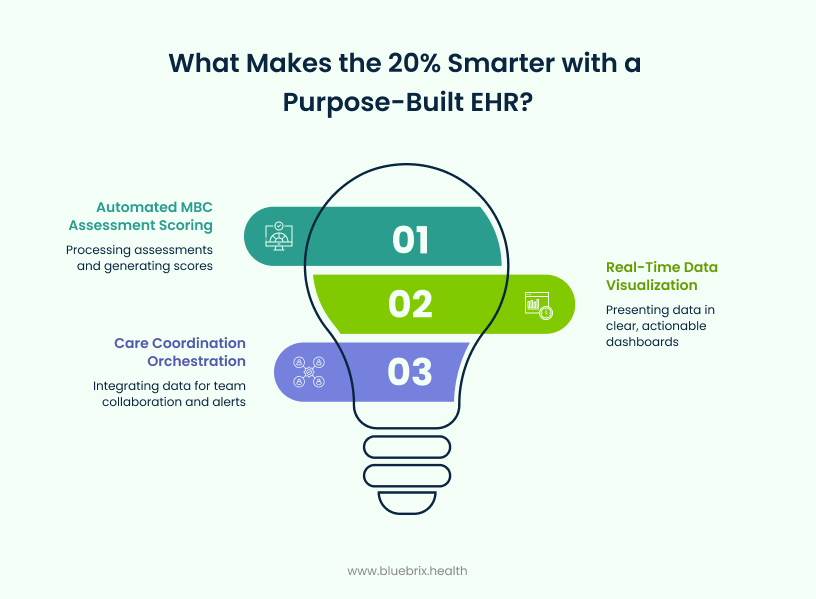
Solving time drains with seamless patient engagement
Your sessions with patients shouldn’t feel like checking off boxes—they should be interactive, where your patient feels heard, understood, and genuinely cared for. blueBriX understands this, which is why we shift key tasks outside the appointment. Automated reminders prompt your patients to complete assessments like PHQ-9 or GAD-7 through a simple portal or app before they arrive.
The system instantly scores these assessments and sends results straight to your dashboard—no manual scoring, no hunting for information. You walk into sessions with everything you need already at your fingertips, ready to focus on connection instead of paperwork.
Bridging fragmented data through real-time visualization
Data isn’t useful if it’s buried in PDFs or scattered across different systems. You need to see the full picture quickly, especially when time is limited and decisions matter. With blueBriX’s visual dashboards integrated directly into your clinical chart, raw patient data becomes clear, actionable insights at a glance.
No more digging through pages of notes. Instead, you can review a patient’s entire journey in seconds—tracking progress over weeks or months instantly. This makes it easier to have meaningful conversations with patients about their progress and collaborate on next steps, rather than spending valuable session time piecing together fragmented information.
Closing the care loop with a care coordination orchestration platform
Analytics from Measurement-Based Care (MBC) data can’t be useful if it is not delivered to the right people at the right time. blueBriX is a next-generation platform built for whole-person care that integrates MBC seamlessly into its care coordination orchestration. It combines real-time MBC data analysis, automated task routing, and intelligent alerts, ensuring clinicians, care managers, and care teams receive actionable MBC insights exactly when needed.
For instance, when a patient’s depression questionnaire reflects severe symptoms, the platform generates a high-priority alert that immediately notifies the care coordinator to review the case. The coordinator then assigns follow-up tasks—such as adjusting the treatment plan to the therapist or scheduling a medication review with the psychiatrist—while enabling secure communication among the team to align on next steps. Meanwhile, the patient may receive automated outreach to keep them engaged in care.
By providing each team member with interpreted, prioritized MBC data, blueBriX drives proactive care and early prevention, closing care gaps before crises escalate. Through this precise coordination and task management, blueBriX transforms measurement-based care from static data collection into a scalable, actionable process that optimizes treatment outcomes and enhances collaborative care delivery.
The strategic benefits of sustainable measurement-based care
When measurement-based care moves from aspiration to daily practice, the benefits extend far beyond individual appointments. You’re not just saving time—you’re transforming how your practice operates, how you manage risk, and how you prove value to payers and stakeholders.

Reducing risk and preventing burnout
Automation handles heavy lifting – collecting, scoring, and flagging patient data automatically. This frees you from manual tracking and interpretation, reducing cognitive load and the stress that fuels burnout.
When a patient’s scores signal worsening depression or suicidal ideation, you get an immediate alert without having to dig through assessments yourself. You can focus your energy on patient care instead of paperwork, improving both your well-being and patient safety.
Vbc readiness and payer compliance
As healthcare shifts toward Value-Based Care, payers want proof that your treatments work and patients are improving. Regular, reliable measurement-based care data is how you demonstrate quality and justify reimbursement.
Automated MBC collection ensures you have the consistent data needed to meet payer compliance requirements, support contract negotiations, and qualify for outcome-based incentive payments. You have everything documented and ready, making it easier to prove your program’s value and secure better contracts.
Scaling programmatic excellence
If you’re running multiple programs like substance use disorder treatment, IDD services, intensive outpatient, or standard outpatient care—MBC data lets you compare outcomes across the board. You can see what’s working, where, and for whom.
This insight drives smarter decisions. Maybe your data shows a particular therapy approach is especially effective in your intensive outpatient program—so you expand it there while trying something different for standard outpatient services. Instead of guessing what works, you’re refining programs based on real evidence. This data-driven approach helps you scale what’s successful and continuously improve care across your organization.

