If you’re running a behavioral health practice today, you already know the demand for care is skyrocketing. Caseloads are up, regulations are heavier, and patients need more than a quick prescription and discharge. Yet too many practices are still running on EHR systems that were built with primary care in mind.
And that’s where the trouble starts. Sure, those systems are fine for tracking blood pressure and lab results. But try documenting a group therapy session or managing consent under 42 CFR Part 2 and suddenly you’re back to spreadsheets, sticky notes, or endless copy-pasting.
I’ve heard clinicians call it “death by template.” Notes that don’t fit. Workflows that make no sense. Admins chasing compliance with half-baked access controls. It’s like forcing a square peg into a round hole, frustrating, time-consuming, and risky.
The truth is, a generic EHR doesn’t just slow you down. It leaves gaps:
- in compliance
- in data
- and worst of all, in patient care.
Your system should be helping you run smoother, not piling more stress onto already stretched teams.
If any of the next four red flags sound familiar, it’s a sign your EHR isn’t working for behavioral health and it’s time to rethink what you’re running on.
Red flag 1: the documentation treadmill
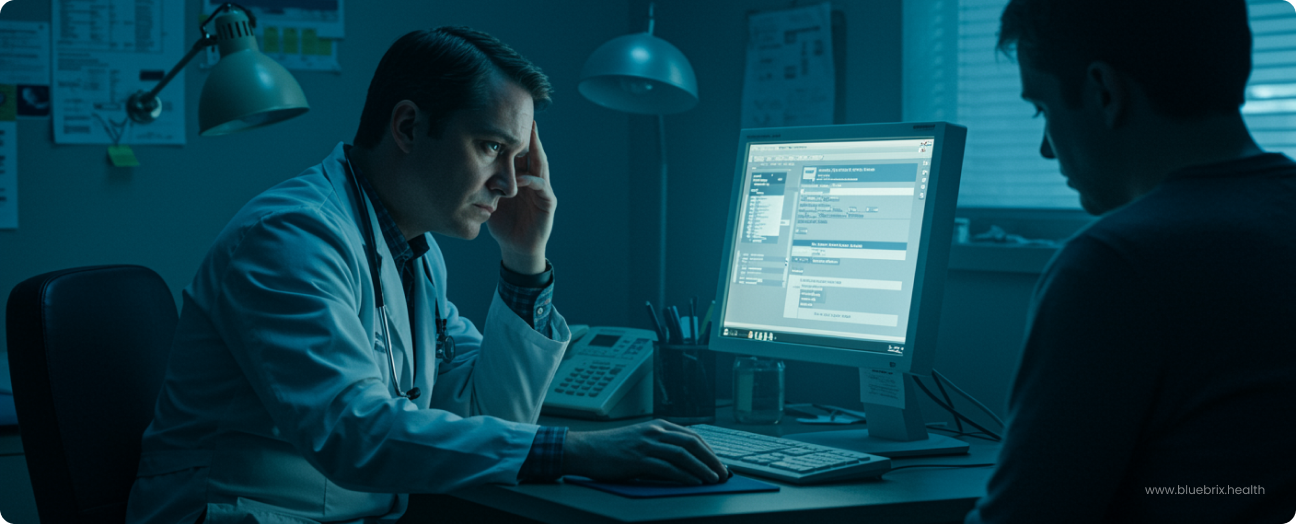
What is the documentation treadmill in behavioral health EHRs? The documentation treadmill happens when clinicians spend hours finishing notes long after the last patient has left. In behavioral health, this usually means typing SOAP, DAP, or BIRP notes into rigid templates that were never designed for therapy.
Why it happens:
- Most generic EHRs are built for physical health, not behavioral health.
- They lack flexible, narrative-friendly templates.
- Clinicians end up copy-pasting, building their own forms, or jotting notes outside the EHR and re-entering them later.
The impact:
- Burnout: clinicians spending 3+ hours daily on documentation.
- Lost productivity: fewer sessions per day.
- Errors: gaps or inconsistencies that can affect compliance and billing.
Example:
Picture this—your team is done seeing patients by 5 p.m., but at 8 p.m. they’re still at their laptops finishing notes. That’s the treadmill. No matter how fast they type, they can’t keep up. And we’re almost forgetting the risk of losing the minute details they have to recollect that could make a significant difference in therapy!
What to look for in a solution:
- Built-in templates for behavioral health note styles (SOAP, DAP, BIRP).
- Voice-to-text dictation for faster charting.
- Smart autofill to cut down repetitive typing.
A purpose-built behavioral health EHR breaks the treadmill by automating the grunt work so clinicians get their evenings back and can focus on patients, not paperwork.
Red flag 2: interoperability walls & fragmented care
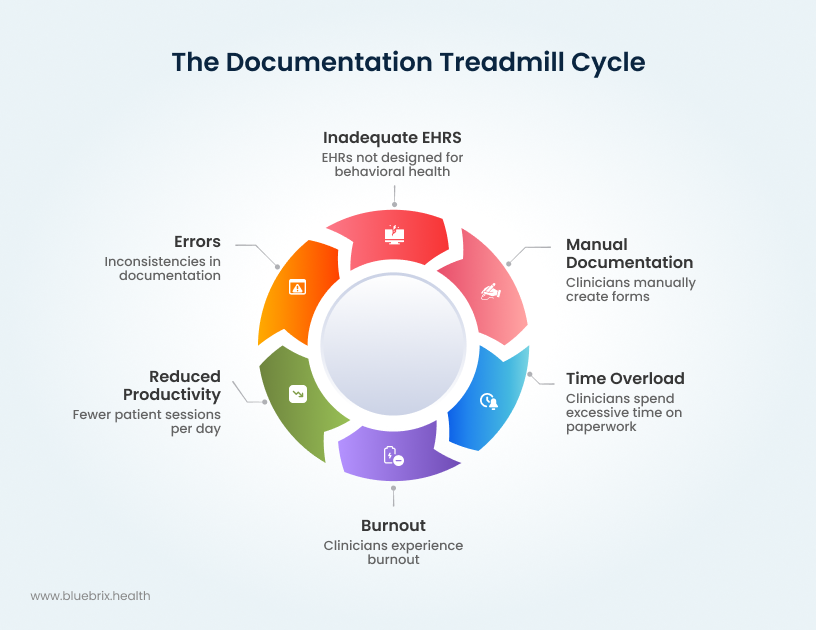
Interoperability walls are what happen when your EHR doesn’t “talk” to other systems. In behavioral health, that means you’re stuck faxing, scanning, or emailing records in 2025, while other parts of healthcare are moving toward real-time, secure data exchange.
Why it happens:
- Most legacy behavioral health EHRs don’t support modern standards like FHIR.
- Sensitive data like substance use treatment records are protected under 42 CFR Part 2, which adds complexity.
- Without built-in consent management, most practices default to over-blocking data, keeping information siloed.
The impact:
- Patient safety risks: missed medication updates, duplicate labs, incomplete histories.
- Poor care coordination: primary care, specialists, and behavioral health providers can’t stay aligned.
- Compliance headaches: either too much data sharing (privacy risk) or too little (care gaps).
Example:
A patient leaves the hospital with a new medication, but their behavioral health provider never sees the discharge summary. Weeks later, there’s a drug interaction that could have been avoided if the EHRs had been connected.
What to look for in a solution:
- Secure, FHIR-based interoperability that allows real-time exchange.
- Consent management tools that honor 42 CFR Part 2 and HIPAA.
- Configurations that let you share “just enough” data to protect patients and still keep care continuous.
With platforms like blueBriX, behavioral health teams can finally achieve true interoperability, not just message passing or data transfers, but seamless, secure coordination across the entire care network. The system enables real-time, FHIR-based data exchange with built-in consent management that respects both HIPAA and 42 CFR Part 2, ensuring clinicians always have the right information at the right time—without risking patient privacy or compliance.
Red flag 3: revenue cycle management (RCM) black holes
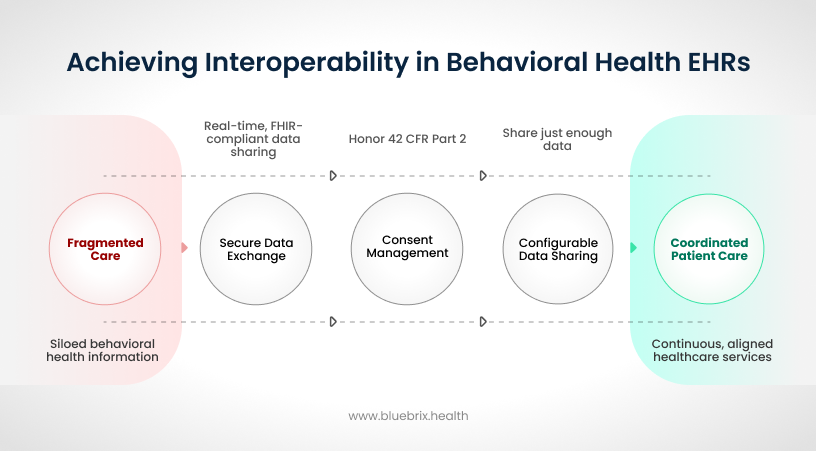
RCM black holes happen when your EHR can’t handle the complexity of behavioral health billing. Claims disappear into delays, denials pile up, and revenue gets stuck in limbo—all because the system wasn’t built for therapy, psychiatry, or substance use billing rules.
Why it happens:
- Behavioral health billing is more complex than physical medicine.
- Multiple services (therapy, med management, group sessions) may be billed in a single visit.
- Medicaid rules vary by state, and payer-specific requirements are detailed.
- Generic EHRs don’t support these nuances, leading to coding errors and underbilling.
The impact:
- High denial rates: claims bounce back due to missing modifiers or wrong codes.
- Cash flow strain: extended accounts receivable (AR) cycles slow down payments.
- Revenue leakage: missed opportunities to bill for services you actually delivered.
- Staff overload: billing teams spend hours fixing errors that software should catch.
Example:
Your billing team submits a claim for a visit that included both therapy and medication management. A generic EHR doesn’t bundle it correctly, the payer rejects it, and your team spends weeks fixing and resubmitting. Multiply that across hundreds of claims, and you’re looking at thousands in lost revenue and wasted staff hours.
What to look for in the right solution:
- Automated claim scrubbing that flags errors before submission.
- Behavioral health–specific CPT/ICD and DSM-V code templates.
- Built-in logic for Medicaid/Medicare variations.
- Real-time denial tracking and financial reporting.
A purpose-built behavioral health EHR like blueBriX plugs these black holes with automation. Claims are validated up front, denials drop, and you capture every dollar you’ve earned. That means steadier cash flow, less billing chaos, and more resources freed up for patient care.
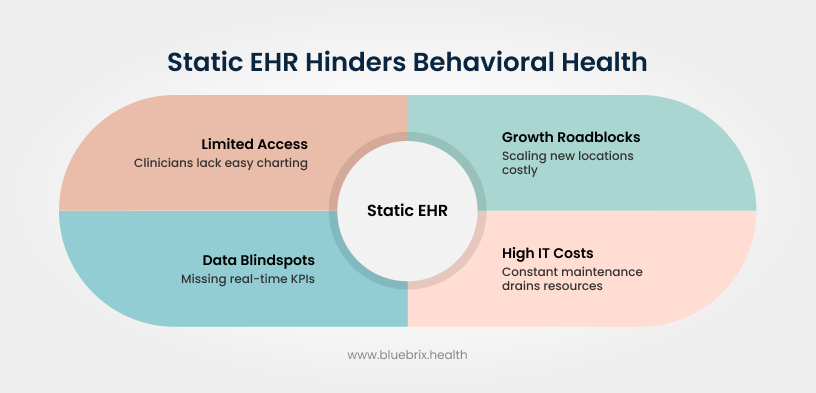
Red flag 4: static systems and missing future
A static EHR system is one that can’t adapt to modern behavioral health needs. These are often legacy or on-premise platforms that feel outdated, require costly upgrades, and make scaling your practice unnecessarily difficult.
Why it happens:
- On-premise systems weren’t designed for cloud use or multi-location practices.
- They lack mobile access, integrated telehealth, and digital patient engagement tools.
- Analytics are limited, leaving leadership blind to key trends.
- Upgrades often require expensive “rip-and-replace” projects.
The impact:
- Limited accessibility: clinicians can’t easily chart from multiple sites or during telehealth.
- Growth roadblocks: scaling to new locations is costly and disruptive.
- Data blind spots: missing real-time KPIs and outcome tracking for value-based care.
- High IT costs: constant maintenance and big-bang upgrades drain resources.
Example:
A clinic expands to two new sites, but their on-prem EHR can’t handle multi-location access. The only option? Buy separate licenses, build clunky workarounds, or rip everything out and migrate to a new system that could end up losing time, money, and morale in the process.
What to look for in a solution:
- Cloud-native design for easy, secure access anywhere.
- Mobile-friendly features for clinicians on the go.
- Built-in telehealth, digital tools, and patient engagement options.
- Real-time analytics dashboards to track outcomes, compliance, and financials.
- Scalable architecture that grows with your practice.
With blueBriX, practices can avoid the “static trap.” Its cloud-native, mobile-first design and predictive analytics make it flexible, scalable, and future-ready so you can grow without costly overhauls.
Ignoring the red flags: what risks do behavioral health practices face?
When behavioral health leaders ignore these red flags, the problems don’t stay small, they snowball.
- Clinician burnout: documentation overload drives staff out of the field.
- Patient safety issues: incomplete records and care silos put patients at risk.
- Revenue loss: denials, delays, and missed billing opportunities drain cash flow.
- Compliance gaps: outdated systems leave practices exposed under HIPAA and 42 CFR Part 2.
- Scalability barriers: legacy systems can’t keep up with multi-location or telehealth growth.
End of the day this means, every month with a misfit EHR adds more cost, more risk, and more frustration.