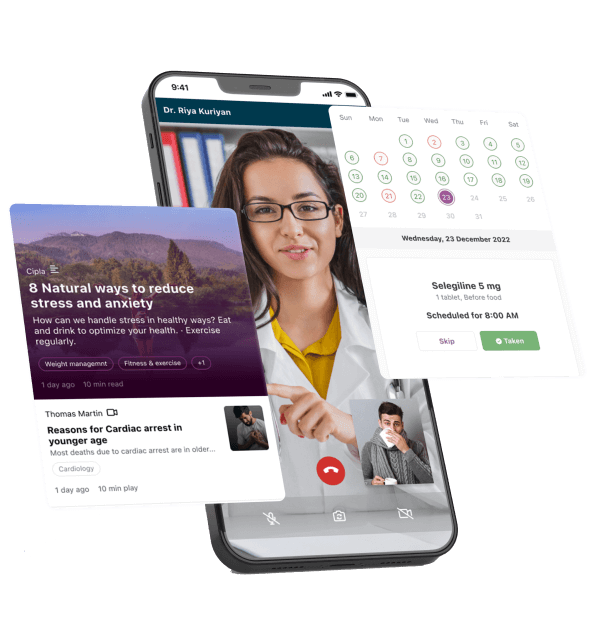
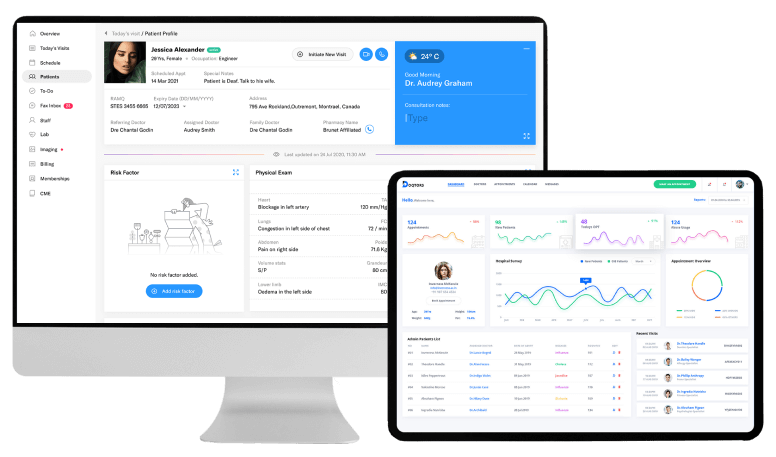
Patient engagement solutions
With blueBriX, launch meaningful patient engagement solutions that cater to specific needs.
Adherence
At blueBriX, we acknowledge the challenges associated with adhering to complex treatment protocols. That’s why we’ve developed a versatile and personalized adherence module that can adapt to diverse treatment regimes, fostering optimal and consistent engagement in their treatment.
Education
Recognizing diverse needs in patient education throughout their journey, our personalized educational module delivers the appropriate material at crucial times. Patients can fine-tune their contextual interests as they advance through their treatment path.
Remote patient monitoring (RPM)
The demand for home-based patient care is growing. The blueBriX RPM module offers vital features, such as questionnaire forms for assessing patient quality of life and symptoms. It also seamlessly connects with devices to collect patient vitals, symptoms, and adherence data.