Most Care Coordination platforms are just expensive digital silos. For CIOs facing 2030 value-based care deadlines, choosing the wrong one isn’t just an IT problem—it’s a revenue risk.
You’re not evaluating standalone software. You’re architecting how your EHR, population health tools, communication systems, community resources, and care teams work together as one unified operation. The question isn’t “which vendor should we buy?” rather “how do we connect the pieces we already have and fill the gaps that are breaking coordination?”
Value-based care has made this critical. Readmission penalties, quality bonuses, and risk-adjusted payments all depend on seamless coordination, yet most organizations still operate with siloed systems where information stays trapped and patients fall through the cracks.
Modern care coordination platforms promise to be the connective tissue, but the CIO’s challenge is determining which ones actually deliver. How do you evaluate platforms that must integrate with your existing infrastructure? How do you ensure orchestration works in practice, not just in demos?
This guide cuts through the vendor noise to focus on what matters: choosing platforms that integrate, coordinate, and deliver measurable value without adding another silo to your ecosystem.
Why this decision matters now
The business case has changed
The shift to value-based care has accelerated as 2030 is nearing and with it, the urgency for healthcare organizations to get care coordination right. Because care coordination is one of the central pillars of successful value-based care and achieving the associated incentives. Organizations that haven’t built the infrastructure for coordinated, accountable care will find themselves at a severe competitive disadvantage.
Here’s what’s changed: care coordination documented on paper won’t cut it anymore. Under value-based contracts, payers demand proof that coordination actually prevented readmissions, closed care gaps, and improved patient outcomes. It’s no longer enough to show you made phone calls or sent referrals. Instead, you must demonstrate a measurable impact across the entire care continuum.
The financial stakes are immediate and substantial:
- 30-day hospital readmissions trigger penalties costing organizations millions annually.
- Medicare Advantage Stars ratings—heavily dependent on care coordination quality—directly impact per-member-per-month payments.
- Automated Patient Care Management (APCM) billing offers monthly per-patient reimbursement for remote care coordination, but organizations without compliant platforms leave this revenue uncaptured.
- ACO and bundled payment models tie reimbursement to total cost of care, where coordination failures (duplicate tests, preventable ED visits, missed follow-ups) erode margins.
- HEDIS measures and quality bonuses reward organizations that demonstrate coordinated, proactive care across populations.
The penalties are real. The bonuses are substantial. And both hinge on your ability to coordinate effectively—and prove it.
But who gets caught in the middle trying to meet both ends? Providers. They’re the ones manually coordinating care—toggling between systems, hunting for information across disconnected platforms, and tracking referrals one by one. When teams spend more time fighting technology than caring for patients, burnout isn’t a risk—it’s inevitable.
On the other hand, we have patients whose expectations have also evolved. Patients expect seamless experiences—appointment reminders via text, accessible care plans, and transparent communication. When systems can’t deliver, patients disengage and disengaged patients don’t adhere to care plans or drive the outcomes your contracts require.
The market reality
If the business case is clear, the vendor landscape isn’t.
The market is crowded. EHR add-ons that don’t integrate fully, point solutions that create new silos, and population health tools that lack workflow depth. Each vendor claims to solve care coordination, but piecemeal approaches leave gaps. Effective coordination requires a unified platform that integrates seamlessly across your ecosystem.
Success depends entirely on fit: Does it integrate with your EHR? Match how your teams actually work? Address your specific coordination gaps?
But here’s what CIOs consistently underestimate: integration complexity. Vendors promise “seamless EHR integration” and “out-of-the-box interoperability.” Reality? Projects take 6-12 months longer than projected. Data doesn’t flow smoothly. Workflows require extensive customization. Interface fees pile up.
Integration isn’t one-time—it’s ongoing. HL7 feeds break. APIs change. EHR upgrades disrupt connectivity. The hidden cost: making the platform work can cost as much as the license itself.
The question isn’t just “which platform?” It’s “which platform can we actually implement, integrate, and sustain before 2030?”
The biggest mistakes CIOs make (and how to avoid them)
Even experienced CIOs fall into predictable traps when evaluating care coordination platforms. Vendors highlight their strongest capabilities while glossing over limitations. Demos show perfect scenarios, not messy real-world workflows.
Here are the five most common mistakes—and how to avoid them:

Mistake #1: Letting features drive the decision
The trap: Choosing the platform with the longest feature list.
The reality: Most organizations use only 30-40% of available features. Meanwhile, the 2-3 workflows your teams use daily might not work well at all.
The fix: Before evaluating vendors, identify 2-3 critical workflows that must work perfectly. For example: “We need seamless hospital-to-home transition tracking with automatic task assignment.” Evaluate vendors primarily on how well they execute your priority workflows, not how many generic features they offer.
Mistake #2: Underestimating integration complexity
The trap: Believing “certified EHR integration” means seamless data flow from day one.
The reality: Integration projects routinely take 6-12 months longer than projected. HL7 feeds require custom mapping. Real-time sync isn’t actually real-time. Even after go-live, integration maintenance is ongoing—EHR upgrades break connections, and edge cases emerge constantly.
The fix: Demand a technical deep-dive demo using your actual EHR instance, your data, and your workflows—not the vendor’s staged environment. Speak with reference customers using your same EHR about integration challenges. Budget 50% more time and money for integration than the vendor estimates.
Mistake #3: Ignoring the end-user experience
The trap: CIOs and executives evaluate platforms in conference rooms while care coordinators who will actually use the system aren’t involved until after the decision is made.
The reality: If care managers find the interface confusing or workflows cumbersome, they’ll abandon it. Studies show 30-50% of healthcare IT implementations fail due to poor user adoption.
The fix: Include frontline care coordinators in vendor demos from day one. Have them test the platform with real patient scenarios they handle daily. Conduct pilot programs before organization-wide rollout. Make user satisfaction a primary evaluation criterion.
Mistake #4: Skipping the pilot program
The trap: Going straight to enterprise-wide deployment because you’re confident in your vendor selection and want faster ROI.
The reality: Full-fledged deployment without piloting means discovering workflow gaps, integration issues, and user adoption challenges across your entire organization simultaneously—creating chaos and eroding confidence in the platform before you can optimize it.
The fix: Start with a focused pilot:
- Select 1-2 care teams or service lines (e.g., cardiology transitions of care, high-risk diabetes management)
- Run for 60-90 days with clear success criteria
- Gather user feedback continuously and iterate
- Document what works, what needs adjustment, and what requires vendor fixes
Mistake #5: Vendor lock-in without exit strategy
The trap: Negotiating contracts focused on price and features without thinking about exit terms.
The reality: If the platform disappoints or your needs change, you’re stuck paying for a system you don’t want, unable to transition because your data is trapped in proprietary formats.
The fix: Negotiate upfront:
- Full data export rights in standard formats (CSV, JSON, FHIR) with no fees
- Reasonable termination clauses with performance-based exit provisions
- Clear pricing escalation terms as you scale
- Vendor commitment to support transition if you leave
The common thread? Each mistake happens when CIOs prioritize the sales process over operational reality. Ground every decision in operational truth. Test with real users. Demand proof from similar organizations. Define success numerically. Plan for things going wrong.
Start with strategy, not software
Most organizations jump straight to vendor demos without doing the critical strategic work first. That’s how you end up comparing features instead of evaluating fit and selecting platforms that solve the wrong problems.
Before you talk to vendors, answer these questions:
What problem are we actually solving?
Care coordination means different things to different organizations. Be specific about your highest-priority gap:
- Reducing readmissions for specific populations?
- Closing care gaps for quality measures?
- Managing transitions from hospital to home?
- Addressing social determinants of health?
Who needs to change?
Platforms don’t coordinate care—people do. Identify whose workflows must improve for coordination to succeed:
- Care managers overwhelmed with manual work?
- Physicians frustrated by fragmented patient information?
- Patients lost in care transitions?
What does success look like in 12 months?
Vague goals lead to vague results. Define concrete metrics before evaluating vendors:
- Specific metrics: readmission reduction %, care gap closure rates, coordinator productivity
- Financial targets: cost savings, quality bonus capture, contract performance
- Adoption metrics: user satisfaction, workflow time savings
What’s the tolerance for disruption?
Be honest about your organization’s capacity for change. Implementation complexity varies dramatically:
- Implementation bandwidth: Do you have dedicated IT resources available for integration work, or is your team already stretched thin managing day-to-day operations?
- Change management maturity: How does your team actually respond when workflows change?
- Budget for true total cost of ownership: Beyond the licensing or subscription fee, can you afford implementation costs, ongoing maintenance, staff training time, potential workflow disruptions during transition, and the hidden costs of customization or integration work?
Without clear answers to these questions, vendor selection becomes a guessing game. The right platform for another organization might be completely wrong for yours and you won’t know the difference until you’ve already signed the contract.
The nine non-negotiable capabilities in your care coordination platform
When evaluating care coordination platforms, focus on these nine non-negotiables. Without them, coordination fails regardless of how impressive the demo looks.

Real interoperability, not just integration
Your system must enable bi-directional, real-time data flow without manual intervention. If coordinators are still copying and pasting between systems, the platform isn’t doing its job. True interoperability should eliminate duplicate data entry entirely, freeing your team to focus on patient care instead of administrative workarounds.
A complete patient view that actually helps
Look for a solution that consolidates all relevant clinical and social information into one actionable dashboard. More data doesn’t equal better coordination—the system must intelligently surface what’s most important instead of burying critical alerts in dozens of updates. The view should help teams make faster decisions, not overwhelm them with information.
Workflow that matches how care teams actually work
The right solution adapts to your processes, not the other way around. Feature-rich platforms that disrupt established workflows get abandoned by frustrated staff. It should support the way your care coordinators actually spend their day—from intake through discharge—without requiring workarounds or extra steps.
Dynamic, patient-centered care plans
Care plans built around each patient’s unique conditions, goals, and circumstances—not generic templates. Your platform should allow you to create condition-specific pathways that automatically assign tasks to the right team members, track progress across disciplines, and adapt as the patient’s needs evolve.
Proactive intelligence, not just reactive alerts
The system must identify patients who need intervention before crises happen. Value-based success requires prevention, not damage control. It should leverage predictive analytics to flag high-risk patients before they show up in the emergency department—giving your team time to intervene proactively.
Tools that keep patients engaged in their care
The right platform extends beyond the clinic visit to keep patients actively participating in their care. It should give patients access to their care plans, deliver automated reminders, and enable direct communication with their care team. Without these tools, coordination stops at the provider level and misses the most important participant—the patient.
Security, compliance, and data governance
Any solution must include built-in safeguards that protect patient data and ensure regulatory compliance. HIPAA, 42 CFR Part 2, role-based access, encryption, and comprehensive audit trails should be standard—not optional add-ons. The system must handle consent management and multi-organization data sharing securely and transparently.
Scalability and future-proofing
Look for a solution that grows with your organization and adapts to evolving care models without requiring expensive rebuilds. Whether you’re managing 10,000 patients today or 50,000 across multiple service lines tomorrow, the system should scale seamlessly. It must handle multiple care models simultaneously without performance degradation or exponential cost increases.
Measurable impact from day one
Built-in analytics that prove ROI and support continuous improvement. You need to demonstrate value to executives and optimize performance over time. Request case studies showing how the vendor has measured impact for organizations similar to yours.
Beyond features: evaluating the partnership
Selecting a care coordination platform isn’t just a technology decision—it’s choosing a long-term partner embedded in your daily operations. The most feature-rich platform fails if the vendor can’t implement it effectively, support your teams reliably, or adapt as your needs evolve. Let’s explore “partnership-fit” checkers!
Implementation Reality Check
Every vendor promises rapid, seamless implementation. The reality is more complex. Most care coordination platforms take 6-12 months to deliver real operational value, regardless of vendor timelines. Integration takes longer than projected. Data migration uncovers quality issues. Workflows require more customization than expected. Care teams need time to adapt.
This isn’t a failure—it’s the nature of integrating complex systems into live clinical operations. What separates successful implementations from disasters is honest planning and vendor transparency upfront.
Questions to ask vendors:
- What’s the typical implementation timeline for organizations our size and complexity?
- What percentage of your implementations finish on time and on budget?
- How much of our IT team’s time will this realistically require—not best-case, but typical?
- What are the most common implementation challenges, and how do you address them?
Support When Things Go Wrong
The uncomfortable truth is that every platform has issues. Systems go down. Integrations break. Data doesn’t sync as expected. Users get confused. What separates good vendors from bad ones isn’t perfection—it’s how they respond when things go wrong.
When your care coordinators can’t access patient data, or a critical integration fails during a busy clinic day, you need immediate, effective support. Not a ticket queue. Not a “we’ll escalate this” email. Real help, fast.
Questions to assess support quality:
- What’s your average response time for critical issues that block care coordination workflows?
- Do we get a dedicated support contact who knows our environment, or do we enter a general ticket queue?
- What are your support hours—24/7, business hours only, or something in between?
- Can we see your system uptime history for the past year? What was your longest outage?
- What’s your escalation process when our care teams are completely blocked?
- How do you handle issues that require coordination between your team, our EHR vendor, and our IT staff?
What good support looks like:
- Defined response time commitments with accountability (e.g., critical issues acknowledged within 1 hour, resolution path within 4 hours)
- Dedicated account support, not rotating help desk staff
- Proactive monitoring and notification of issues before users report them
- Clear escalation paths when standard support isn’t resolving problems
- Post-incident reviews and prevention planning
The hidden costs nobody talks about
Vendor proposals focus on one number: the annual license fee. But that rarely reflects what you’ll actually spend. The true cost of ownership is typically 2-3 times the quoted license fee when you account for integration, training, customization, and ongoing support.
Organizations that budget only for licensing inevitably face budget overruns, delayed implementations, or compromised functionality because they can’t afford the “extras” needed to make the platform actually work.
It’s not just the license fee
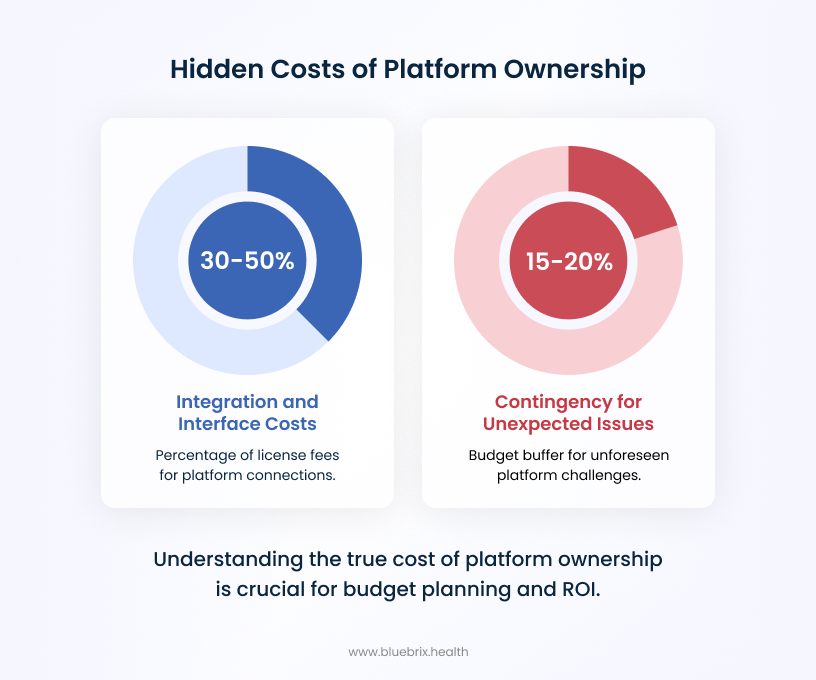
Integration and interface costs (often 30-50% of license fees)
Your platform must connect to your EHR, claims data, HIEs, referral networks, and community resources. Each connection costs money:
- HL7 interface development and testing
- API connection fees (often per call or data volume)
- Custom field mapping for your EHR configuration
- Ongoing interface maintenance and troubleshooting
Integration costs routinely exceed initial vendor estimates, and maintenance fees continue indefinitely.
Data migration and cleanup
Legacy systems contain duplicate records, inconsistent conventions, and incomplete fields. Migration forces you to address:
- Data assessment and quality auditing
- Deduplication and standardization
- Historical data conversion and validation
- Manual cleanup of critical records
What vendors quote as a quick migration often becomes a months-long cleanup project.
Training and change management (the most underestimated cost)
Training isn’t one-time—it’s ongoing as staff turns over and workflows evolve:
- Initial training for all user roles
- Super user and champion programs
- Custom training materials
- Ongoing education for new hires
- Change management to drive adoption
Vendors include “basic training” (a few webinars). Real adoption requires role-specific training delivered over months.
Ongoing customization and optimization
Out-of-the-box platforms rarely fit perfectly:
- Workflow configuration refinement
- Custom report development
- Dashboard and alert customization
- Integration of additional data sources post go-live
High-performing organizations continuously refine platforms—requiring ongoing investment.
Internal it resources
Your IT team will be deeply involved:
- Dedicated staff during implementation
- Ongoing support and maintenance
- Vendor upgrade coordination
- Security and compliance monitoring
Total cost of ownership over 3-5 years
Smart CIOs evaluate platforms based on total cost of ownership (TCO), not just year-one licensing. Hidden costs in year one often more than double the license fee. Ongoing costs typically run 50% above licensing in subsequent years.
Budget realistically: the smarter approach
- Assume total costs will be 2-3x the annual license fee in year one
- Budget 1.5x the license fee annually for ongoing operation
- Require itemized TCO projections, not just licensing quotes
- Build 15-20% contingency for unexpected issues
Bottom line: The cheapest platform isn’t the one with the lowest license fee—it’s the one that delivers value relative to true total cost. Be honest about costs upfront. Your CFO would rather see realistic projections that deliver ROI than low initial quotes that balloon into budget disasters.
Building your evaluation framework
A structured approach ensures you choose the platform that fits your organization, not just the one with the best demo.
Assemble the right team
Don’t make this an IT-only decision. The best technical platform is worthless if clinicians won’t use it.
Your evaluation team must include:
- Clinical leaders (physicians, care managers, social workers)
- Revenue cycle/coding representatives
- Quality and population health teams
- IT architecture and security
- Operations and workflow experts
Each perspective is critical. Clinical leaders ensure workflow fit. Revenue cycle validates coding and billing impact. Quality teams confirm reporting capabilities. IT assesses integration feasibility. Operations identifies implementation risks.
Create a weighted scoring system
Evaluate vendors objectively by weighting criteria based on your organization’s priorities:
Sample priorities (adjust for your organization):
- Clinical workflow fit: 30%
- Interoperability and data quality: 25%
- ROI potential and proven outcomes: 20%
- Partnership and support: 15%
- Implementation feasibility: 10%
If integration complexity is your primary concern, weight it higher. If user adoption has killed past implementations, prioritize workflow fit. There’s no universal formula—weight what matters most to your organization’s success.

