
An EHR is meant to help and ease the lives of doctors. According to a recent study by the Annals of Family Medicine, they’re having the opposite effect. During an 11.4 hour workday, primary care physicians end up spending 5.9 hours on EHR related tasks. As a result the American Medical Association (And Others) is unhappy with the EHR Providers.
According to the American Medical Association (AMA), “data entry tasks associated with EHR systems are significantly cutting into available time for physicians to engage with patients.” The organization blames poorly designed and implemented EHRs for this, claiming that it is leading to neglected patients and doctor burnout rates (which are growing to more than 50 percent).
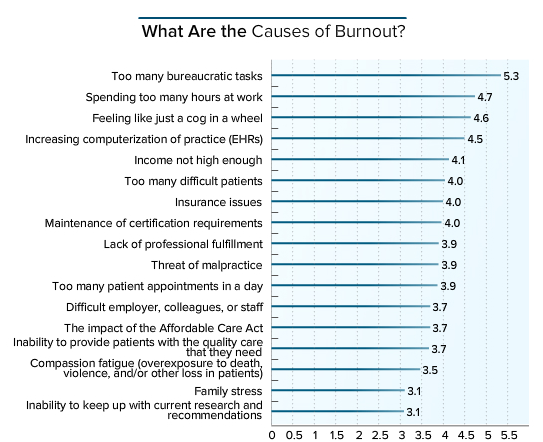
A MedScape Lifestyle Report, however, offers us a little more context: burnout is mostly linked to ‘too many bureaucratic tasks,’ followed (with a wide margin) by ‘spending too many hours at work,’ ‘feeling like just a cog in a wheel,’ and ‘increasing computerization of practice (EHRs).’
At this point, the industry has been talking about doctor burnout and EHR design for years. However, AMA’s conclusion that poor design and implementation are leading to issues might be a stretch. For the sake of *this* particular blog, we will explore it.
AMA is strongly encouraging EHR providers to redesign with a set of 8 priorities in mind. These being:
- Enhance physicians’ ability to provide high-quality patient care
- Support team-based care
- Promote care coordination
- Offer product modularity and reconfigurability
- Reduce cognitive workload
- Promote data liquidity
- Facilitate digital and mobile patient engagement
- Expedite user input into product design and post-implementation feedback
A number of aspects on AMA’s list can be consolidated. Care coordination, and data liquidity speak to the basic benefits of interoperability in healthcare. Ideally, EHR providers would address the lack of interoperability and the time it takes to transfer patient data to different systems (we’ve written about this before too). Systems should be able to exchange data between any EHR system, health exchange or clearing house.
Quality patient care, and patient engagement can be addressed through custom workflows, specifically designed and implemented to prompt the staff of certain tasks, focus the information provided to a doctor or remind staff members of certain forms they need a patient to complete.
Product modularity is a little more complex – it relies entirely on how the system is initially visualized and architected. Very few (if any) well known EHR systems can fulfill this in the current market – the systems are too rigid and archaic. It would be too expensive to change to a more modular structure at this point. Unfortunately, client fatigue and user difficulty is not enough of a financial motivator to prompt any significant change.
A quality EHR fulfills the AMA’s eight priorities easily by keeping the end user in mind. A good system is built with cognitive design and is malleable – shaping to fit the client’s needs and, ideally, reducing burnout. The system has good usability because it incorporates the user from the beginning.
The AMA can’t mandate these changes in the industry. The purpose of our entire industry is to make the lives of providers and the public better, and we can only do that if we work to create a system that works for them. We should align to a mission similar to the AMA and “promote the art and science of medicine and the betterment of public health”.