Why the 2025 ABA CPT code changes demand your immediate attention
The 2025 CPT code updates are not a minor adjustment. They represent a significant operational and financial challenge for Applied Behavior Analysis (ABA) providers and hospital behavioral programs. All year, payers have tightened their policies, CMS finalized its telehealth rules, and the CPT Editorial Panel moved forward with several adaptive-behavior revisions. With the AMA’s 2025 release bringing 420 total updates, ABA services are directly in the crosshairs.
If your templates, prior-auth checklists, or edits still reflect pre-2025 habits, you’re setting yourself up for avoidable denials, severe audit risk, and disruptive cash-flow swings. Treat Q4 2025 as your cleanup window. Use it to validate your notes, telehealth mappings, and code usage against this year’s rules, not last year’s shortcuts.
Why immediate attention is critical: the scale of change
The core reason the 2025 updates demand immediate action is the complexity of the changes across documentation, billing, and defense of your work. The AMA’s 2025 CPT release brought 420 total updates: 270 new codes, 112 deletions, and 38 revisions. That’s a massive shift, and ABA services were right in the middle of it. When clinicians ask why the EHR and billing edits had to change, that’s your context.
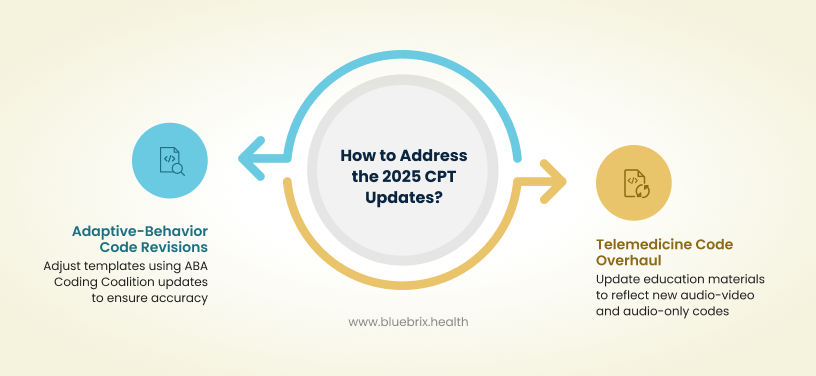
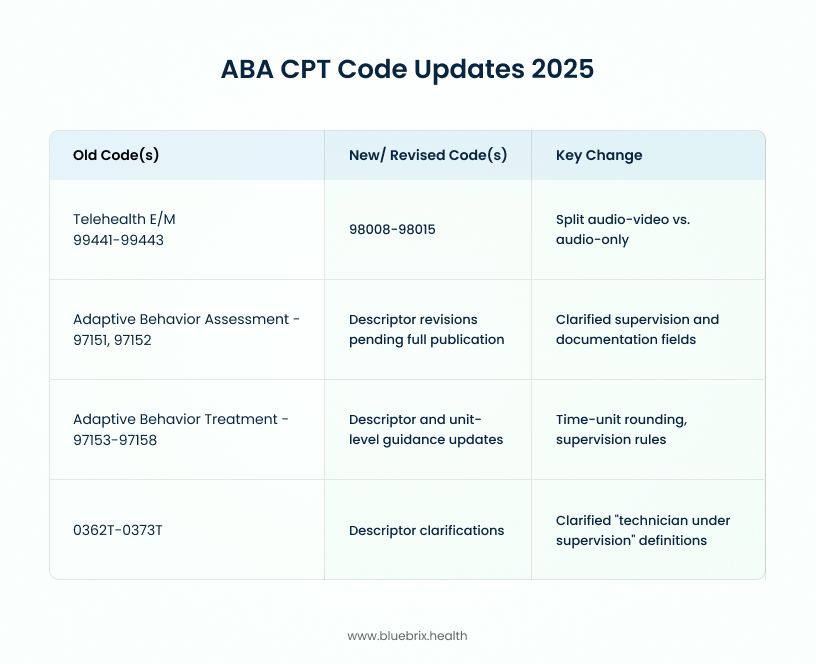
Two high-impact changes matter most for ABA teams:
- Adaptive-Behavior Code Revisions: The ABA Coding Coalition confirmed more adaptive-behavior code revisions approved at the September 2025 CPT Editorial Panel meeting. They’ve been the clearest public tracker of what’s coming, so use their updates alongside your 2025 CPT book to adjust templates down to the descriptor level.
- Telemedicine Code Overhaul: The new 98000-series telemedicine E/M codes officially replaced the old telephone codes 99441–99443. These new codes separate audio-video from audio-only encounters. Even if your payer handles them differently, your education materials and crosswalks should reflect the CPT 2025 structure.
Navigating the Medicare caveat
While CPT 2025 added the 98008–98015 audio-only codes, Medicare didn’t adopt them. For traditional Medicare, stick with the standard E/M codes and use POS 02 (telehealth) or POS 10 (home) plus the appropriate 95 or 93 modifier. Commercial payers can choose to recognize the new codes independently.
For Medicare billing in general, remember CMS runs its own Telehealth List and payment rules. The Q3014 originating-site facility fee is $31.01 for CY 2025. Commercial payers, however, can choose to recognize the new codes independently. CMS published its updated list and fee schedule early in the year. Make sure your POS and modifier logic matches those publications before you add any payer-specific rules.
How the updates affect your revenue cycle — from front-end to back-end
The 2025 CPT changes impact every stage of your Revenue Cycle Management process:
- Front end: Prior auth is usually where friction starts. In 2025, payers got stricter about unit counts, supervision requirements, and documentation language for adaptive-behavior services. If intake staff are still using outdated code lists or skipping unit detail on re-auths, approvals stall and care plans slip.
- Mid-cycle: The single best predictor of clean claims this year has been documentation accuracy. Common misses: time rounding on 15-minute codes, missing supervision level, and telehealth mappings that don’t match current rules. Make sure your templates and dropdowns are built around AMA’s behavioral health and telemedicine guidance and your payer bulletins so clinicians aren’t left guessing.
- Back end: Your denial trends tell the story. Most programs saw a denial spike early in 2025 and a recovery once edits were updated and staff retrained. If your first-pass rate still hasn’t bounced back, look at claims with time-unit or POS/modifier mismatches against CMS’s current telehealth list, then retest. The Q3014 fee update still catches systems that never refreshed that field.
Common mistakes and the blueBriX readiness checklist
Providers often make critical mistakes when CPT codes change, leading to major revenue loss:
Mistake 1: writing to old descriptors
If your templates don’t prompt for supervision level, setting, or start-stop time, the claim looks under-documented and that’s an automatic denial.
Mistake 2: freezing clearinghouse rules
Your edits must reflect CPT 2025 and CMS’s 2025 Telehealth List, including the deletion of 99441–99443 and addition of the 98000 series. Load the current year first, then apply payer-specific tweaks.
Mistake 3: assuming all payers mirror Medicare
CMS publishes recognition and status indicators on its list. Some commercial plans follow them; others don’t. Anchor your logic to CMS, then map the differences so your clearinghouse routes claims correctly.
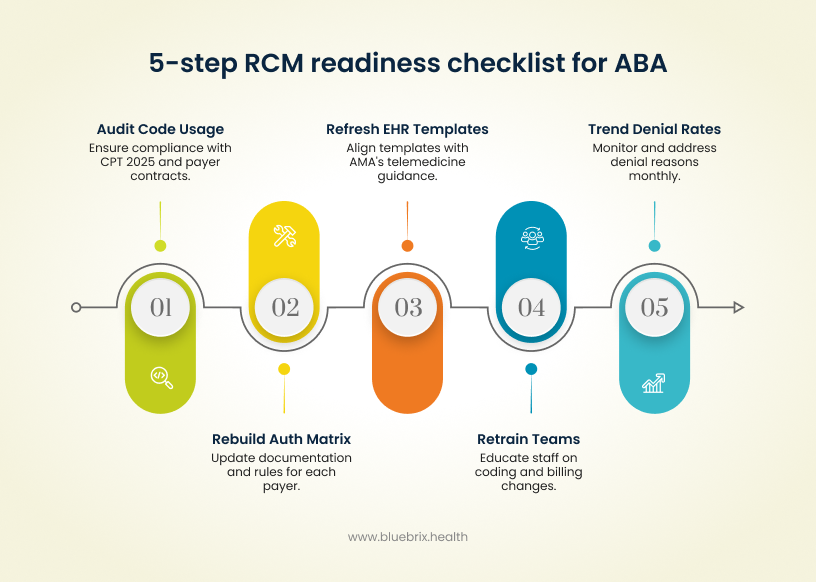
A 5-step RCM readiness checklist for ABA providers and hospital programs
- Audit your code usage. Make sure your top ABA codes and any telemedicine E/M activity align with CPT 2025 and your payer contracts.
- Rebuild the prior-auth matrix. Show staff the current documentation, unit, and evidence rules for each payer.
- Refresh EHR templates. Base them on AMA’s 2025 telemedicine and behavioral health guidance so time, supervision, and setting fields are consistent.
- Retrain coding and billing teams. Use real examples, covering both audio-video and audio-only cases, so everyone understands what changed.
- Trend your first-pass rates monthly. By Q4, denial reasons should cluster into a few fixable categories once your rules are fully current.
How a network that recovered revenue after the 2025 transition
A multi-site ABA network started 2025 with old note templates and outdated telehealth edits. Denials spiked for time-unit rounding and missing supervision details, and the old telephone E/M codes kept showing up even after January.
They fixed it fast: four weeks of work to rebuild templates, load CPT 2025 logic, and overhaul the prior-auth checklist. By the next quarter, collections stabilized and first-pass rates climbed higher than before.
The takeaway: align your system to current rules, then monitor for drift.
Why outsourcing RCM / coding support may be the safest move?
The 2025 ABA CPT updates are active now and will shape your reimbursement and audit posture through year-end. Audit your code usage, sync templates to CPT 2025 and AMA telemedicine guidance, and map your edits to CMS’s 2025 Telehealth List. If your internal team can’t keep pace with AMA updates, CMS telehealth maintenance, and payer bulletins, a specialized RCM partner can carry that load. External teams keep current-year edits up to date, refresh templates, and trend denials continuously.
It’s not just about cutting write-offs, it’s about protecting cash flow when CMS or a payer shifts the rules mid-year. Outsourcing can bridge the gap while you build in-house capacity, or serve as a long-term way to keep your rule set current without adding headcount. Track denials monthly and decide where a specialist like blueBriX can protect margins while you absorb the changes.
Why blueBriX is the ultimate compliance partner
If your internal team cannot keep pace with AMA updates, CMS telehealth maintenance, and dozens of payer bulletins, outsourcing to a specialized RCM partner is often the safest move.
Proven ROI through proactive alignment
A multi-site ABA network started 2025 with old note templates and outdated telehealth edits, resulting in denials spiking for time-unit rounding and missing supervision details. They recovered 18% lost revenue by dedicating four weeks to rebuild templates, load CPT 2025 logic, and overhaul the prior-auth checklist. This proves the ROI of proactive RCM support: align your system to current rules, then monitor for drift.
The role of automation and AI in compliance
Compliance in 2025 requires automation:
- Real-time Coding Validation: Scrubbers check time increments, supervision notes, POS, and modifiers against the 2025 CMS Telehealth List before a claim ever leaves your system.
- Automated Payer Rule Enforcement: Automated rule libraries pull in payer bulletins, making it realistic to keep up with mid-year policy changes.
- Predictive Denial Analytics: AI flags claims that look like past denials, reducing rework and touch time per claim.
blueBriX end-to-end coding & billing support
blueBriX keeps programs aligned with current-year rules by combining template rebuilds, code-set updates, payer-policy mapping, and monthly first-pass analytics. We load CPT 2025 telemedicine logic and the current CMS Telehealth List into your edits, and co-train clinical and billing staff so documentation and coding tell the same story. It’s about steady cash flow in a year when the rules have moved more than once.
Schedule your complimentary CPT transition advisory call.