For years, clinic leaders have watched care coordination happen in the background sometimes by design, more often by accident. A care coordinator spends an hour tracking down discharge paperwork. A medical assistant calls a specialist’s office for the third time to confirm whether Mrs. Chen’s referral was received. A nurse navigator reconciles medications after a patient’s hospitalization. Nobody’s tracking this work. Nobody’s billing for it. It’s just what clinics do.
That era ends January 1, 2026.
CMS’s final 2026 Medicare Physician Fee Schedule rule, finalized in late October 2025, explicitly recognizes care coordination as a billable, reimbursable service and the payment rates are substantial enough to reshape clinic economics. For the first time, clinics can capture dedicated revenue for the coordination work that has always been essential to patient care but never properly compensated. This isn’t a modest adjustment. For many clinics, it’s the difference between staying independent and consolidating under hospital ownership.
But here’s the catch: capturing this opportunity requires understanding what changed, why it matters, and most importantly what it takes to actually implement it. Let’s walk through the landscape.
Care coordination has been free for too long
Think about the journey your clinic coordinator takes on a typical Tuesday morning:
At 8:15 AM, a discharge notification arrives for Mr. Patterson, who spent two nights in the hospital for pneumonia exacerbation. Your coordinator downloads the discharge summary, adds it to his chart, and calls him to schedule a follow-up appointment. She also pulls his medication list from the hospital discharge paperwork and compares it to what you have on file. Three medications changed. She flags these for the provider to review and plans to call Mr. Patterson again in 72 hours to confirm he’s gotten prescriptions filled and is taking them correctly.
At 9:00 AM, a prior authorization request comes in for a specialist referral you sent for Ms. Rodriguez. Your coordinator calls the specialist’s office, then the payer, then back to the specialist. Finally, it’s approved. She schedules the appointment and sends confirmation to the patient.
At 10:30 AM, your population health team flags that 15 patients haven’t had their annual flu vaccine. Your coordinator starts making outreach calls.
By noon, she’s touched dozens of patients and completed hundreds of small tasks that, collectively, keep your clinic’s care coherent and timely.
And here’s what you’ve been reimbursed for all of this: nothing. Zero. Zip.
Your clinic bills the visit codes when patients come in. You bill chronic care management codes for some patients. But the glue that holds care together, the coordination that prevents 30-day readmissions, catches medication errors, ensures referrals are followed, and identifies patients with unmet social needs has been invisible on the billing ledger.
For decades, this worked because care coordination was implicit in primary care. Clinics absorbed the cost because it was part of the job. But as primary care margins have tightened, as populations have grown sicker and more complex, and as patient journeys have spanned multiple providers and settings, care coordination has become not just important it’s become essential to value-based contracting, quality metrics, and patient outcomes.
CMS recognized this distortion. The result: explicit, unbundled reimbursement for care coordination, starting in 2026.
Three changes that reshape primary care economics
The 2026 final rule introduces three critical shifts that fundamentally change the financial picture for clinics:
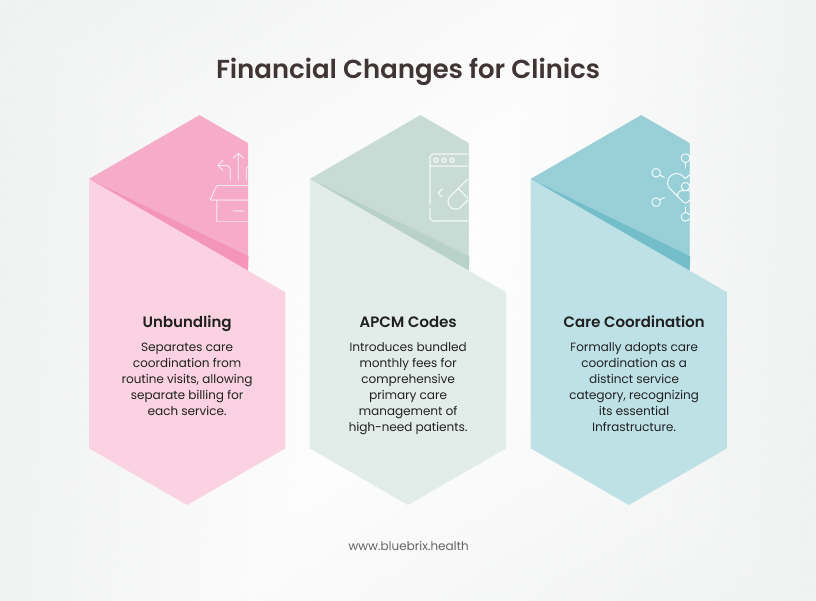
1. Unbundling separates care coordination from routine visits
For years, RHCs and FQHCs operated under a bundled payment model. A single visit generated a single bundled code (like G0511 for RHCs), which included a flat fee regardless of whether the clinic also provided chronic care management, remote patient monitoring, remote therapeutic monitoring, or behavioral health integration. It was all-in-one, and payments were capped.
Starting January 1, 2026, CMS is unbundling these services. This means RHCs and FQHCs that provide multiple care management services to the same patient can now bill separately for each service and at higher rates.
What this means in dollars: A mid-size FQHC that previously coded G0511 at roughly $54.67/month can now bill individual codes: Chronic Care Management (CCM) at $42.22, Remote Patient Monitoring (RPM) at $31.20, Remote Therapeutic Monitoring (RTM) at $16.87, and behavioral health add-ons at additional rates. For a complex patient receiving all four services, the monthly reimbursement jumps from $54.67 to $150+. For a clinic with 200 complex patients receiving multiple services, that’s easily an additional $200K $300K annually.
2. APCM codes signal CMS’s primary care strategy going forward
The Advanced primary care management (APCM) codes G0556, G0557, and G0558 were introduced in 2025 as a pilot. CMS is now expanding them and signaling they’re the centerpiece of its primary care payment strategy going forward.
These three codes represent a fundamentally different payment model: instead of paying for individual care management services, CMS pays a bundled monthly fee for comprehensive primary care management of high-need patients. The three codes are tiered by complexity:
- G0556 is for patients with 1 or fewer chronic conditions and reimburses at approximately $15 per month per patient. This tier is suitable for clinics managing less complex populations or as an entry point into APCM.
- G0557 is for patients with 2 or more chronic conditions and reimburses at approximately $50 per month per patient. This is the most commonly used tier and is designed for clinics managing moderately complex populations with multiple comorbidities.
- G0558 is for patients with 2 or more chronic conditions plus Qualified Medicare Beneficiary (QMB) status, indicating low-income beneficiaries, and reimburses at approximately $110 per month per patient. This tier recognizes the additional complexity of dual-eligible patients and provides substantially higher reimbursement.
But here’s what makes these codes different: they’re not just billing codes. They require clinics to deliver 13 specific service elements: 24/7 access, comprehensive care planning, team-based delivery, systematic risk stratification, care transitions protocols, quality reporting, and more.
What this means in opportunity: A clinic with 500 patients with 2+ chronic conditions (G0557 eligible) generates $300,000 annually just from APCM. Add another 100 dual-eligible patients at G0558, and you’re at $433,000. For a clinic with multiple providers, this scales quickly. A 10-provider clinic could realistically generate $1 million or more in new annual APCM revenue.
3. Explicit recognition of care coordination as a distinct service category
CMS is formally adopting care coordination as a designated service category for RHCs and FQHCs separate from clinical care management. Care coordination includes activities like managing referrals, coordinating with specialists and post-acute providers, supporting care transitions, and ensuring care plans are accessible across settings. These are non-face-to-face administrative services that are now billable. This distinction matters because care coordination was previously bundled or invisible. Now it’s recognized as essential infrastructure, with dedicated payment.
Advanced primary care management: the 13 elements every clinic needs to know
If your clinic decides to pursue APCM, here’s what CMS requires. These 13 elements aren’t optional; they’re mandated for billing and audit compliance. CMS will audit clinics billing APCM to verify all elements are actually being delivered, not just documented. Here’s the complete list:
Element 1: 24/7 patient access & continuity
Patients must have round-the-clock access to reach the clinic with urgent needs. This doesn’t mean a physician is on-call 24/7; it means there’s a documented after-hours protocol, perhaps through an on-call service or nurse line. Patients need real-time access to their medical records and the ability to schedule follow-ups with their care team. Documentation is critical: your clinic must be able to prove to auditors that patients know how to reach you at 2 AM on a Sunday.
Element 2: comprehensive, electronic care plans
Patients must have a written, patient-centered care plan that lives in your EHR. It should address diagnosis, treatment, management goals, and required follow-ups. The plan must be regularly updated, especially after hospitalizations. Critically, the patient and caregivers must have access to this plan—not as a locked PDF, but as something they can engage with. The care plan should be accessible to your full care team, specialists, and post-acute providers whenever possible.
Element 3: systematic risk stratification
Your clinic must identify high-risk patients using evidence-based tools (CMS has approved models, or your payer may provide them). Risk stratification should incorporate clinical data (chronic conditions, utilization history, medication complexity) and social determinants of health (housing status, food security, transportation, literacy, social isolation). This isn’t optional or intuitive; it requires systematic processes and often software support. You must be able to document your risk stratification methodology for audits.
Element 4: proactive care gap identification
Your team must actively monitor for missed preventive services, medication adjustments, test results, and screening. This means running population health reports regularly—not waiting for patients to notice gaps themselves. Your care coordinators should have dashboards showing which patients are due for flu shots, which have not filled new prescriptions, which have overdue labs or imaging. This must be systematic, not sporadic.
Element 5: care transitions protocol
Patients requiring hospitalization, emergency department visits, or SNF placement must receive documented follow-up within 7 days of discharge or transition. Your clinic must have a process to receive notifications (often through health information exchanges), assign tasks to care coordinators, and document the follow-up. This is one of the most audited elements, because the 7-day window is explicit and measurable.
Element 6: team-based care delivery
APCM isn’t just the physician. It requires a team: care coordinators, clinical staff, navigators, and the physician or qualified practitioner as the “primary focal point.” Clear role delineation is essential. Your care coordinator isn’t filing charts; she’s making proactive outreach calls, coordinating with specialists, and managing care transitions. Your clinical staff isn’t just processing visits; they’re monitoring lab results, flagging clinical concerns, and supporting patient self-management.
Element 7: self-management support & patient engagement
Your clinic must actively support patients in managing their conditions. This includes education about medications, lifestyle modifications, symptom monitoring, and when to seek care. Patients should understand their diagnoses, treatment goals, and their role in achieving those goals. This can be delivered through group visits, individual counseling, digital tools, or community programs—but it must be documented and systematized.
Element 8: coordination with community resources & social services
Clinics must identify and connect patients with community-based resources—food banks, housing assistance, transportation services, mental health resources, substance abuse treatment, legal services, and community health workers. APCM recognizes that health is determined by social and economic factors. Your clinic should have a documented list of community partners, a process for assessing patient needs, and a referral workflow.
Element 9: behavioral health & mental health coordination
APCM requires that clinics screen for and coordinate behavioral health and substance use disorders. This doesn’t mean you need to employ psychiatrists; it means you have a documented process for identifying behavioral health needs and referring to or coordinating with behavioral health providers. This might include screening for depression, anxiety, substance use, and domestic violence, with clear workflows for response and referral.
Element 10: consultant & specialist coordination
Your clinic must actively coordinate care with specialists. This means sending clear referral information, receiving specialist recommendations, and integrating specialist guidance into your primary care plan. Instead of sending a referral and never hearing from the specialist again, you’re maintaining an active dialogue. You’re tracking whether the referral was completed, whether recommendations were followed, and what the outcomes were.
Element 11: care plan accessibility & shared decision-making
Beyond just having an electronic care plan, patients and their caregivers should be able to access it, understand it, and contribute to it. The care plan should reflect shared decision-making—the patient’s preferences, values, and goals should be documented. This is about empowering patients, not just imposing a care plan on them. Documentation should show patient engagement in care planning.
Element 12: quality reporting & performance metrics
APCM requires participation in MIPS (Merit-based Incentive Payment System) and the Value in Primary Care value pathway. Your clinic must track and report quality metrics including readmission rates, emergency department utilization, chronic disease management metrics (like HbA1c control for diabetes), preventive service rates, and patient satisfaction. These metrics directly tie to reimbursement—poor performance results in payment adjustments.
Element 13: coordination of care across all settings & transitions
This is the integrative element that ties everything together. Your clinic is responsible for ensuring that care is coordinated across all settings where your patient receives care—primary care, specialists, urgent care, emergency department, hospital, skilled nursing facility, home health, behavioral health, community services. When your patient moves between settings, you’re actively ensuring smooth transitions and continuity.
Why your EHR alone won't cut it
Here’s a hard truth: your EHR was built to support billing and visit documentation. It’s designed to help you code encounters, generate superbills, and maintain a legal record. It was not designed to orchestrate care across multiple providers and settings.
Consider the workflow challenge:
Your patient, Mr. Jones, sees his primary care physician on Monday with uncontrolled hypertension. You adjust his medication. He also has an appointment with a cardiologist on Wednesday, a different provider, different EHR, different network. The cardiologist sees the same uncontrolled hypertension and adjusts his beta blocker. The medication adjustment is never communicated to your clinic until you see Mr. Jones six months later.
Your EHR can’t prevent this. It’s siloed. The cardiologist’s EHR is siloed. They’re not talking.
Or consider this: A patient is discharged from the hospital on Friday evening with a new diagnosis and three medication changes. Your clinic doesn’t receive the discharge summary until Tuesday. By then, the 7-day window for APCM follow-up is already ticking. Your care coordinator manually chases down the paperwork, calls the patient, and plays catch-up, all because discharge notifications aren’t automated.
Or this: Your clinic has identified 50 high-risk patients who should be contacted this month for preventive outreach. Your care coordinator has a list in Excel. She’s responsible for remembering to make those calls, documenting them, and flagging any that require escalation. It’s manual, it’s error-prone, and it doesn’t scale.
Clinics attempting APCM without dedicated care coordination infrastructure will stumble on three fronts:
- Fragmented care plans that don’t reach specialists or post-acute partners
- Manual, reactive processes that miss time-sensitive follow-ups
- Compliance and documentation gaps that create audit risk
What you actually need is a unified care coordination platform that integrates with your EHR and connects to specialists, post-acute providers, and health information exchanges. The platform should automate admission/discharge notifications so your care coordinator gets alerted in real time. It should centralize care plans so specialists and post-acute partners can see and contribute to them. It should track risk-stratified patient cohorts and auto-assign outreach tasks to your care team. It should generate audit-ready documentation for APCM compliance. And critically, it should reduce manual task burden so your care coordinators can focus on high-touch patient engagement, not data entry.
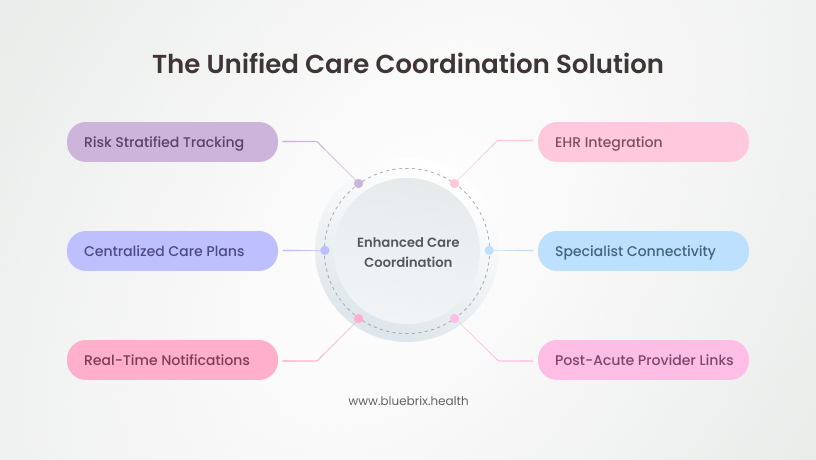
This infrastructure doesn’t exist in your typical EHR. That’s why we built blueBriX – a specialized platform built for care coordination. And frankly, it’s non-negotiable if you’re serious about APCM.
Your roadmap: which payment model fits your clinic?
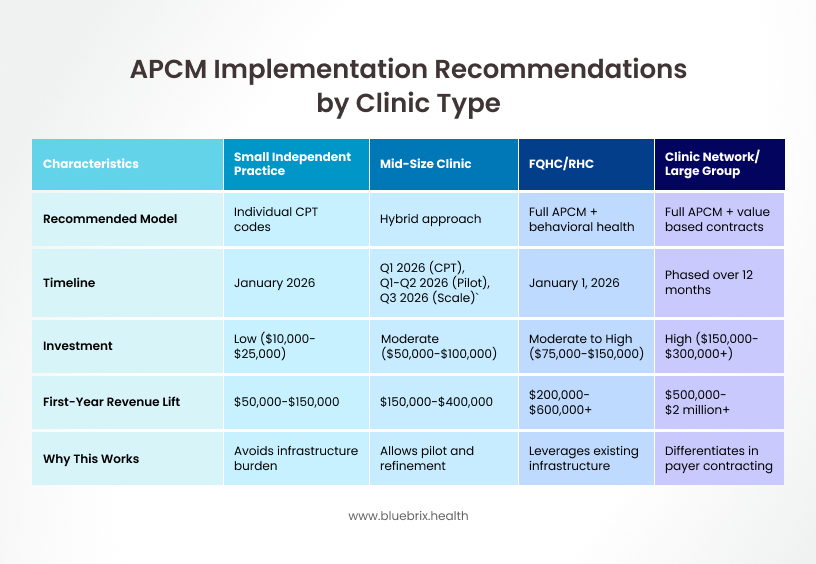
Not every clinic should pursue APCM immediately. Depending on your size, current infrastructure, and risk tolerance, here’s what we recommend:
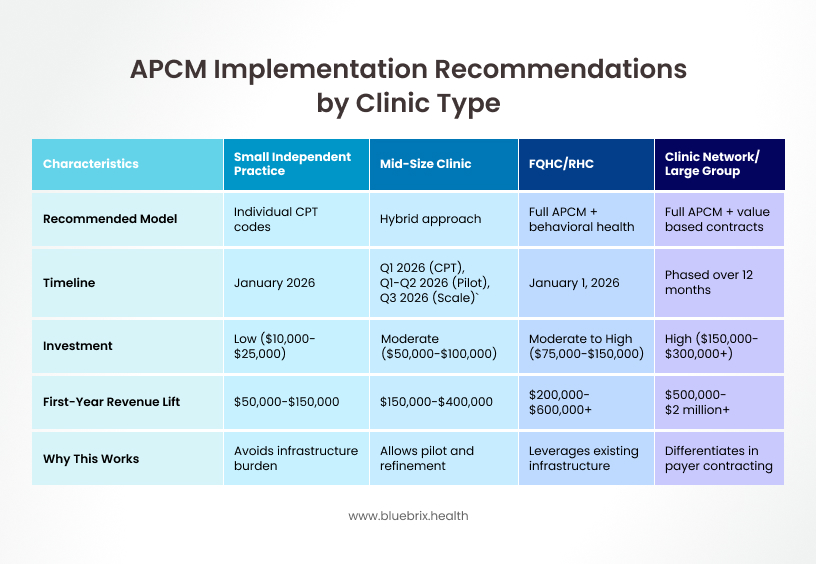
Small independent practice (1–3 providers, under 1,000 patients)
Recommended model: Start with individual CPT codes (Chronic Care Management, Principal Care Management, Remote Patient Monitoring, Remote Therapeutic Monitoring).
Timeline: Begin immediately in January 2026.
Investment: Low. Budget $10,000–$25,000 for billing system setup, minimal technology, and staff training on documentation requirements.
Expected first-year revenue lift: $50,000–$150,000 depending on your patient complexity mix and how many patients you enroll in care management services.
Why This Works: Small practices don’t have the infrastructure burden of APCM’s 13 required elements, but they can still capture meaningful care coordination revenue by billing for existing coordination work. You start documenting care management services you’re already providing, and revenue flows immediately.
Mid-Size Clinic (5–10 providers, 2,000–5,000 patients with some care coordination infrastructure)
Recommended model: Hybrid approach. Start with individual CPT codes for your broader population, then pilot APCM with a focused, high-risk cohort of 100–200 patients.
Timeline: Launch individual CPT codes in Q1 2026. Pilot APCM in Q1–Q2 2026. Scale APCM across your clinic in Q3 2026.
Investment: Moderate. Budget $50,000–$100,000 for a dedicated care coordination platform, extensive staff training, workflow redesign, and potentially 1–2 additional care coordinator FTEs.
Expected first-year revenue lift: $150,000–$400,000 depending on your patient complexity mix, how many patients you enroll in APCM, and how effectively you implement the 13 required elements.
Why this works: Mid-size clinics have the patient volume and complexity to justify APCM investment, but may not want to swing all-in immediately. A phased approach lets you pilot, learn, refine, and then scale. You capture revenue from individual CPT codes immediately while building toward full APCM implementation.
FQHC or RHC with existing care management infrastructure
Recommended model: Full APCM implementation plus integrated behavioral health add-on codes (new in 2026).
Timeline: Immediate launch January 1, 2026.
Investment: Moderate to high. Budget $75,000–$150,000 for care coordination platform, comprehensive staff training, workflow redesign, and coordination with your behavioral health team.
Expected first-year revenue lift: $200,000–$600,000+ depending on your patient volume, complexity, and how many patients you’re able to enroll in APCM and BHI services.
Why this works: FQHCs and RHCs are already operating under value-based payment models and likely have care management infrastructure in place. The unbundling of G0511 into separate, higher-paying codes creates immediate revenue opportunity. APCM allows you to capture even more revenue while providing more structured, comprehensive care. The behavioral health add-ons are particularly relevant given FQHCs’ dual focus on primary care and behavioral health.
Clinic network or large multi-specialty group
Recommended Model: Full APCM across all primary care clinics, with parallel value-based contract negotiations (ACO REACH, Medicare Advantage preferred status, Medicaid managed care partnerships).
Timeline: Phased implementation over 12 months—start with flagship clinics in Q1 2026, roll out to remaining clinics over the year.
Investment: High. Budget $150,000–$300,000+ for enterprise care coordination platform, change management resources, extensive training across multiple locations, and payer contracting support.
Expected first-year revenue lift: $500,000–$2 million+ depending on your primary care network size and how effectively you implement APCM across clinics and leverage it for value-based contracting.
Why this works: Large networks have the scale, complexity, and payer relationships to justify enterprise-level investment. APCM becomes a competitive differentiator in payer contracting—you can demonstrate documented care coordination outcomes, which is increasingly required for preferred status in Medicare Advantage and ACO arrangements. The 12-month rollout allows for systematic implementation, staff training, and payer communication.
Don’t make these five mistakes when scaling care coordination
Most clinics that stumble do so not because the reimbursement is unclear, but because they misjudge the implementation complexity. Here are the five most common mistakes—and how to avoid them:
Mistake 1: treating care coordination as billing automation
Many clinics focus on the billing codes first and care delivery second. They think: “If I document that I did care coordination, I can bill for it.” Wrong. CMS will audit APCM clinics to ensure the 13 required elements are actually delivered. Documentation without delivery is fraud. Start with workflow redesign; billing follows.
Solution:
Design workflows first.
Ask:
- What does 24/7 access actually look like at our clinic?
- How do we systematically identify high-risk patients?
- What does a 7-day post-discharge follow-up workflow require?
Only after you’ve answered these questions should you think about documentation and billing.
Mistake 2: siloed implementation (no specialist coordination)
Clinics often build care coordination workflows that are internal only. They don’t proactively communicate with specialists, don’t track referral responses, and don’t coordinate care transitions with post-acute partners. This breaks at the seams. Your patient is discharged from the hospital, and nobody tells you. A specialist adjusts a medication, and you don’t know. Care coordination is only effective if it’s cross-provider.
Solution: Choose a care coordination platform with built-in specialist communication, referral tracking, and health information exchange integration. Your internal workflows matter, but they’re only half the picture. True care coordination happens at the intersections, between primary care and specialists, between clinic and hospital, between office and post-acute providers.
Mistake 3: underestimating staffing needs
APCM requires dedicated care coordinators. Many clinics try to overlay APCM responsibilities onto existing staff—asking front desk staff to also manage care transitions, expecting clinical staff to also run population health reports. Result: coordinator burnout, missed follow-ups, poor quality.
Solution: Budget conservatively. Allocate 1 full-time care coordinator per 50–75 complex patients. If you have 500 APCM-eligible patients, you need at least 7 coordinators. This isn’t overhead; it’s the operational backbone of APCM. Underinvesting in staffing is the #1 reason APCM implementations fail.
Mistake 4: poor risk stratification
Clinics often enroll all patients or use outdated, unsystematic methods to identify who’s high-risk. This wastes resources. APCM works best for high-complexity, high-utilization patients. Enrolling low-risk patients in APCM dilutes your coordinator’s attention and doesn’t generate proportional value.
Solution: Use evidence-based risk tools. CMS has approved several models; your payer may provide others. Focus on your sickest, most complex cohort first. As you mature, you can expand to moderately complex patients. But start narrow, prove the model works, and then scale.
Mistake 5: treating APCM as revenue, not quality
Some clinics implement APCM primarily to maximize billing. This is shortsighted. CMS will tie APCM reimbursement to quality metrics—readmission rates, HbA1c control, blood pressure control, patient satisfaction. If your quality lags, you face payment adjustments.
Solution:
Design workflows around quality first.
Ask:
- How do we measurably reduce readmissions?
- How do we improve chronic disease management? How do we improve patient satisfaction?
Revenue follows quality. Make quality the north star, and billing becomes straightforward.
A turning point for independent primary care
The broader context is crucial here: CMS’s 2026 care coordination reimbursement is not a one-year provision. It’s part of a decade-long shift toward value-based primary care.
Every major CMS initiative launched or expanded in 2026 – ACO REACH, Medicare Shared Savings Program enhancements, Making Care Primary, Ambulatory Specialty Model – assumes robust care coordination as foundational infrastructure. CMS is essentially saying: “We’re paying for primary care to be the center of the healthcare system, and that requires coordination.”
This has profound implications for independent primary care. For the past five years, primary care margins have been squeezed. Clinics have consolidated under hospital ownership because independent practice became uneconomical. CMS’s 2026 reimbursement increases for care coordination are explicitly designed to reverse this trend to make independent primary care viable again.
Clinics that implement care coordination in 2026 don’t just capture new revenue. They build competitive advantage in payer contracting (Medicare Advantage plans and ACOs actively seek clinics with APCM capabilities). They improve patient outcomes and satisfaction, increasing retention and referral volume. They create documented, measurable evidence of quality that becomes leverage in negotiations. They position themselves as preferred partners for high-risk, high-upside value-based contracts.
The clinics that wait, that treat 2026 as just another year, will watch their peers pull ahead. By 2027 or 2028, when they decide to implement APCM, they’ll be behind the curve: payers will have already identified preferred APCM partners, and the competitive window will have closed.