Redefining compliance
& reporting strategy
Measure visibility
Static reports come too late to fix performance. blueBriX provides live STAR and HEDIS dashboards so teams can spot gaps, track outcomes, and protect incentive programs.
Live tracking
Monitor STAR, HEDIS, and payer-specific KPIs continuously.

Gap identification
See overdue or missed measures early.

Incentive alignment
Tie performance directly to bonuses and quality targets.
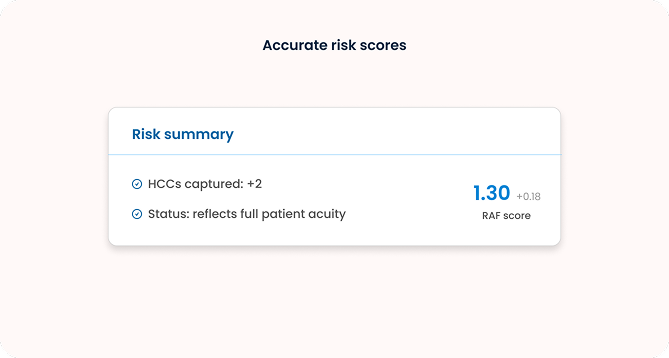
RAF & HCC support
Risk adjustment often gets under-documented. blueBriX provides workflow-level guidance to ensure accurate RAF/HCC capture—protecting reimbursement and reflecting true patient complexity..

Point-of-care guidance
Flag missing documentation in real-time.

Workflow integration
Support clinicians without adding extra steps.

Accurate risk scores
Ensure RAF/HCC reflect full patient acuity.
Compliance simplified
Audits shouldn’t mean last-minute scrambles. blueBriX automatically maintains secure, detailed records so compliance reviews are straightforward.
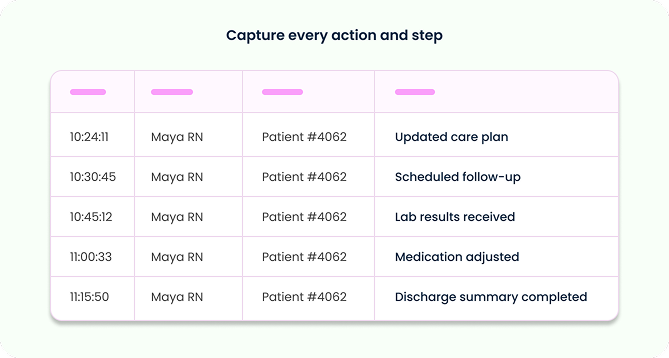

Comprehensive logs
Capture every action and workflow step.

Secure storage
Maintain integrity and compliance readiness.

Audit-ready
Export and share logs easily with CMS or payer reviewers.
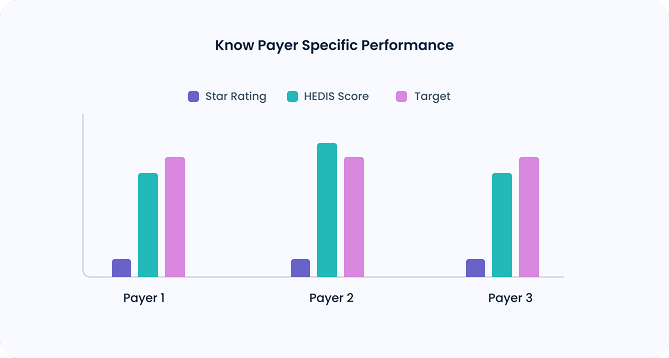
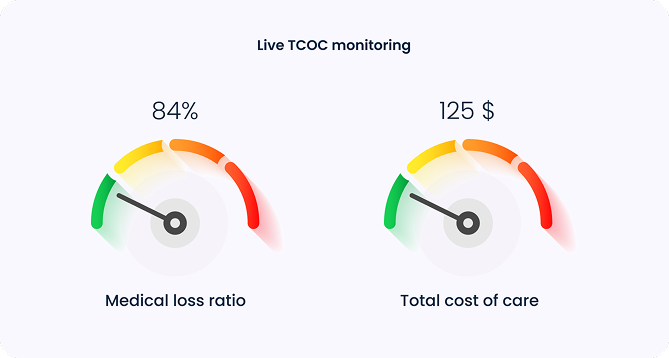
Payer alignment
Different payers measure performance differently. blueBriX delivers contract-specific dashboards so you can manage utilization, costs, and incentive-linked KPIs.
Payer specific Views
See STARs, HEDIS, and custom metrics per payer.
TCOC monitoring
Track medical loss ratio (MLR) and total cost of care.
Custom dashboards
Tailor metrics to contract requirements and VBC programs.




