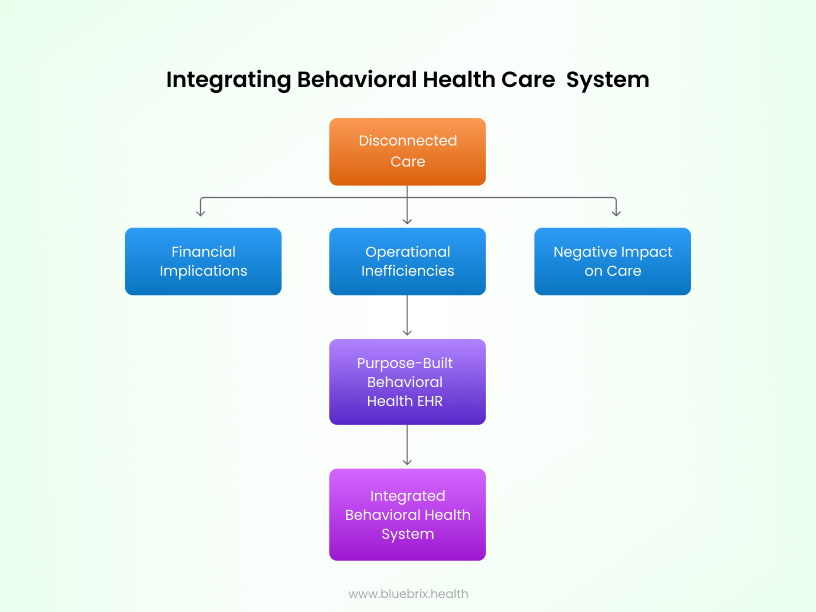
Navigating the fragmented landscape of behavioral healthcare presents challenges that extend beyond visible expenses. Disjointed care pathways often lead to financial waste, operational inefficiencies, and, most critically, compromised patient outcomes due to delays, miscommunication, and inconsistent treatment approaches. In this discussion, we explore these hidden costs and introduce a solution designed to mend fragmentation, streamline workflows, enhance provider communication, and ultimately cultivate a more coordinated and effective patient care experience.
In behavioral health care, fragmented technology is a persistent challenge. Providers often rely on separate systems for clinical notes, scheduling, billing, prescriptions, and lab management. While each system may work independently, the lack of integration creates inefficiencies and hidden costs that can compromise both patient outcomes and the clinic’s financial stability. Care that is not given uniformly can lead to unforeseen and unexpected “hidden” costs, both in terms of the patient’s health outcomes and the patient’s finances. A purpose-built, integrated behavioral health EHR eliminates these silos by unifying patient data and streamlining care coordination. This enables providers to deliver more informed, effective care while reducing the risk of costly errors that could impact both patients and the clinic.
Financial Consequences of Disconnected Behavioral Health Systems
When behavioral health organizations rely on fragmented technology, the financial repercussions are substantial and far-reaching:
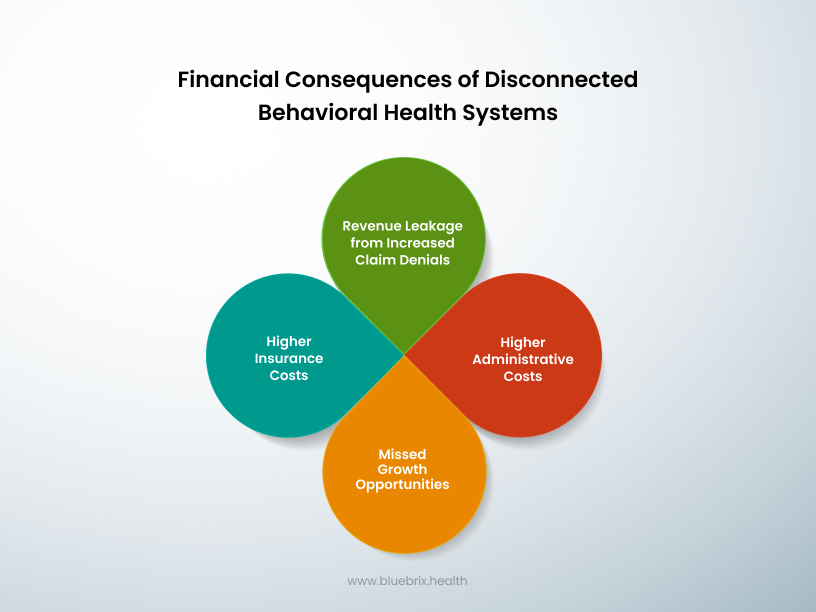
- Revenue Leakage from Increased Claim Denials: Fragmented systems contribute to higher claim denial rates, with around 79% of behavioral health organizations reporting a rise in denials due to incomplete or inconsistent patient data. This not only delays reimbursements but also results in revenue losses that can significantly impact the organization’s financial stability.
- Higher Administrative Costs: Disconnected systems lead to redundant tasks, such as manual reconciliations and duplicate data entry, which drive up operational expenses. The need for ongoing system maintenance and error correction further strains financial resources.
- Missed Growth Opportunities: When staff are burdened with inefficient administrative processes, fewer resources are available for patient-centric initiatives or strategic growth efforts. This inefficiency stifles innovation and limits the organization’s potential for expansion.
- Higher Insurance Costs: Disconnected systems can lead to higher insurance premiums as insurers cover the costs of inefficient care. This can make mental health services less accessible to those who need them.
Operational Burdens on Behavioral Health Staff
Fragmented technology doesn’t just affect the bottom line—it also creates significant operational challenges that burden behavioral health staff:
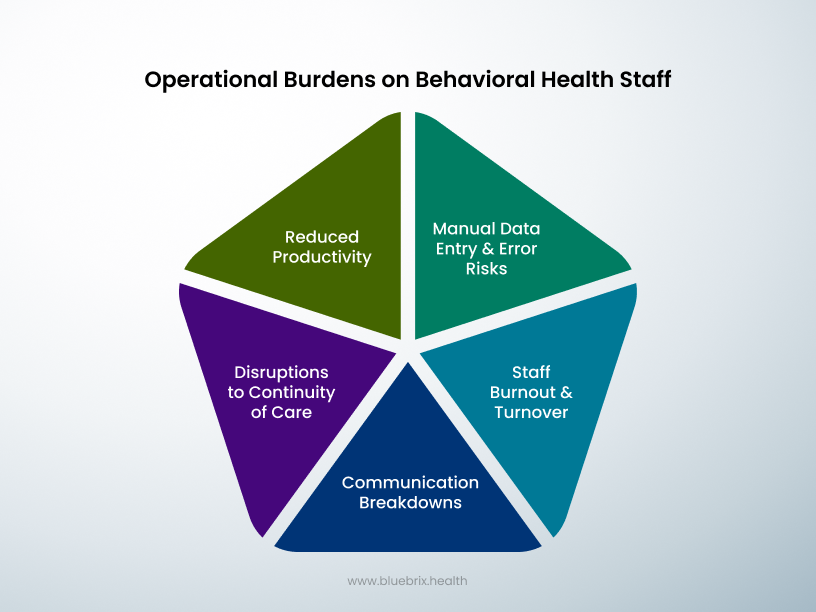
- Reduced Productivity: Clinicians and therapists spend nearly 35% of their time on documentation and repetitive administrative tasks, which takes them away from direct patient care. This inefficiency reduces overall productivity and limits the time available for meaningful therapeutic interactions.
- Manual Data Entry and Error Risks: With disconnected systems, staff often have to re-enter data manually or transfer information between platforms. This not only wastes time but also increases the risk of errors and data inconsistencies, which can compromise patient safety and treatment accuracy.
- Staff Burnout and Turnover: Inefficient EHR systems are a major source of frustration for behavioral health professionals. In fact, 77% of providers report feeling overwhelmed by disjointed technology, which contributes to burnout. This, in turn, leads to higher turnover rates and additional recruitment costs, further straining the organization’s resources.
- Communication Breakdowns: Inefficient communication between different care providers can result in miscommunication and errors. This can lead to delays in treatment, clinical errors, and suboptimal patient outcomes.
- Disruptions to Continuity of Care: Frequent staff turnover and disjointed care can disrupt the continuity of care for patients. This instability can hinder patient engagement and adherence to treatment plans, negatively impacting overall outcomes.
Negative Impact on Patient Care in Behavioral Health
Disconnected systems directly affect the quality of care and patient outcomes in several ways:
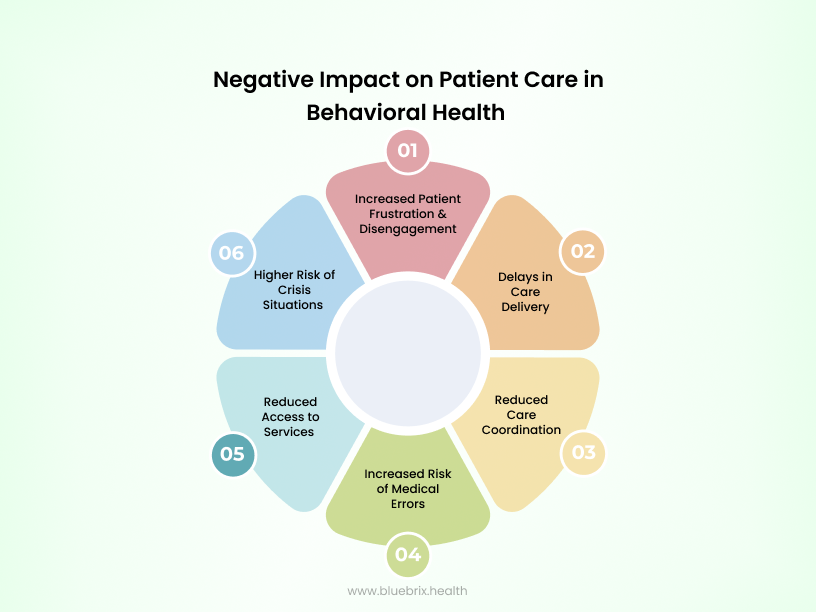
- Delays in Care Delivery: When patient data is scattered across multiple systems, it becomes difficult for behavioral health providers to access critical information quickly. This fragmentation leads to delays in diagnosis and treatment, potentially worsening patient conditions and reducing treatment effectiveness. For example, a study found that patients with severe mental illness experienced an average delay of 8-10 years from the onset of symptoms to receiving appropriate treatment.
- Reduced Care Coordination: Lack of interoperability results in fragmented communication between therapists, psychiatrists, and other care providers. This leads to redundant assessments and inconsistent treatment plans, diminishing the continuity and effectiveness of care. This inconsistency can result in medication errors and suboptimal treatment outcomes. According to the CDC, social isolation and loneliness, which can be exacerbated by fragmented care, increase the risk of premature death by 29% and 26%, respectively.
- Reduced Access to Services: Patients in disconnected systems often face barriers to accessing necessary services, particularly in rural or underserved areas. Research indicates that people living in rural areas are 20% less likely to receive mental health services compared to those in urban areas.
- Increased Patient Frustration and Disengagement: Navigating a disjointed system can be frustrating for patients, leading to disengagement from treatment. This can result in poorer health outcomes and increased risk of relapse. A survey found that 40% of patients with mental health conditions reported feeling frustrated with the complexity of accessing care.
- Increased Risk of Medical Errors: Disjointed systems contribute to communication gaps and incomplete patient records, which heighten the risk of preventable mistakes. Studies indicate that fragmented behavioral health systems contribute to medication errors, missed follow-ups, and gaps in crisis intervention, jeopardizing patient safety.
- Higher Risk of Crisis Situations: Without coordinated care, patients are at a higher risk of experiencing crises, such as severe mental health episodes or hospitalizations. Studies show that individuals with serious mental illness are 2.5 times more likely to visit the emergency room compared to the general population.
Disconnected behavioral health systems don’t just cause operational headaches—they have far-reaching consequences that can seriously impact financial performance, staff well-being, and patient care.
The Solution? Integrated Behavioral Health Systems
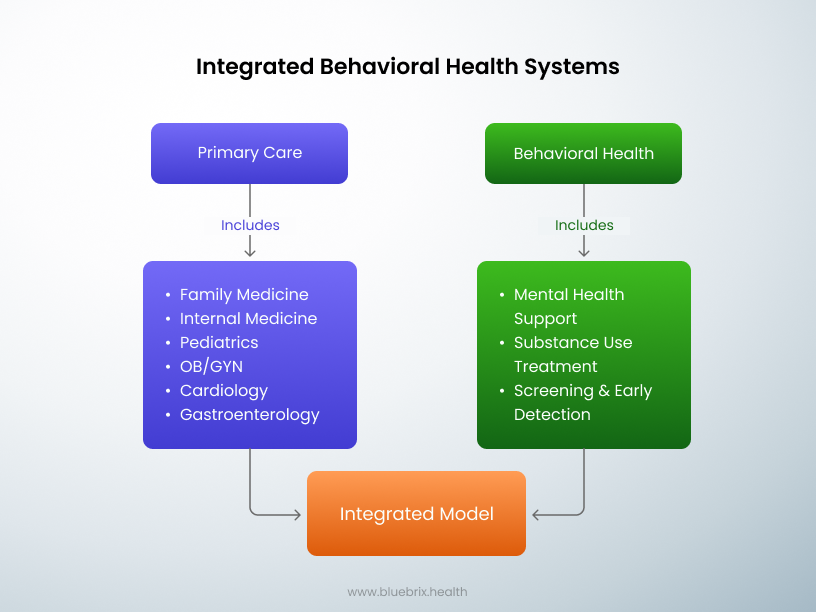
Embracing Integrated Behavioral Health isn’t just a game-changer—it’s a necessity. It streamlines operations, slashes costs, and transforms the experience for both staff and patients. With everything centralized, care becomes more coordinated, efficient, and effective.
Benefits of Integrated Behavioral Health Systems
In the section preceding this, we went over how a lack of integrated systems can negatively impact a provider’s ability to administer effective treatment and how it can negatively impact the patient from both a financial perspective and from a health outcome perspective. In this section, we are going to explore how and why integrated labs and pharmacy systems benefit behavioral care:
- Enhance Access: Studies show that patients using pharmacies integrated within community mental health centers (CMHCs) exhibit significantly higher medication adherence rates compared to those using external pharmacies. This is due to reduced physical barriers and immediate access to medications.
- Higher Adherence Rates: Studies have shown that patients using integrated pharmacies demonstrate adherence rates of around 96%, significantly higher than those using external community pharmacies. This high level of adherence correlates with lower hospitalization rates (40% reduction) and decreased emergency department visits (18% reduction).
- Better Outcomes: Improved adherence leads to lower hospitalization rates and emergency department (ED) visits, reducing overall healthcare costs by an estimated $700,000 per 1,000 patients annually.
- Pharmacist-Led Interventions: Pharmacists embedded in behavioral health teams can adjust medications, interpret lab results, and manage complex pharmacologic therapies for conditions like depression, anxiety, PTSD, and substance use disorders
- Lab Integration for Monitoring: Behavioral health treatments often require routine lab monitoring (e.g., for antipsychotic medications or long acting injectables). Integrated labs ensure timely testing and results interpretation, reducing delays in care.
- Hybrid Pharmacy Models: These models synchronize refills, package medications together, and deliver them efficiently. They also use tools like Medherent to improve medication adherence, leading to fewer hospitalizations and ED visits.
- Reduced Healthcare Costs: Integrated systems lower costs by preventing unnecessary hospitalizations and ED visits. For example, integrated CMHC pharmacies save $58 per member per month on average.
- Efficient Resource Use: By centralizing lab and pharmacy services, facilities save valuable staff time (up to 7.6 hours per patient per month), which is critical during staffing shortages.
- Support for Vulnerable Populations: Patients with serious mental illnesses (SMIs) often have complex medication regimens requiring close monitoring. Integrated systems ensure timely interventions tailored to individual needs.
Connecting the Dots: A Purpose-Built Behavioral Health EHR
While integrating systems is essential, the effectiveness of this integration depends significantly on the core platform managing it—namely, the Electronic Health Record (EHR) system. A purpose-built behavioral health EHR designed specifically for behavioral health care is critical in addressing the unique challenges of this field.
Here’s how a tailored EHR can help:
Seamless Data Integration for Whole Person Care
According to a report by MACPAC, EHRs can promote coordinated care by allowing clinicians to readily update patient health information and distribute that information to authorized providers across different settings. A purpose-built behavioural health EHR enables seamless integration with lab and pharmacy systems, consolidating all patient information into a unified platform. This ensures that providers have real-time access to lab results, medication history, and clinical notes, allowing for informed, timely, and accurate care decisions. By eliminating data silos, a specialized EHR supports whole person care, reducing the risks of fragmented care and missed information.
Improved Care Coordination and Continuity
Behavioral health often involves multiple providers, including psychiatrists, therapists, and primary care physicians. An EHR designed for behavioral health streamlines communication and coordination across these teams. It allows secure sharing of patient data, ensuring that all care team members remain aligned, which reduces redundancies, prevents conflicting treatments, and promotes continuity of care.
Enhanced Clinical Decision Support
Purpose-built EHRs include clinical decision support (CDS) tools tailored for behavioral health. These tools offer real-time alerts and recommendations related to medication interactions, patient safety risks, and evidence-based treatment protocols. This ensures that providers can make well-informed decisions, reducing the likelihood of medication errors and adverse events.
Improved Clinician Time Management
EHRs streamline data collection and reduce manual documentation, freeing up clinicians to focus more on patient care. Behavioral health providers using purpose-built behavioral health EHRs report spending more time reviewing client progress, enhancing treatment quality and fidelity.
Support for Evidence-Based Practices
EHRs provide tools for tracking adherence to evidence-based care models, enabling providers to implement standardized assessments and interventions efficiently. This improves service quality and patient satisfaction.
Simplified Regulatory Compliance and Documentation
Behavioral health care is subject to specific regulations and reporting requirements. A customizable EHR automates compliance processes, streamlining the documentation of patient encounters, treatment plans, and outcomes. This reduces the administrative burden on staff, minimizing the risk of errors while ensuring adherence to regulatory standards.
Improved Patient Engagement and Outcomes
Modern, purpose-built behavioral health EHRs often include patient portals and engagement features, enabling individuals to access their health information, medication instructions, and appointment schedules. This fosters transparency, improves medication adherence, and empowers patients to take an active role in their care, ultimately contributing to better health outcomes. A Journal of Medical Internet Research study found that patient portals boost satisfaction by 70% and cut chronic disease readmissions by 30%. EHR-integrated engagement tools also reduce missed appointments by 23%, improving efficiency and resource use.
Cost Savings and Operational Efficiency
Purpose-built behavioral health EHRs deliver significant cost savings and efficiency gains. Technology-enabled behavioral health integration (tBHI) programs have reduced emergency department visits by 34%, lowering expensive acute care costs. Patients in these programs also show improved mental health outcomes, reducing the need for costly interventions. Integrated EHR systems streamline billing, cutting denial rates to less than 1%, and behavioral health homes using EHRs report 26% lower per-member-per-month (PMPM) costs. Additionally, EHRs boost administrative efficiency, with timely clinical note submissions rising from 76% to 96%, enhancing workflows and reducing delays. These findings underscore the financial and operational value of EHR adoption in behavioral health.
The Bottom Line
Without a purpose-built behavioral health EHRs at the core, even the best integrated systems cannot fully address the complexities of behavioral health care. An EHR specifically designed for this field offers the data unification, care coordination, and clinical support necessary to deliver high-quality, cost-effective, and patient-centric care.
If you’re looking for a comprehensive purpose-built behavioral health EHR solution that integrates seamlessly with labs, pharmacy systems, medical devices and other digital health systems, blueBriX’s purpose-built healthcare platforms tailored for behavioral health providers should be on top of your consideration list. Contact us to learn more about how our solutions can help you enhance patient care and streamline your behavioral health operations better than other generic EHRs. blueBriX has been an industry leader in the healthcare software field for nearly two decades and we would be happy to assist you, as we have with our hundreds of satisfied clients.