Healthcare, like many other industries, is going through a transformation as technology becomes more affordable and big data becomes more useful. As a result, this healthcare IT crossover has led to several relatively new regulations that force providers to work closely with their associated IT teams. Many are struggling with the transition.
If you’re in the healthcare industry, you’re likely familiar with MACRA – or the Medicare Access and CHIP Reauthorization Act of 2015 – that combines various incentive programs into one. This compilation is the “Merit Based Incentive Payment System,” which emphasizes better quality of care standards for practices using certified EHR technology.
The good news is, MIPS offers physicians much-needed flexibility by relaxing some of the previous requirements for certification and reporting measures. Policymakers took industry feedback into account when creating the regulation.
The new rule aims to move our healthcare system from a fee-for-service approach to one centered on value-based care and aimed at improving patient health, a recent Healthcare IT News piece mentioned.
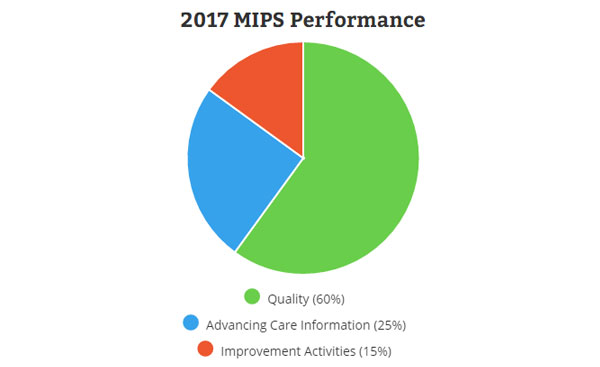
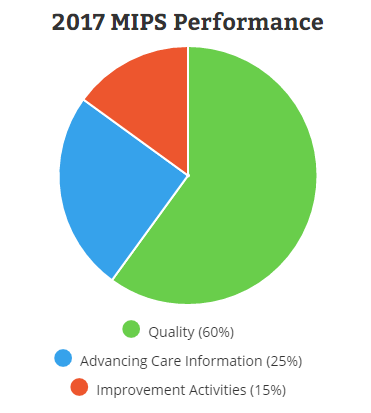
MIPS incentivizes providers to use a 2015 certified EHR – but does not mandate it. This, in theory, encourages greater interoperability and patient access to data. Performance measures fall into three main categories – ‘quality’, ‘advancing care information’ and ‘improvement activities’. There is a fourth – ‘cost’ – but CMS will reinstate it in 2018.
Each measure is broken down into various sections, but for this blog, we’ll just run through a summary of each.
Quality
The ‘Quality’ performance category within MIPS assesses health process and outcomes through various measures. MIPS-eligible clinicians should demonstrate improved quality above the baseline level or established performance benchmark. The performance benchmark is based on historical or performance-period data (or potentially based on 2017 performance data for quality measures with no historic benchmark).
For this transition year, CMS’ data validation process for the ‘Quality’ performance category will apply to claims and registry submissions to validate whether they fulfill all applicable measures when submitting fewer than six. The validation process also requires that a provider submit the necessary outcome measures or other high priority measures.
Advancing Care Information
The MIPS ‘Advancing Care Information’, or ‘ACI’, performance category replaces the Medicare EHR Incentive Program for eligible professionals, also known as ‘Meaningful Use’. ACI promotes patient engagement and the electronic exchange of information using certified EHR technology.
Improvement Activities
The ‘Improvement Activities’ (IA) performance category assesses how much providers participate in activities that make clinical practice better. For example, activities related to ongoing care coordination, clinician and patient shared decision making, regular use of patient safety practices and expanding practice access.
We’re 8 months in, but you might be wondering about the reporting period for 2017.
Providers can submit a yearly report or a report that covers any 3 consecutive months. Since the final rule and benchmarks for the measures under various incentive programs arrived mid year, it likely makes sense to report on a 3 month period (perhaps October thru December of this year, as that would allow for additional training and implementation time).
MIPS relies on the synchronization of technology and healthcare. EHR providers are perfectly suited to help providers navigate the changes before the October reporting period.
In fact, we’re here to help! We’re offering training to our customers who need some help navigation MIPS. Shoot us a message and we can get started!